Review Article - (2023) Volume 14, Issue 6
Abstract
Hyperlipidemia is a condition of having abnormalities in plasma lipids. According to the surveys done in India, urban populations are more affected by higher cholesterol levels than rural populations. Hyperlipidemia is mainly caused due to lifestyle, lack of exercise, and high-fat diet intake. It is classified based on two factors. They are on the basis of lipid type i.e., hypercholesteremia and hypertriglyceridemia, and on the basis of causing factors i.e., familial and acquired factors. In general, Hyperlipidemia can be treated by lifestyle and dietary changes. If the levels are high, medication is needed (Ayurvedic or Allopathic). The most commonly used drugs are statins and fibrates. Inducing agents are used to increase plasma lipids. These are used in in vitro and in vivo experiments mostly used inducing agents are Triton X100, Triton WR 1339, and methionine. As hyperlipidemia can be cured by switching to a healthy diet, natural home remedies can show a high impact.
Keywords
Hyperlipidemia, Lipoproteins, Chylomicrons, Triton X100, Methionine
Abbreviations
HDL: High-Density Lipoprotein; LDL: Low-Density Lipoprotein; VLDL: Very Low-Density Lipoprotein; ApoB: Apoprotein B; TG: Triglyceride; IP: Intra Peritoneal; IV: Intravenous; ROA: Route of Administration; IDL: Intermediate-Density Lipoprotein; Apo-2: Apoprotein-2; CHD: Chronic Heart Disease; TLC: Therapeutic Lifestyle Changes; FA: Fatty Acids; PPAR: Peroxisome Proliferator-Activation Receptor; NPCIL-1: Niemann-Pick C1-Like 1 protein; ACATI: Acetyl-coA Cholesterol Acyl Transferase Inhibitor; MTP: Microsomal Triglyceride transfer Protein; CETP: Cholesterol Esterase Transfer Proteins; LS: Lanosterol Synthase; FDA: Food and Drug Administration; ApoC-3: Apoprotein C3; ApoA1: Apoprotein A1; ApoA4: Apoprotein A4; GST: Glutathione S-Transferase; SOD: Superoxide Dismutase; GSH: Glutamyl- L-cysteinyl-glycine; CAT: Catalase; PX: Peroxidase
Introduction
Hyperlipidemia is a health condition that results in the chronic elevation of cholesterol, cholesterol ester, triglycerides, and phospholipids in the blood (Shattat GF, 2015; Mishra PR, et al., 2011; Jeyabalan S and Palayan M, 2009). Due to this abnormal elevation of lipid contents in blood and it will get deposited in the walls of arteries, the liver, and other organs. This acts as a precursor for many hazardous health diseases such as Atherosclerosis, heart attacks, strokes, etc., (Ezeh KJ and Ezeudemba O, 2021; Altmann SW, et al., 2004). Hyperlipidemia is liable for most cardiovascular diseases (Brouwers MC, et al., 2012). It is estimated that this will become the major cause of the increase in mortality rate due to hyperlipidemia in the coming years (Shattat GF, 2015; Mishra PR, et al., 2011).
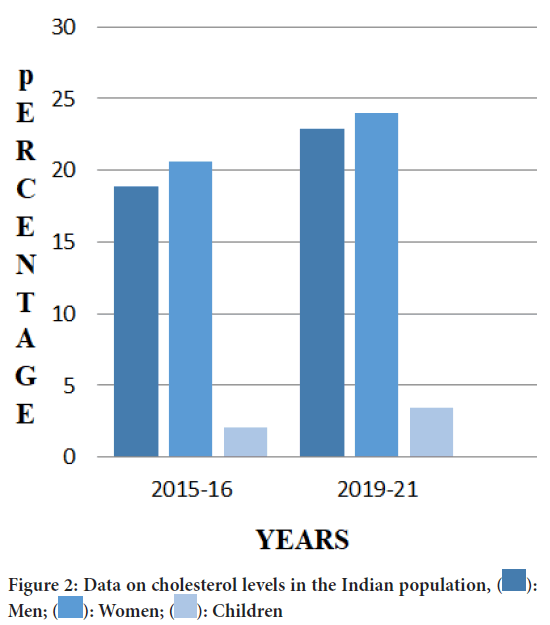
Overall deaths due to elevated levels of cholesterol are found to be 2.6 million deaths and 29.7 million disabilities (Noubiap JJ, et al., 2015; Mendis S, et al., 2011). The food source of cholesterol from high-fat dairy products like milk, cream, yogurt, butter and ghee, etc., Liver in our body also produces and stores some amount of cholesterol. On average estimation, our liver can produce 80% of cholesterol (Mumthaj P, et al., 2021; Singh R and Nain S, 2018; DuBroff R and de Lorgeril M, 2015) (Figure 1).
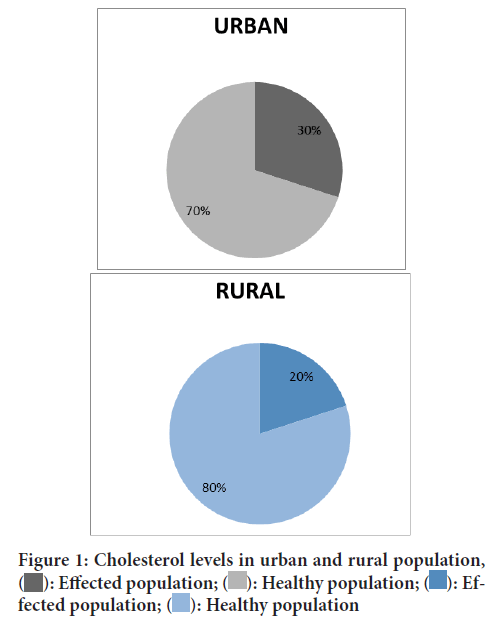
Figure 1: Cholesterol levels in urban and rural population,  : Effected population;
: Effected population;  : Healthy population;
: Healthy population;  : Effected population;
: Effected population;  : Healthy population
: Healthy population
The above pie chart shows the data of urban and rural population that is 30% and 20% suffering from hyperlipidemia in India (Gupta R, et al., 2017).
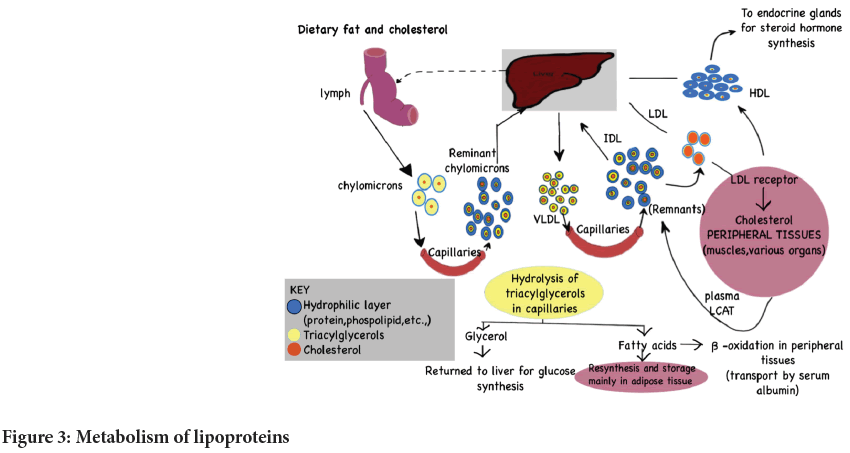
Cholesterol includes Low-Density Lipoproteins (LDL), High-Density Lipoproteins (HDL). LDL is the bad cholesterol that leads to a disorder such as strokes, carotid artery disease, and peripheral arterial disease whereas, HDL is good cholesterol, as it eliminates LDL from the body. Any deviation in these levels results in hyperlipidemia (Mumthaj P, et al., 2021). Many hormones and steroids are produced from cholesterol (Table 1 and Figure 2).
| Lipoproteins | Normal range | Risk condition |
|---|---|---|
| LDL | Under 100 mg/dl | 160 and high |
| HDL | Greater than 60 mg/dl | Under 40-50 mg/dl |
| VLDL | 2 and 30 mg/dl | Above 30 mg/dl |
| Triglycerides | Less than 150 mg/dl | Above 200 mg/dl |
| Total | Under 200 mg/dl | 240 mg/dl and higher |
Table 1: Normal and risk range of cholesterol in human body (Mumthaj P, et al., 2021)
Figure 2: Data on cholesterol levels in the Indian population, : Men;
: Men;  : Women;
: Women;  : Children
: Children
This bar graph clearly shows the rise in cholesterol levels in the Indian population. This data is from the years 2015-2016 and 2019-2021. This is mainly due to lack of physical exercise, genetical inheritance, and improper diet (Pandey G, 2022).
Literature Review
Hyperlipidemia is classified based on 2 factors (Joseph D, 2011). They are:
On the basis of lipid type
Hypercholesterolemia: Hypercholesterolemia is described as high levels of cholesterol in the blood. It indicates the blood serum cholesterol levels of 200 mg/dl or more in blood serum levels. Many atherosclerosis and atherosclerosis conditions such as ischemic cerebrovascular disease, coronary heart diseases, etc., are caused by hypercholesterolemia. There are mainly two types of causes. They are primary causes and secondary causes. The primary causes include environmental causes such as obesity, dietary choices, and genetic factors whereas secondary factors include diabetes mellitus, kidney diseases, hypothyroidism, Cushing syndrome, family history, less physical activity, etc., (Pattis P and Wiedermann CJ, 2008).
Hypertriglyceridemia: It is described as high levels of triglycerides in the blood. HTG is classified based on TG levels:
• Mild TG level (150-199 mg/dl)
• High TG levels (200-499 mg/dl)
• Very high>500 mg/dl
The main reasons for HTG are genetic factors and elevated levels of triglycerides. The other causes include medical conditions (Karachi H, et al., 2022).
On the basis of causing factor (Mumthaj P, et al., 2021)
Hereditary factors: It is a condition that increases the levels of LDL that is passed down across families.
Acquired factors: It is a condition of abnormal elevation of lipids including triglycerides and cholesterol in the blood due to a sedentary lifestyle and unbalanced diet.
Classification of lipoproteins
Lipoproteins are large molecules made of lipids and proteins. They are used to make lipids and proteins compatible with water. Lipids are made up of different types of molecules. Some of these molecules are made up of lipids and other types of molecules.
Lipoproteins are classified as Chylomicrons, Very Low-Density Lipoprotein, Intermediate Density Lipoprotein, High-Density Lipoprotein, and Low-Density Lipoprotein (Sharma A, et al., 2019).
Chylomicrons (CM): Chylomicrons are large particles that transport dietary lipids from the intestine to the bloodstream, where they are broken down into smaller and denser Intermediate-Density Lipoprotein (IDL). They have a variety of apolipoproteins attached, including A-I, A-II, A-IV, B-48, C-I, C-II, C-III, and E. Very Low-Density Lipoprotein (VLDL) particles are primarily formed in the liver, but also in the intestine to a lesser degree (Sundaram M and Yao Z, 2010).
Very Low-Density Lipoproteins (VLDL): Very Low-Density Lipoproteins (VLDLs) are smaller particles than chylomicrons and triglycerides, and are secreted from the liver. VLDLs transport cholesterol from the liver to organs and tissues in the body. They are composed of a mixture of cholesterol and triglycerides (Sundaram M and Yao Z, 2010).
Intermediate Low-Density Lipoproteins (ILDL): The lysis of VLDL particles by lipase enzymes in the capillaries of adipose tissue and muscle results in Intermediate-Density Lipoprotein.
High-Density Lipoproteins (HDL): High-Density Lipoproteins (HDL) are commonly referred to as “good cholesterol”. They are synthesized in the liver and carry cholesterol and other lipids from tissues back to the liver for degradation. HDL also plays an important role in protecting against atherosclerosis (Ridker PM, et al., 2010).
Metabolism of lipoproteins
Intake of high dietary fat and cholesterol leads to the deposition of fat in the liver lymph (Figure 3). Chylomicrons are formed in the intestine as it enters the liver through capillaries. These chylomicrons enter into the capillaries and form remnant chylomicrons and enter into the liver and form VLDL these enter into the capillaries and form remnants and IDL (Intermediate Density Lipoproteins) then the remnant convert into LDL (Low-Density Lipoproteins) this LDL binds to the LDL receptor and convert into cholesterol this form HDL (High-Density Lipoproteins) and passes to endocrine glands for steroid hormone synthesis. Cholesterol in the peripheral tissue from remnant through plasma LCAT (Lecithin Cholesterol Acyltransferase, which is an enzyme that converts free cholesterol into cholesteryl ester) and gets converted into LDL and HDL. Triacylglycerols go through hydrolysis in capillaries and form glycerol and fatty acid. Glycerol returns to the liver for glucose synthesis. Some of the fatty acids get resynthesis and are stored mainly in adipose tissue and the remaining fatty acids go through beta-oxidation in the peripheral tissue and are transported by serum albumin.
Figure 3: Metabolism of lipoproteins
Pathogenesis
The pathogenesis of hyperlipidemia begins when blood monocytes and platelets attach to a damaged vessel wall, the release of mediators such as platelet-derived growth factors stimulate the growth of smooth cells in the intimal and medial lining of the vessel, as well as collagen synthesis, cholesterol uptake, and plaque formation. Plaque rupture can lead to acute syndromes such as unstable angina, myocardial infarction, and sudden cardiac death (Mumthaj P, et al., 2021; Murphy SL, et al., 2013).
Symptoms
Atherosclerosis: It is a condition in which the accumulation of lipids in the walls of the arteries. It leads to insufficient blood and oxygen supply to the heart.
Coronary artery diseases: It is a condition in which the accumulation of lipids in the walls of the arteries which leads to the narrowing of the arteries.
Myocardial infraction: It is a condition in which there is a decrease in oxygen supply to the heart. This is due to the accumulation of lipids.
Ischemic stroke: It is a condition due to the blockage of the artery.
Vascular diseases: It blocks the blood flow in the arteries or veins.
High blood pressure: It is a condition where cholesterol gets deposited in the walls of the arteries which leads to the narrowing of the arteries.
Pancreatitis: It is a condition in which large triglycerides-rich lipoproteins particles primary chylomicron; prevent capillary circulation and causes ischemic damage to the pancreatic acinar (Kumar G, et al., 2013).
Causes
• The primary reason for hyperlipidemia is a defect in lipid metabolism. It effects by the defect of lipoprotein lipase activity and the absence of Apo protein C-11.
• The secondary cause of hyperlipidemia includes genetic abnormalities and environmental factors which includes-
• Lifestyle and exercise
• High-fat diet intake.
• Low-Density Lipoprotein plays an important role in maintaining the hepatic uptake of Low-Density Lipoprotein from plasma mutation in the Low-Density Lipoprotein receptor causes familial hypercholesterinemia.
• Decrease LDL receptor and increased Apo B.
• Decrease in the level of Low-Density Lipoprotein receptors is responsible for decreased clearance of Apo B will deposit in the body.
• Defect in Apo 2-synthesis.
• Increase in Very Low-Density Lipoprotein and decrease in excretion.
• Apo cl accumulated in the plasma leading to an increase in Apomediated inhibition of Low-Density Lipoprotein and triglycerides hydrolysis (Nirosha K, et al., 2014; Millar JS, et al., 2005; Dhingra S and Bansal MP, 2005).
Risk factors
Risk factors of hyperlipidemia are of two types-
1. Non modified risk factors include
• Age, gender and genetics
• Chronic diseases
2. Modified risk factor includes
• Medications
• Nutrition
• Physical inactivity (Nouh F, et al., 2018)
Diagnosis
Hyperlipidemia can be detected with a blood test called a lipid profile. This test checks for LDL, HDL, VLDL, and Triglyceride levels in the blood. Regular testing is recommended to diagnose hyperlipidemia (Cunningham AB, 1988).
Preventive measures
To lower fatty acid and cholesterol levels, adopt the following diet:
• Increase intake of foods high in soluble fiber such as oats, beans, and certain fruits.
• Eat pears, apples, bananas, etc.
• Consume fish twice a week (Verma N, 2016).
Dietary changes: Dietary changes include-
• Oatmeal-LDL is reduced by 12%-24%.
• Orange juice-Lowers cholesterol levels in the blood.
• Coriander seeds-Lower triglyceride and cholesterol levels.
• Soybeans, honey and fish oil-Lowers the levels of triglycerides
• Brown rice, brinjal, coconut oil, turmeric-Lower the levels of LDL cholesterol, improves the LDL/HDL ratio and raises HDL (Verma N, 2016).
Treatment
Many lipid-lowering drugs are marketed to treat hyperlipidemia. A drug project suggests that drugs used to prevent myocardial infarction are relatively ineffective in existing CHD patients (Russell DW, 2003; Edeoga HO, et al., 2005).
Elevated LDL, presence of risk factors, and documented CHD should qualify drug therapy development along with TLC. Current lipid-lowering drugs include statins, ezetimibe, bile acid sequestrates or bile-binding resins, niacin, fabric acid derivatives, and plant sterols. If dietary changes prove inadequate, medications specifically designed to lower blood cholesterol levels may be prescribed (Safeer RS and laCivita CL, 2000).
Fibrates (Fabric acid derivatives): Fibrates, which include clofibrate, gemfibrozil, fenofibrate, and bezafibrate, are a commonly used class of antihyperlipidemic agents that result in a significant decrease in plasma triglycerides and a modest decrease in LDL sterols. HDL cholesterol levels rise gradually. Angiographic experiments revealed that fibrates play the most important role in slowing the progression of coronary atherosclerosis and reducing the occurrence of coronary artery disease.
Data from rodent and human studies suggest four major fibrate mechanisms:
Lipid lipolysis stimulation: Fibrates primarily act as ligands for the PPAR- nuclear transcription receptor. They increase the expression of lipoprotein lipase, Apo, and decrease the expression of Apo C-III, a lipolysis inhibitor. Fibrates also increased HDL cholesterol levels by increasing the expression of Apo AI and Apo AII (Elmore S, 2007).
Increasing hepatic Fatty Acids (FA) uptake: While decreasing hepatic triglycerides production Fibrates promote the formation of fatty acid transport protein and acyl-CoA synthetize, which contribute to increased fatty acid uptake by the liver and a lower availability of fatty acids for triglyceride formation (Keshetty V, et al., 2009).
Increase LDL particle removal: Fibrates appear to increase LDL catabolism via the receptor-mediated pathway, LDL particles became larger and more lipid-rich, and thus had a higher affinity for receptors (da Rocha JT, et al., 2009).
High-density lipoprotein formation: It is accelerated and reverse cholesterol transport is stimulated. Fibrates increase Apo A-1 formation contributing to increase the liver, plasma concentrations of Apo A4, HDL- cholesterol and a more effective reverse cholesterol transport (Girija K and Lakshman K, 2011).
Nicotinic acid derivative (niacin): Niacin, a water-soluble B vitamin, was the earliest lipid-lowering agent used to treat hyperlipidemia and has been shown to reduce cardiovascular morbidity and all-cause mortality. Reduces Total Cholesterol, LDL Cholesterol, and Triglycerides (Irudayaraj SS, et al., 2013).
Niacin inhibits hormone-sensitive lipase and reduces lipid dissolution of triglycerides, the major producers of circulating free fatty acids. For these normally circulating fatty acids, the liver plays an important role in the formation of triacylglycerol. Niacin, therefore, inhibits the secretion of VLDL and reduces the production of LDL (Ragheb A, et al., 2011).
Treatment with niacin has been plagued by low patient compliance. The most common side effects are severe skin redness, itching, headache, and in some patient’s nausea and abdominal discomfort, affecting more than three of quarters of patients. Niacin also increases liver enzymes (Safeer RS and laCivita CL, 2000).
Selective cholesterol absorption inhibitor (ezetimibe): The discovery and development of ezetimibe, the first in a family of drugs that inhibit intestinal absorption of plant sterols and cholesterol, has improved the treatment of hypercholesterolemia. Inhibits the absorption of sterols from the small intestine and does not affect plasma levels of vitamins A, D, E, K.Ezetimibe selectively inhibits cholesterol absorption in the small intestine and reduces cholesterol delivery from the intestine to the liver by blocking the human sterol transport protein Niemann-Pick C1-Like 1 Protein (NPC1L1). This increases the clearance of sterols from the bloodstream (Carvalho FS, et al., 2014).
Ezetimibe is generally a well-tolerated drug. The most common side effects are headache, abdominal pain, and diarrhea. Ezetimibe appears to cause elevated liver enzymes. Functional tests include elevated alanine transaminase and aspartate transaminase.
Lifestyle changes: Therapeutic lifestyle changes are recommended as initial treatment for mild cases of hyperlipidemia and people without CHD or CHD risk equivalents with fewer than two risk factors. The diet should be restricted to 25%-35% of energy intake, with saturated fatty acids making up less than 7%, and cholesterol intake limited to 200 mg a day. Plant sterol esters and soluble fiber are preferred (Verma N, 2016).
Ayurvedic treatment: Ayurvedic medicine is one of the oldest medical systems in the world. Ayurvedic therapy is based on the “laws” of nature. This approach to wellness is based on an understanding of the interrelationship between body, mind, and spirit. The goal of Ayurvedic medicine is to integrate and balance these elements to prevent disease and promote health through diet, nutrition, herbs, yoga, meditation, and seasonal daily routine (Belay B, et al., 2007).
Plant’s role in the treatment of hyperlipidemia: Medicinal plants have always been considered a source of healthy life for all peoples and international trade due to their rich therapeutic benefits and 100% natural nature. The regular use of herbal medicines in many developing countries is largely due to the high cost of Western medicines and healthcare (Bersot TP, 2011).
New potential targets and treatment options
Recently, a number of clinical studies have revealed new potential agents with promising antihyperlipidemic activity, which include:
Acyl-coA Cholesterol Acyl Transferase inhibitor (ACAT): Acyl-coA Cholesterol Acyl Transferase (ACAT) is an enzyme that catalyzes the conversion of intracellular cholesterol to cholesteryl esters. ACAT has two isomers called ACAT1 and ACAT2.
Inhibitor of Microsomal Triglyceride transfer Protein (MTP): Microsomal Triglyceride transfer Proteins (MTPs) has multiple functions, including transport of neutral lipids between membrane vesicles, CD1 biogenesis, antigen-presenting molecules and regulation of cholesterol ester biosynthesis.
Cholesterol Ester Transfer Protein (CETP) inhibitor: CETP in the liver promotes a shift of cholesteryl esters from antiatherogenic HDL to proatherogenic lipoprotein B-containing lipoproteins, including VLDL and LDL. Furthermore, most studies have shown that there is evidence that CETP may play a proatherogenic role by participating in reverse cholesterol transport, suggesting that inhibition of CETP slows atherosclerosis progression. There is support for the idea.
Lanosterol synthase inhibitor: Lanosterol Synthase (LSS) catalyzes the cyclization of 2,3-oxidosqualene to lanosterol, the first sterol in the cholesterol synthesis pathway.
Recent drugs for hyperlipidemia: The FDA has approved two new non-statin drugs that have been shown in clinical trials to potentially help lower high cholesterol. Nexretol and Nexlyzet can be used with statins with reduced or minimal side effects. Two new drugs have some side effects that differ from statins (Tables 2 and 3).
| S.no | Agents | Dose | No. of days | Cell lines | Mechanism of action | References |
|---|---|---|---|---|---|---|
| 1 | Triton X100 | 0.01% | Single induction |
Hepatoma cells | Triton X100 accelerates hepatic cholesterol synthesis and intestinal lipid absorption suppresses the action of lipoprotein lipase circulation by extra hepatic tissue resulting in blood lipid concentration and causing hyperlipidemia. | Ahn JM, et al., 1997 |
| 2 | Triton WR-1339 | 10 mg/ml | Triton WR-1339 increased oxidative stress through an elevation in that associated with depletion in glutathione activates the GST, SOD, GSH, PX and CAT in plasma, liver and brain then triton WR induced into DNA fragments and inhibit Acetylcholine (ACH) | Tacherfiout M, et al., 2018; Yamamoto K, et al., 1984 | ||
| 3 | Methionine | 1% (w/w) | Methionine increases serum triglycerides and total concentration of cholesterol activity in tissue by decreases lipoprotein lipase activity in tissue dietary methionine increase bile acid secretion which excreted into the faeces which enhance hepatic cholesterol which causes hyperlipidemia. | Hidiroglou N, et al., 2004; Kawasaki M, et al., 2008 | ||
| 4 | D-fructose | 0.55 mM | High fructose diet which increases hepatic secretion of very low-density lipoproteins this decreases the plasma clearance which causes hyperlipidemia | Huang D, et al., 2011 |
Table 2: Inducing agents of in vitro models
| S.no | Agents | Dose | No. of days | ROA | Animals | Mechanism of action | Reference |
|---|---|---|---|---|---|---|---|
| 1 | Triton X100 | 1.5 and 3 mg/kg | 21 | I.P | Rats | Triton X100 accelerates hepatic cholesterol synthesis and intestinal lipid absorption suppresses the action of lipoprotein lipase circulation by extra hepatic tissue resulting in blood lipid concentration and causes hyperlipidemia. | Parwin A, et al., 2019 |
| 2 | Triton WR-1339 | 400 mg/kg | 7 | I.P | Male wistar rats | Triton WR-1339 inhibit the activity of lipoprotein lipase enzyme, this result in accumulation of triglycerides and very low density lipoproteins it increases the hepatic cholesterol biosynthesis | Zarzecki MS, et al., 2014; Kumar G, et al., 2013 |
| 3 | Poloxamer-407 | 0.5 and 1 g/kg | 12 | I.P | Rats | Poloxamer 407 increase serum lipoprotein and inhibit the lipoprotein lipase which facilitates the hydrolysis of triglycerides which result in hyperlipidemia | Johnston TP and Palmer WK, 1993; Chaudhary HR and Brocks DR, 2013 |
| 4 | Doxorubicin | 6 mg/kg | 5 weeks | I.V | Rats | Doxorubicin decreases L carnitine and causes hyperlipidemia nephropathy | Badary OA, et al., 2000 |
| 5 | D-Galactosamine | 400 mg/kg | 1 | Oral | Male albino rats | D galactosamine induced fatty liver and significantly increases cholesterol free fatty acids, triglycerides and phospholipids and causes hyperlipidemia | Arivu I and Muthulingam M, 2015 |
| 6 | Cyclosporin A | 25 mg/kg | 28 | I.P | Male rats | Cyclosporine A inhibits ApoB and VLDL transportation over the endoplasmic reticulum so that reduction and the efficiency of lipid by inhibition of MTP | Afshari AT, et al., 2005; Kockx M, et al., 2012 |
| 7 | Adriamycin | 1.5 mg/kg | Weekly twice | I.P | Male lewis inbred rats | This increases the cholesterol, phospholipids and triglycerides which causes hyperlipidemia nephropathy | Kunitomo M, et al., 1985 |
| 8 | High fat diet | 20% sucrose, 15% lard, 1.2% cholesterol, 0.2% bile salts, 10% casein, 0.6% calcium hydro phosphate, 0.4% mountain flour | Six weeks | Oral | Male Sprague Dawley rats | Increase the VDL, HDL, VLDL, triglycerides level and causes hyperlipidemia | Kim MH, et al., 2016; Duan R, et al., 2021 |
Table 3: Inducing agents used in in vivo models
Discussion and Conclusion
This review is based on a study of many articles that gives information about hyperlipidemia and in vitro, in vivo inducing models. As hyperlipidemia is the main cause of many complicated diseases. Hyperlipidemia is the top disease that causes mortality throughout the world. According to the surveillance, this is an increase in the cholesterol level yearly. It is one of the major risk factors that affect heart structure and functions. We mainly focus on the prevention and treatment of hyperlipidemia and also it helps in preventing complicated diseases. According to Ezeh KJ and Ezeudemba O, recent changes in treatment recommendations are providing greater guidance for the management of Hyperlipidemia. Statins are the frontline treatment for hyperlipidemia. Medicinal plants give a 100% therapeutic effect. This also gives information about new drugs approved by FDA. This review is also an overview of inducing models used in experimental studies. According to Ahn JM and Parwin A, Triton X100 and Triton WR1339 are most widely used for experimental studies. It also provides information about the various inducing models used in in vitro and in vivo with their mechanism of action. This article is useful for future studies.
Acknowledgements
We acknowledge our college for providing a platform for my review work.
References
- Shattat GF. A review article on hyperlipidemia: Types, treatments and new drug targets. Biomed Pharmacol J. 2015; 7(1): 399-409.
- Mishra PR, Panda PK, Apanna KC, Panigrahi S. Evaluation of acute hypolipidemic activity of different plant extracts in Triton WR-1339 induced hyperlipidemia in albino rats. Pharmacologyonline. 2011; 3(4): 925-934.
- Jeyabalan S, Palayan M. Antihyperlipidemic activity of Sapindus emarginatus in Triton WR-1339 induced albino rats. Res J Pharm Technol. 2009; 2(2): 319-323.
- Ezeh KJ, Ezeudemba O. Hyperlipidemia: A review of the novel methods for the management of lipids. Cureus. 2021;13(7): e16412.
[Crossref] [Google Scholar] [Pubmed]
- Altmann SW, Davis Jr HR, Zhu LJ, Yao X, Hoos LM, Tetzloff G, et al. Niemann-Pick C1 Like 1 protein is critical for intestinal cholesterol absorption. Science. 2004; 303(5661): 1201-1204.
[Crossref] [Google Scholar] [Pubmed]
- Brouwers MC, van Greevenbroek MM, Stehouwer CD, de Graaf J, Stalenhoef AF. The genetics of familial combined hyperlipidaemia. Nat Rev Endocrinol. 2012; 8(6): 352-362.
[Crossref] [Google Scholar] [Pubmed]
- Noubiap JJ, Nansseu JR, Bigna JJ, Jingi AM, Kengne AP. Prevalence and incidence of dyslipidaemia among adults in Africa: A systematic review and meta-analysis protocol. BMJ Open. 2015; 5(3): e007404.
[Crossref] [Google Scholar] [Pubmed]
- Mendis S, Puska P, Norrving BE, World Health Organization. Global atlas on cardiovascular disease prevention and control. World Health Organization. 2011.
- Mumthaj P, Natarajan P, Janani AM, Vijay J, Gokul V. A global review article on hyperlipidemia. Int J Pharm Sci Rev Res. 2021; 68(1): 104-110.
[Crossref]
- Singh R, Nain S. A mini-review on hyperlipidemia: Common clinical problem. Interv Cardiol J. 2018; 4(3): 10-11.
- DuBroff R, de Lorgeril M. Cholesterol confusion and statin controversy. World J Cardiol. 2015; 7(7): 404-409.
[Crossref] [Google Scholar] [Pubmed]
- Gupta R, Rao RS, Misra A, Sharma SK. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J. 2017; 69(3): 382-392.
[Crossref] [Google Scholar] [Pubmed]
- Pandey G. NFHS-5: Indians are getting fatter-and it's a big problem. BBC News. 2022.
- Joseph D. Pharmacotherapy: A pathophysiological approach. The McGraw Hill companies. 2011; 370.
- Pattis P, Wiedermann CJ. Ezetimibe-associated immune thrombocytopenia. Ann Pharmacother. 2008; 42(3): 430-433.
[Crossref] [Google Scholar] [Pubmed]
- Karachi H, Muppidi V, Wyne K. Hypertriglyceridemia. StatPearls. 2022.
[Pubmed]
- Sharma A, Khanijau MR, Agarwal MR. Hyperlipidemia: A review article. Soc Sci Rev. 2019; 5(2): 11-22.
- Sundaram M, Yao Z. Recent progress in understanding protein and lipid factors affecting hepatic VLDL assembly and secretion. Nutr Metab. 2010; 7(1): 1-7.
[Crossref] [Google Scholar] [Pubmed]
- Ridker PM, Genest J, Boekholdt SM, Libby P, Gotto AM, Nordestgaard BG, et al. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: An analysis from the JUPITER trial. Lancet. 2010; 376(9738): 333-339.
[Crossref] [Google Scholar] [Pubmed]
- Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2010. Natl Vital Stat Rep. 2013; 61(4): 1-117. [Crossref]
[Google Scholar] [Pubmed]
- Nirosha K, Divya M, Vamsi S, Sadiq M. A review on hyperlipidemia. Int J Novel Trends Pharm Sci. 2014; 4(5): 81-92.
- Millar JS, Maugeais C, Ikewaki K, Kolansky DM, Barrett PH, Budreck EC, et al. Complete deficiency of the low-density lipoprotein receptor is associated with increased apolipoprotein B-100 production. Arterioscler Thromb Vasc Biol. 2005; 25(3): 560-565.
[Crossref] [Google Scholar] [Pubmed]
- Dhingra S, Bansal MP. Hypercholesterolemia and apolipoprotein B expression: Regulation by selenium status. Lipids Health Dis. 2005; 4(1): 1-3.
[Crossref] [Google Scholar] [Pubmed]
- Nouh F, Omar M, Younis M. Risk factors and management of hyperlipidemia. Asian J Cardiol Res. 2018; 2(1): 1-10.
- Cunningham AB. An investigation of the herbal medicine trade in Natal/KwaZulu. University of Natal. 1988.
- Russell DW. The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem. 2003; 72(1): 137-174.
[Crossref] [Google Scholar] [Pubmed]
- Edeoga HO, Okwu DE, Mbaebie BO. Phytochemical constituents of some Nigerian medicinal plants. Afr J Biotechnol. 2005; 4(7): 685-688.
- Safeer RS, laCivita CL. Choosing drug therapy for patients with hyperlipidemia. Am Fam Physician. 2000; 61(11): 3371-3382. [Crossref]
[Google Scholar] [Pubmed]
- Elmore S. Apoptosis: A review of programmed cell death. Toxicol Pathol. 2007; 35(4): 495-516.
[Crossref] [Google Scholar] [Pubmed]
- Keshetty V, Pabba S, Gudipati R, Kandukuri JM, Allenki V. Antihyperlipidemic Activity of methanolic extract of garlic (Allium sativum L.) in Triton X-100 induced hyperlipidemic rats. J Pharm Res. 2009; 2(5): 23-31.
- da Rocha JT, Sperança A, Nogueira CW, Zeni G. Hypolipidaemic activity of orally administered diphenyl diselenide in Triton WR-1339-induced hyperlipidaemia in mice. J Pharm Pharmacol. 2009; 61(12): 1673-1679.
[Crossref] [Google Scholar] [Pubmed]
- Girija K, Lakshman K. Anti-hyperlipidemic activity of methanol extracts of three plants of Amaranthus in Triton-WR 1339 induced hyperlipidemic rats. Asian Pac J Trop Biomed. 2011; 1(1): S62-65.
[Crossref] [Google Scholar] [Pubmed]
- Irudayaraj SS, Sunil C, Duraipandiyan V, Ignacimuthu S. In vitro antioxidant and antihyperlipidemic activities of Toddalia asiatica (L) Lam. leaves in Triton WR-1339 and high fat diet induced hyperlipidemic rats. Food Chem Toxicol. 2013; 60: 135-140.
[Crossref] [Google Scholar] [Pubmed]
- Ragheb A, Attia A, Elbarbry F, Prasad K, Shoker A. Attenuated combined action of cyclosporine A and hyperlipidemia on atherogenesis in rabbits by thymoquinone. Evid Based Complement Alternat Med. 2011.
[Crossref] [Google Scholar] [Pubmed]
- Carvalho FS, Burgeiro A, Garcia R, Moreno AJ, Carvalho RA, Oliveira PJ. Doxorubicin‐induced cardiotoxicity: From bioenergetic failure and cell death to cardiomyopathy. Med Res Rev. 2014; 34(1): 106-135.
[Crossref] [Google Scholar] [Pubmed]
- Verma N. Introduction to hyperlipidemia and its treatment: A review. Int J Curr Pharm Res. 2016; 9(1): 6-14.
- Belay B, Belamarich PF, Tom-Revzon C. The use of statins in pediatrics: Knowledge base, limitations, and future directions. Pediatrics. 2007; 119(2): 370-380.
[Crossref] [Google Scholar] [Pubmed]
- Bersot TP. Drug therapy for hypercholesterolemia and dyslipidemia. Goodman and Gilman’s, The Pharmacological Basis of Therapeutics. 2011: 877-908.
- Ahn JM, Kim SJ, Kim H, Park C, Kim WH, Park JH. Triton X-100 induces apoptosis in human hepatoma cell lines. Yonsei Med J. 1997; 38(1): 52-59.
[Crossref] [Google Scholar] [Pubmed]
- Tacherfiout M, Petrov PD, Mattonai M, Ribechini E, Ribot J, Bonet ML, et al. Antihyperlipidemic effect of a Rhamnus alaternus leaf extract in Triton-induced hyperlipidemic rats and human HepG2 cells. Biomed Pharmacother. 2018; 101: 501-509. [Crossref]
[Google Scholar] [Pubmed]
- Yamamoto K, Byrne R, Edelstein C, Shen B, Scanu AM. In vitro effect of Triton WR-1339 on canine plasma high density lipoproteins. J Lipid Res. 1984; 25(8): 770-779.
[Crossref] [Google Scholar] [Pubmed]
- Hidiroglou N, Gilani GS, Long L, Zhao X, Madere R, Cockell K, et al. The influence of dietary vitamin E, fat, and methionine on blood cholesterol profile, homocysteine levels, and oxidizability of low density lipoprotein in the gerbil. J Nutr Biochem. 2004; 15(12): 730-740.
[Crossref] [Google Scholar] [Pubmed]
- Kawasaki M, Funabiki R, Yagasaki K. Effects of dietary methionine and cystine on lipid metabolism in hepatoma-bearing rats with hyperlipidemia. Lipids. 1998; 33(9): 905-911.
[Crossref] [Google Scholar] [Pubmed]
- Huang D, Dhawan T, Young S, Yong WH, Boros LG, Heaney AP. Fructose impairs glucose-induced hepatic triglyceride synthesis. Lipids Health Dis. 2011; 10: 1-10.
[Crossref] [Google Scholar] [Pubmed]
- Parwin A, Najmi AK, Ismail MV, Kaundal M, Akhtar M. Protective effects of alendronate in Triton X-100-induced hyperlipidemia in rats. Turk J Gastroenterol. 2019; 30(6): 557-564.
[Crossref] [Google Scholar] [Pubmed]
- Zarzecki MS, Araujo SM, Bortolotto VC, de Paula MT, Jesse CR, Prigol M. Hypolipidemic action of chrysin on Triton WR-1339-induced hyperlipidemia in female C57BL/6 mice. Toxicol Rep. 2014; 1: 200-208.
[Crossref] [Google Scholar] [Pubmed]
- Kumar G, Srivastava A, Sharma SK, Gupta YK. The hypolipidemic activity of Ayurvedic medicine, Arogyavardhini vati in Triton WR-1339-induced hyperlipidemic rats: A comparison with fenofibrate. J Ayurveda Integr Med. 2013; 4(3): 165-170.
[Crossref] [Google Scholar] [Pubmed]
- Johnston TP, Palmer WK. Mechanism of poloxamer 407-induced hypertriglyceridemia in the rat. Biochem Pharmacol. 1993; 46(6): 1037-1042.
[Crossref] [Google Scholar] [Pubmed]
- Chaudhary HR, Brocks DR. The single dose poloxamer 407 model of hyperlipidemia; systemic effects on lipids assessed using pharmacokinetic methods, and its effects on adipokines. J Pharm Pharm Sci. 2013; 16(1): 65-73.
[Crossref] [Google Scholar] [Pubmed]
- Badary OA, Abdel-Naim AB, Abdel-Wahab MH, Hamada FM. The influence of thymoquinone on doxorubicin-induced hyperlipidemic nephropathy in rats. Toxicology. 2000; 143(3): 219-226.
[Crossref] [Google Scholar] [Pubmed]
- Arivu I, Muthulingam M. Hypolipidemic efficacy of Boerhaavia diffusa (Linn.) in kidney on D-galactosamine induced fatty liver in male albino wistar rats. Int J Modn Res Revs. 2015; 3(7): 721-725.
- Afshari AT, Shirpoor A, Balakhani ED. The effect of garlic on cyclosporine-A-induced hyperlipidemia in male rats. Urol J. 2005; 2(3): 153-156.
[Google Scholar] [Pubmed]
- Kockx M, Kritharides L. Cyclosporin A-induced hyperlipidemia, lipoproteins-role in health and diseases. Rijeka: InTech Publishers. 2012: 337-354.
- Kunitomo M, Yamaguchi Y, Matsushima K, Futagawa Y, Bando Y. Hyperlipidemic effects of adriamycin in rats. Jpn J Pharmacol. 1985; 39(3): 323-329.
[Crossref] [Google Scholar] [Pubmed]
- Kim MH, Lee EJ, Cheon JM, Nam KJ, Oh TH, Kim KS. Antioxidant and hepatoprotective effects of fermented red ginseng against high fat diet-induced hyperlipidemia in rats. Lab Anim Res. 2016; 32: 217-223.
[Crossref] [Google Scholar] [Pubmed]
- Duan R, Guan X, Huang K, Zhang Y, Li S, Xia JA, et al. Flavonoids from whole-grain oat alleviated high-fat diet-induced hyperlipidemia via regulating bile acid metabolism and gut microbiota in mice. J Agric Food Chem. 2021; 69(27): 7629-7640.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Swathi Nalla*, Nalini Mathala, P Satya Sahithi, MS Eesha Krishna, N Anuradha, P Naga Usha Sri and Ch BhavaniCitation: Nalla S: A Brief Report on Hyperlipidemia and its Inducing Models
Received: 22-May-2023 Accepted: 23-Jun-2023 Published: 30-Jun-2023, DOI: 10.31858/0975-8453.14.6.401-407
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3