Case Report - (2022) Volume 13, Issue 9
Abstract
Severe Acute Respiratory Distress Syndrome-Coronavirus 2 (SARS-CoV-2) or COVID-19 disease can cause severe disease of the lower respiratory tract. Upper respiratory illness can also occur but symptoms are generally mild. Fatal upper airway disease like epiglottitis is rare but has been observed in those who have COVID-19 disease. In this report, we present a case of acute epiglottitis in a young male with known COVID-19 disease who presented to the emergency department with throat tightening after having sore throat for three days. Microbiological workup was negative however C1 deficiency was discovered. It is possible that viral illness triggered an episode of epiglottitis in a patient who had a predisposition for angioedema.
Keywords
COVID-19, Epiglottitis, Angioedema
Introduction
The Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS- COV-2) causes the illness known as Coronavirus Disease 19 (COVID-19). Early strains of the disease are known to cause severe lower respiratory tract illness like pneumonia and acute respiratory distress syndrome. The new Omicron variant, on the other hand, is thought to cause a milder infection due to greater infiltration of the upper respiratory tract rather than the lung par- enchyma (Halfmann PJ, et al., 2022; McMahan K, et al., 2022). Upper Respiratory Infections (URI) typically generates symp- toms like pharyngodynia, nasal congestion, dysgeusia, olfactory dysfunction, and rhinorrhea. Epiglottitis, or inflammation of the epiglottis and adjacent structures that can lead to complete air- way obstruction, is a manifestation of URI that is rarely seen in patients with COVID-19 disease (Guerra AM and Waseem M, 2022; Emberey J, et al., 2021). In this case presentation, we report a rare case of epiglottitis in a COVID positive patient who was found to have C1 inhibitor deficiency. Of note, variant testing was not available, and our patient could have had either the Omicron or Delta variant since these were the predominant variants at the time of his presentation. The timing of his disease in early January 2022 makes infection with the Omicron variant possible.
Case Presentation
A 19-year-old Hispanic male with no significant past medical his- tory other than a COVID positive test one week prior presented to the emergency department with throat tightening that started earlier that day. He had been having sore throat for three days but no other symptoms. On the day of presentation, he ate sushi but he emphasized that he started feeling worsening throat dis- comfort prior to that. He eats sushi one to two times per week and has never experienced throat tightening before. For the last five years, he has been experiencing colicky abdominal pain with diarrhea and edema of his hands, feet, and scrotum every one to two months without obvious triggers. He denied family history of angioedema.
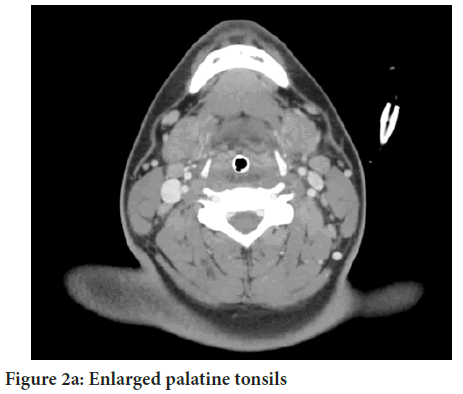
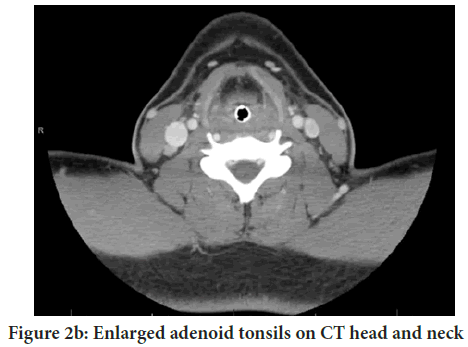
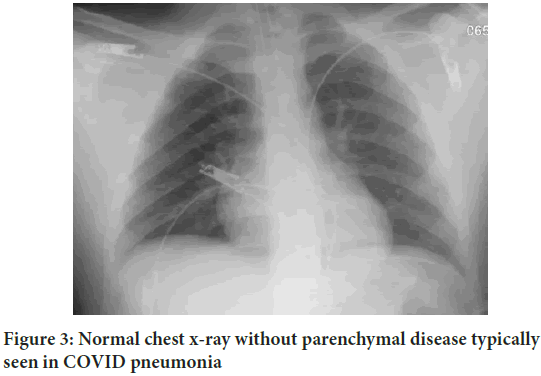
In the emergency department, the patient had a temperature of 98.6 °F, blood pressure 127/94, heart rate 113, respiratory rate 28, and oxygen saturation of 98% on room air. His BMI was 31.2. Physical exam was significant for enlarged epiglottis visualized with a tongue depressor (Figure 1). He was breathing comfort- ably on room air however he had severely limited neck motion, could only breathe when sitting upright, and had difficulty toler- ating his secretions. No rashes or edema of his hands or feet were observed. Initial labs were normal though the patient was still COVID positive. Radiograph of his neck showed swelling of his epiglottis concerning for epiglottitis. Chest x-ray showed normal lung parenchyma. He was given 10 mg IV dexamethasone and 0.5 mL of nebulized racemic epinephrine, and then taken to the operating room for intubation by an anesthesiologist. An ENT was also present in case the patient needed a surgical airway like tracheostomy or cricothyrotomy. Direct visualization of the air- way via laryngoscopy by ENT showed nonpurulent edema of the epiglottis, aryepiglottic folds, and arytenoids. Intubation was suc- cessful, thus obviating the need for creation of a surgical airway. The patient was then transferred to the Intensive Care Unit (ICU) and started on standard epiglottitis medical treatment: Empiric vancomycin 1 g every 8 hours, ceftriaxone 1 g every 24 hours, and dexamethasone 8 mg every 8 hours (Dowdy RA and Cornelius BW, 2020). He was not given standard COVID-19 therapy, namely remdesivir or baricitinib because he was not hypoxic. Computed tomography of his neck obtained while he was in the ICU showed enlarged and edematous nasopharyngeal adenoids and palatine tonsils (Figures 2a and 2b). Repeat laryngoscopy by ENT two days later showed normal epiglottis. The patient was extubated on day two of ICU stay and transferred to a medicine ward.
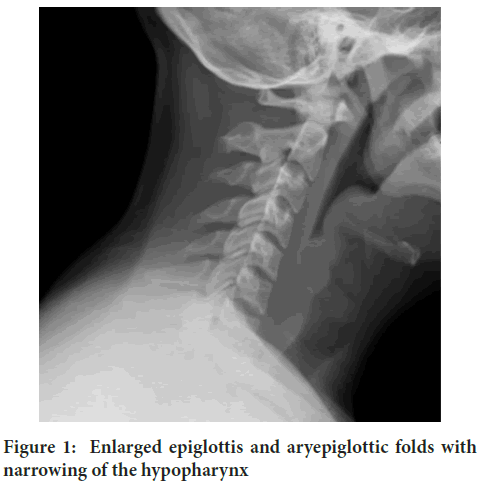
Figure 1: Enlarged epiglottis and aryepiglottic folds with narrowing of the hypopharynx
Figure 2a: Enlarged palatine tonsils
Figure 2b: Enlarged adenoid tonsils on CT head and neck
Results and Discussion
This case presentation is not the first report of COVID-19-related epi- glottitis. Known cases to date are variable. The first known case involves a 60-year-old male patient with severe obesity who presented with dys- phagia, hoarseness, and shortness of breath after using an e-cigarette with cannabis oil the night before. His initial COVID-19 high-sensitivity PCR test was negative however he tested positive the next day. He was found to have purulent epiglottitis and cricothyrotomy was required following unsuccessful intubation (Fondaw A, et al., 2020). Another case exhibits a 53-year-old male with no significant past medical history who developed epiglottis three weeks after testing positive for COVID-19 and he required emergent tracheostomy and longer period of ventilatory support (Emberey J, et al., 2021). A third case discusses a 29-year-old male with no significant past medical history who developed purulent epiglottitis two weeks after recovering from the initial COVID-19 infection, suggesting secondary bacterial superinfection as the potential cause. This patient required trach- eostomy (Renner A, et al., 2021). Another case involves a 43-year-old male former smoker with history of hypertension well controlled with losartan who presented with dysphagia and hoarseness four days after testing posi- tive for COVID-19. His airway was managed successfully with endotrach- eal intubation and he was extubated two days later (Smith C, et al., 2021).
Due to variability in the case reports described, it is difficult to ascertain risk factors for developing epiglottitis in patients who have COVID-19 dis- ease. We present a case of epiglottitis in a patient with COVID-19 disease and a history suggestive of HAE. HAE is a disorder that causes cutaneous and submucosal swelling due to C1 inhibitor deficiency (Grumach AS, et al., 2021). C1 inhibitor deficiency results in excessive production of brady- kinin, thereby causing angioedema usually of the face, lips, gut, oral cavity, and larynx. It becomes fatal when angioedema involves the larynx and leads to airway obstruction (Memon RJ and Tiwari V, 2022). Angioedema attacks have been linked to menstruation, mental stress, physical exertion, weather changes, infections, mechanical trauma, and foodstuffs (Zot- ter Z, et al., 2014). Whether this patient had true infectious epiglottis or angioedema triggered by COVID-19 or exposure to seafood is difficult to determine. Of note, the patient had eaten sushi before on numerous occasions and never experienced throat tightening. He also did not have angioedema anywhere else in his body and his tryptase level was normal, making systemic mastocytosis less likely. A study was conducted to charac- terize COVID-19 infection among patients with HAE and found that HAE patients affected by COVID-19 did not develop acute angioedema attacks (Grumach AS, et al., 2021). Perhaps our patient with suspected HAE de- veloped an acute attack because he could have had the Omicron variant, which affects the upper more than the lower respiratory tract. His normal chest X-ray also supports infection with this newer strain though this is difficult to establish (Figure 3). The cases described in our report suggest that epiglottitis develops on average six to seven days following initial COVID-19 symptoms. This average is skewed; four out of the five cases developed epiglottitis one to three days after initial symptoms and one case developed epiglottitis twenty-six days later. Patients who had epiglottitis and COVID-19 disease required varying lengths and methods of airway protection. The three cases that required tracheostomy or cricothyrotomy involved longer duration of mechanical ventilation ranging from six to thirteen days (Emberey J, et al., 2021; Dowdy RA and Cornelius BW, 2020; Renner A, et al., 2020). The fourth case described above reports a patient who required only two days of endotracheal intubation (Smith C, et al., 2021).
Figure 3: Normal chest x-ray without parenchymal disease typically seen in COVID pneumonia
This case is like ours not only because of the duration and method of airway protection, but also because the authors proposed that COVID-induced angioedema (Abdullah F, et al., 2022), rather than true infectious epiglottis, could have caused the airway edema though this is purely speculation.
Conclusion
Perhaps true infectious epiglottitis causes more severe swelling and airway friability that necessitates surgical airways and longer mechanical ventila- tion. There was no clear association between length of mechanical venti- lation and age, medical comorbidities, or treatment received while hos- pitalized. Without variant testing, it is impossible to know with certainty which strain affected our patient. We are sharing this case with the scien- tific community to highlight that since the Omicron variant is reported to cause more upper respiratory disease and has become prevalent, clinicians should be vigilant about epiglottitis as more cases could arise. Although the Omicron variant is believed to cause milder illness and lower rates of death, epiglottitis is a life-threatening condition and maintaining a high index of suspicion is crucial.
Ethical Approval
This study adheres to the ethical standards of our institution.
Consent for Publication
We obtained written informed consent from the patient for publication of this case report. A copy of the consent is available for review upon request.
References
- Halfmann PJ, Iida S, Iwatsuki-Horimoto K, Maemura T, Kiso M, Scheaffer SM, et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters. Nature. 2022; 603(7902): 687-692.
[Crossref] [Google scholar] [Pubmed]
- McMahan K, Giffin V, Tostanoski LH, Chung B, Siamatu M, Suthar MS, et al. Reduced pathogenicity of the SARS-CoV-2 Omicron variant in hamsters. Med. 2022; 3(4): 262-268.
[Crossref] [Google scholar] [Pubmed]
- Guerra AM, Waseem M. Epiglottitis. 2022.
- Emberey J, Velala SS, Marshall B, Hassan A, Meghjee SP, Malik MJ, et al. Acute epiglottitis due to COVID-19 infection. Eur J Case Rep Intern Med. 2021; 8(3): 002280.
[Crossref] [Google scholar] [Pubmed]
- Dowdy RA, Cornelius BW. Medical management of epiglottitis. Anesth prog. 2020; 67(2): 90-97.
[Crossref] [Google scholar] [Pubmed]
- Fondaw A, Arshad M, Batool S, Robinson B, Patel T. COVID-19 infection presenting with acute epiglottitis. J Surg Case Rep. 2020; 2020(9): rjaa280.
[Crossref] [Google scholar] [Pubmed]
- Renner A, Lamminmäki S, Ilmarinen T, Khawaja T, Paajanen J. Acute epiglottitis after COVID‐19 infection. Clinical Case Reports. 2021; 9(7).
[Crossref] [Google scholar] [Pubmed]
- Smith C, Mobarakai O, Sahra S, Twito J, Mobarakai N. Case report: Epiglottitis in the setting of COVID-19. IDCases. 2021; 24: e01116.
[Crossref] [Google scholar] [Pubmed]
- Grumach AS, Goudouris E, Junior SD, Marcelino FC, Alonso ML, de Oliveira RM, et al. COVID-19 affecting hereditary angioedema patients with and without C1 inhibitor deficiency. J Allergy Clin Immunol Pract. 2021; 9(1): 508-510.
[Crossref] [Google scholar] [Pubmed]
- Memon RJ, Tiwari V. Angioedema. StatPearls Publishing. 2022.
- Zotter Z, Csuka D, Szabó E, Czaller I, Nébenführer Z, Temesszentandrási G, et al. The influence of trigger factors on hereditary angioedema due to C1-inhibitor deficiency. Orphanet J Rare Dis. 2014; 9(1): 1-6.
[Crossref] [Google scholar] [Pubmed]
- Abdullah F, Myers J, Basu D, Tintinger G, Ueckermann V, Mathebula M, et al. Decreased severity of disease during the first global omicron variant COVID-19 outbreak in a large hospital in tshwane, South Africa. Int J Infect Dis. 2022; 116: 38-42.
[Crossref] [Google scholar] [Pubmed]
Author Info
Jackie Tsao1* and Zhou Zhang22Department of Pulmonary and Critical Care, Kaiser Permanente Los Angeles Medical Center, Los Angeles, United States of America
Citation: Tsao J: A Case of Acute Epiglottitis from COVID-19 Infection
Received: 29-Aug-2022 Accepted: 23-Sep-2022 Published: 30-Sep-2022, DOI: 10.31858/0975-8453.13.9.627-629
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3