Mini Review - (2023) Volume 14, Issue 11
Abstract
Parkinsonism is an umbrella term used to identify patients with clinical features consisting of bradykinesia, rigidity, rest tremors and postural instability. It can be due to Parkinson’s Disease (PD), Atypical parkinsonism, Secondary parkinsonism (usually caused by dopamine blockers, stroke, tumor, head injury or any such secondary causes) and parkinsonism as part of another condition like certain types of spinocerebellar ataxias, dystonic syndromes, pantothenate kinase associated iron accumulation in brain, for examples. This mini review discusses about atypical parkinsonian syndromes.
Keywords
Atypical Parkinson syndrome, Parkinsons Disease (PD), Progressive Supranuclear Palsy (PSP), Dementia with Lewy Bodies (DLB), Cortical Basal Degeneration (CBD), Multiple System Atrophy (MSA)
Introduction
Parkinsonism is a term used to describe patients with clinical features consisting of bradykinesia, rigidity, rest tremors and postural instability. Out of these clinical features, bradykinesia is the most important one. Parkinsonism can be due to several causes. It can be due to Parkinson’s Disease (PD), Atypical parkinsonism, Secondary parkinsonism (caused by dopamine blockers, stroke, tumor, head injury or any such secondary causes) and parkinsonism as part of other conditions like certain types of spinocerebellar ataxias, dystonic syndromes, pantothenate kinase associated iron accumulation in brain and so forth. This mini review is aimed at discussing about atypical parkinsonian syndromes for non-neurology practitioners.
Literature Review
Atypical parkinsonism
There are four syndromes currently described under this group. Progressive Supranuclear Palsy (PSP), Dementia with Lewy Bodies (DLB), Corticobasal Degeneration (CBD) and Multiple System Atrophy (MSA).
These disorders are considered atypical because, they usually does not respond to carbidopalevodopa (which is the standard medication for PD), they have early complications like cognitive decline, falls, autonomic dysfunction and they have faster progression causing the patients wheel chair bound within a few years of onset of the disease and they shortens the life span.
Progressive Supranuclear Palsy (PSP)
All the atypical syndromes are uncommon. PSP is the most common atypical parkinsonian syndrome seen in any movement disorder clinics worldwide.
It was first described in 1964 by Steele, Richardson, and Olszewski (Steele JC, et al., 1964). Because of their work, PSP is also called as Steele, Richardson, and Olszewski syndrome. After the initial description clinicians started identifying several of such patients and then started identifying variants also. Now there are about 10 variants including the original syndrome.
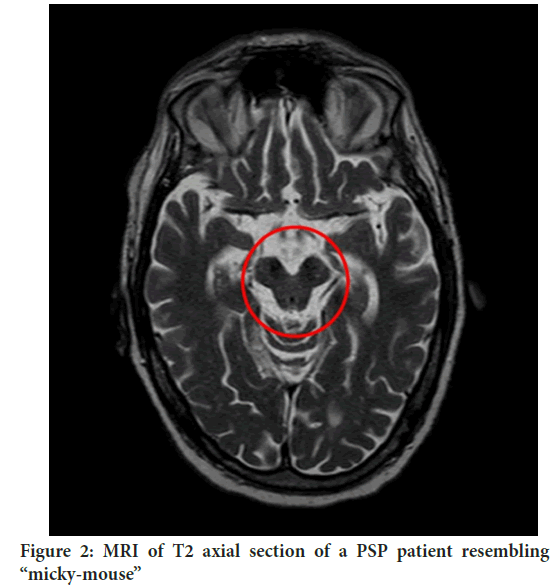
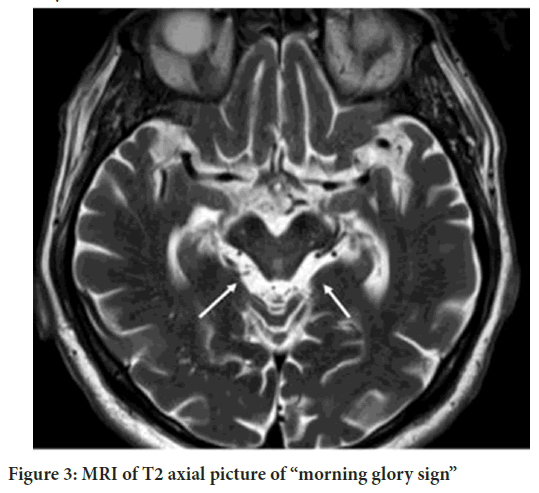
The usual age of onset of PSP is over 65 years. Along with mostly symmetric parkinsonism one important clinical feature of PSP is the vertical supranuclear palsy. This starts with slowing of vertical saccades and the limitation of vertical gaze (down gaze limitation is the classic feature, up gaze limitation can be seen even in some elderly people). Over time, this worsens and the gaze in all directions can become fixed. PSP patients also can start falling very early in the course of illness, probably starting within 1 year of onset of clinical features. Along with that, they usually develop early frontal predominant cognitive decline which is characterized by executive dysfunction and loss of insight. Because of the loss of insight into the illness, even with falls, they may try to walk again without assistance and can fall again which can be a real challenge to care givers. The parkinsonian symptoms (bradykinesia, rigidity, rest tremors) usually do not respond to carbidopa-levodopa. Even though the diagnosis is essentially clinical, there are some MRI features which can be helpful for the diagnosis. “Hummingbird” sign (Graber JJ, Staudinger R, 2009), “Morning Glory sign” and “Micky-Mouse sign” are the three well know MRI features of PSP (Figures 1-3).
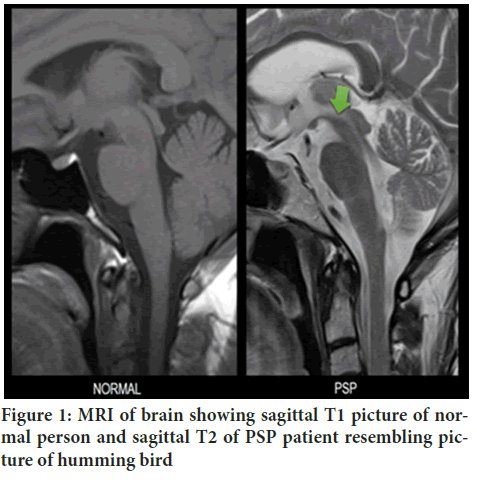
Figure 1: MRI of brain showing sagittal T1 picture of normal person and sagittal T2 of PSP patient resembling picture of humming bird
Figure 2: MRI of T2 axial section of a PSP patient resembling “micky-mouse”
Figure 3: MRI of T2 axial picture of “morning glory sign”
As mentioned earlier, PSP does not respond to medications usually. Patients will need to be referred to speech and physical therapists for assessments. Symptoms like drooling and dystonia can be treated with Botulinum toxin injections.
These patients become wheel chair bound in about 3-5 years of onset and may die in about 6-8 years from the onset. Some of the variants of PSP can have some response to the medication and may have slower progression.
Dementia with Lewy Bodies (DLB)
DLB is the next common atypical parkinsonian syndrome. It is also considered as the second commonest cause of dementia after Alzheimer’s Dementia (AD). There is an arbitrary 1 year cut off, differentiating DLB from PD with Dementia (PDD). If dementia is preceding parkinsonian motor symptoms or dementia occurs within 1 year of the parkinsonian motor symptoms, then the patient is thought to have DLB, otherwise the patient is diagnosed as having PDD (McKeith IG, et al., 2017).
In general, DLB is usually more of a cognitive problem than a parkinsonian syndrome. Cognitive dysfunction is characterized by executive dysfunction, attention and visuospatial disturbances as opposed to AD where memory loss will the early predominant feature. These patients have early visual hallucinations, fluctuations, REM sleep Behavior Disorders (RBD) and sensitivity to antipsychotic medications. Parkinsonian motor features are usually mild than from the typical PD patients, but usually is not that responsive to carbidopa-levodopa treatment. MRI brain shows more diffuse atrophy than PD patients. Dopamine Transporter scan (DaT) which is a functional imaging technique which has a specificity of about 90% in showing dopamine deficiency can be used to differentiate DLB from AD, if clinical diagnosis is not clear (Walker Z, et al., 2002). There is a newer diagnostic test which is the skin biopsy to detect alpha-synuclein in peripheral nerves. This test also may be considered for using for diagnosis. (PD and MSA are the other synucleinopathies).
For treatment, cholinesterase inhibitors can be used for dementia, quetiapine, clozapine or pimavaserin can be used for controlling psychosis, along with other supportive measure.
The disease worsens over time and patients may die in about 7-10 years from the disease onset.
Cortical Basal Degeneration (CBD):
This is the third common atypical parkinsonian syndrome seen in movement disorder clinics.
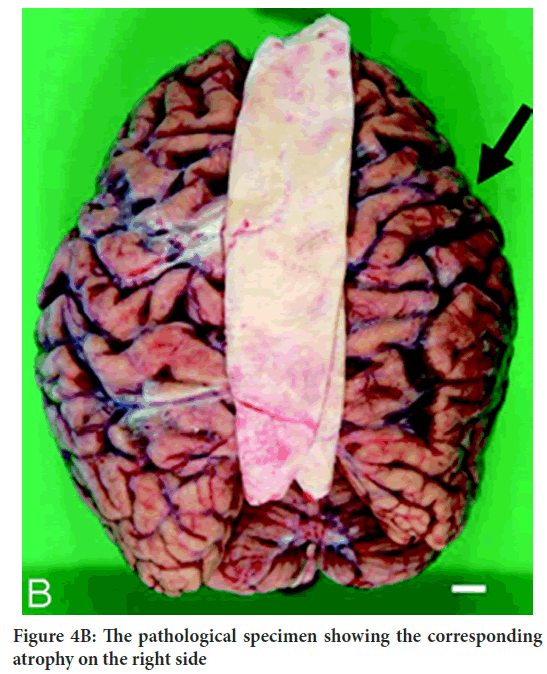
The disease can have interesting clinical features like limb apraxia, alien limb phenomena, stimulus sensitive myoclonus, cortical sensory loss along with the parkinsonian motor symptoms and cognitive decline (Riley DE, et al., 1990). Patient usually presents with asymmetric motor symptoms like that of PD. The disorder was first described in 1967. The disorder typically starts after the age of 60 years. The disease pathology is more related to PSP, both being tauopathies. The typical patient presents with asymmetric limb rigidity, bradykinesia, dystonia and cognitive abnormalities which is more of executive dysfunction, aphasia, apraxia, visuospatial disturbance and cortical sensory loss with preserved memory (Schneider JA, et al., 1997). MRI brain shows asymmetric frontal and parietal atrophy which can be helpful in diagnosis (Figures 4A and 4B).
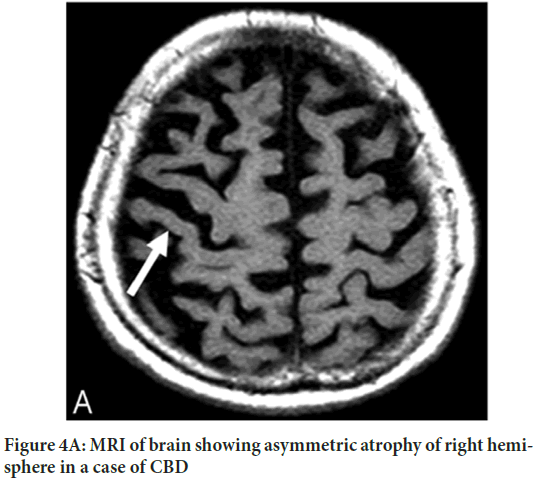
Figure 4A: MRI of brain showing asymmetric atrophy of right hemisphere in a case of CBD
Figure 4B: The pathological specimen showing the corresponding atrophy on the right side
The disease does not usually respond to levodopa treatment. Other symptoms can be tried to be helped with various medications like botulinum toxin for dystonia, choline esterase inhibitors for cognitive impairment along with physical and speech therapy. The patients worsen over time and usually die in about 6-9 years from the disease onset.
Multiple System Atrophy (MSA)
This is the rarest atypical parkinsonian syndrome seen in a movement disorder center. MSA as the word suggests, involves multiple divisions of nervous system. Systems here mean extrapyramidal system (parkinsonism), pyramidal system, autonomic nervous system and cerebellar system. To make a clinical diagnosis, patients need to have an early involvement of autonomic and\or cerebellar system along with parkinsonism. It can be classified as MSA-P and MSA-C accordingly (Stefanova N, et al., 2009).
Discussion
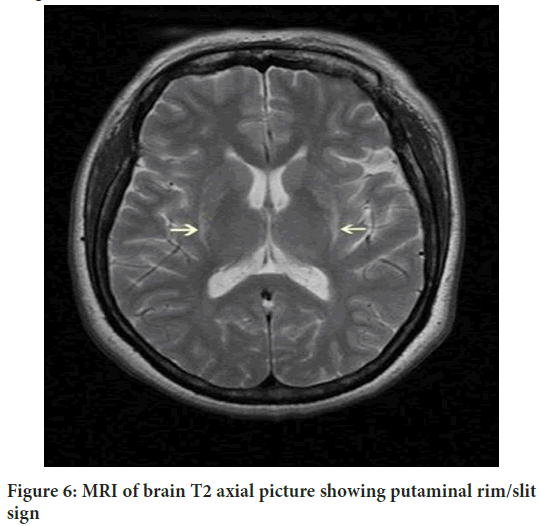
This disease was previously called as Shy-Drager syndrome or olivopontocerebellar atrophy or striatonigral degeneration. MSA patients have early involvement of autonomic nervous system which may manifest as orthostatic hypotension, erectile dysfunction in males, bladder and bowel irregularities and sweating abnormalities. The parkinsonian motor features here are more symmetric in nature with more of postural hand tremors as opposed to the more frequent resting tremors seen in PD. The patients also can have facial dystonia, early falls and postural abnormalities like camptocormia (excessive forward flexion of the body) and Pisa syndrome (excessive lateral flexion of the body). In addition, they can have pyramidal signs like hyperreflexia and/or extensor plantar response. Cerebellar ataxia is more prominent with the MSA-C type. Cognitive function is usually preserved in MSA when compared with PSP, CBD and DLB. There are two MRI findings. Hot cross bun sign and putaminal slit sign (Massano J, et al., 2008). Treatment of this condition is difficult like the others in this group (Figures 5 and 6).
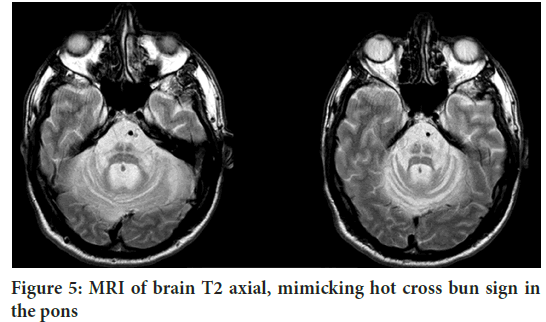
Figure 5: MRI of brain T2 axial, mimicking hot cross bun sign in the pons
Figure 6: MRI of brain T2 axial picture showing putaminal rim/slit sign
Carbidopa-levodopa can be used for parkinsonian motor symptoms. Orthostatic hypotension can be treated with fludrocortisone, midodrine or droxidopa. Botulinum toxin injection can be used for focal dystonia. Urologists/neurourologists referral may be helpful for treating bladder dysfunction and erectile dysfunction. The disease worsens fairly quickly, and patients usually become wheel chair bound in about 3-5 years and may die within approximately 6-8 years from the symptom onset.
Conclusion
Atypical parkinsonian syndromes are rare neurodegenerative disorders. The disorders usually included in atypical parkinsonian syndromes are dementia with lewy bodies, progressive supranuclear palsy, corticobasal degeneration and multiple system atrophy. These disorders are clinically heterogenous and can present with a variety of clinical findings which at times may mimic typical parkinson’s disease especially in the early stage . So keeping these differentials in mind when approaching this group of patients may help to look for red flag signs like early cognitive problems, eye movement abnormalities, orthostatic hypotension, early bulbar signs, apraxia and cortical sensory loss, which if present will point towards atypical parkinsonian syndromes as opposed to typical parkinson’s disease. Unfortunately, no treatment is currently available to prevent the progression of the disease or for cure. Identifying these disorders are important to avoid the use of unnecessary medications, especially medications like dopamine agonists, anticholinergics, monoamine oxidase inhibitors, as these patients are prone to medication side effects. However there are selected medications which can help with some of the disabling symptoms. Reaching a correct early diagnosis is important , as the information about the diagnosis and about the overall poor prognosis may help the patients and family to take. important life decisions.
Authors Contribution
Manuscript writing, conception, organization and revision were carried out by Biju Gopalakrishnan.
References
- Steele JC, Richardson JC, Olszewski J. Progressive supranuclear palsy: A heterogeneous degeneration involving the brain stem, basal ganglia and cerebellum with vertical gaze and pseudobulbar palsy, nuchal dystonia and dementia. Arch Neurol. 1964; 10(4): 333-359.
[Crossref] [Google Scholar] [Pubmed]
- Graber JJ, Staudinger R. Teaching neuroimages: “Penguin” or “hummingbird” sign and midbrain atrophy in progressive supranuclear palsy. Neurology. 2009; 72(17): e81.
[Crossref] [Google Scholar] [Pubmed]
- McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017; 89(1): 88-100.
[Crossref] [Google Scholar] [Pubmed]
- Walker Z, Costa DC, Walker RW, Shaw K, Gacinovic S, Stevens T, et al. Differentiation of dementia with Lewy bodies from Alzheimer's disease using a dopaminergic presynaptic ligand. J Neurol Neurosurg Psychiatry. 2002; 73(2): 134-140.
[Crossref] [Google Scholar] [Pubmed]
- Riley DE, Lang AE, Lewis AE, Resch L, Ashby P, Hornykiewicz O, et al. Cortical‐basal ganglionic degeneration. Neurology. 1990; 40(8): 1203-1212.
[Crossref] [Google Scholar] [Pubmed]
- Schneider JA, Watts RL, Gearing M, Brewer RP, Mirra SS. Corticobasal degeneration: Neuropathologic and clinical heterogeneity. Neurology. 1997; 48(4): 959-968.
[Crossref] [Google Scholar] [Pubmed]
- Stefanova N, Bücke P, Duerr S, Wenning GK. Multiple system atrophy: An update. Lancet Neurol. 2009; 8(12): 1172-1178.
[Crossref] [Google Scholar] [Pubmed]
- Massano J, Costa F, Nadais G. Teaching neuroImage: MRI in multiple system atrophy: “Hot cross bun” sign and hyperintense rim bordering the putamina. Neurology. 2008; 71(15): e38.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Biju Gopalakrishnan1,2*2Department of Neurology, Warren Alpert Medical School of Brown University, Butler Hospital, Rhode Island, USA
Citation: Gopalakrishnan B: Atypical Parkinsonism-A Mini Review for Non-Neurologists
Received: 03-Oct-2023 Accepted: 25-Oct-2023 Published: 02-Nov-2023, DOI: 10.31858/0975-8453.14.11.691-694
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3