Case Report - (2021) Volume 12, Issue 11
Cerebral Venous Sinus Thrombosis (CVST): An Emerging Complication of SARS CoV-2 Infection
Nicola Maggialetti1, Alessandra Gualano2*, Roberto Russo2, Rocco Umberto Accogli2 and Amato Antonio Stabile Ianora2Abstract
Background: During Coronavirus (COVID-19) pandemic, SARS CoV-2 infection has been documented to be associated with thrombotic complications, especially pulmonary embolism, which are triggered by virus binding to ACE-2 receptors and consequent activation of a cascade leading to a hypercoagulable pathway, however Cerebral Venous Sinus Thrombosis (CVST) is emerging as a further thrombotic complication of COVID-19.
Case presentation: We report our experience of a patient affected by SARS CoV-2 infection, who presented to our emergency department with neurological symptoms such as confusion and headache and was diagnosed with CVST at imaging exams.
Conclusion: As neurological symptoms such as confusion and headache are aspecific and shared with patients affected by SARS CoV-2 infection in absence of CVST, clinicians should be aware of this emerging hematologic complication in order to recognize it as soon as possible and provide the best patient care.
Keywords
SARS-CoV-2, COVID-19, CVST, Headache, Venous thromboembolism, Coagulation
Background
Cerebral venous sinus thrombosis (CVST) is an uncommon cause of stroke (<1%) (Nwajei F, et al., 2020), with an annual incidence of 2-5 cases per million people, more commonly occurring in younger patients, particularly women. Most common symptoms are headache, seizures and focal neurologic deficits, while several risk factors, like an inherited coagulopathy, an antecedent history of trauma, cancer, or use of hormonal contraceptives have been identified (Dakay K, et al., 2020). During last year, it has been assumed that SARS-CoV-2 may represent a new risk factor for CVST, by binding with angiotensin converting enzyme 2 (ACE- 2) receptors and triggering a cytokine cascade which leads to a hypercoagulable state (Nwajei F, et al., 2020). Although venous thromboembolic events in other anatomic districts have been widely described in literature, CVST still represents a less frequently reported condition.
Case Presentation
A 46-year-old affected by class II obesity (BMI=37 kg/m²) presented to our emergency department with a confusional state occurred after seizures. Five days before, due to new-onset cough and fever, he underwent a nasopharyngeal swab with a RT-PCR for SARS CoV-2, which resulted positive; he had also been complaining of a headache for three days.
On admission, blood tests revealed high levels of inflammatory markers, platelet count almost reaching the upper limit of normal range (377 × 109/L), normal coagulation parameters (INR<1,20) and elevated D-dimers (11787 μg/mL). Chest CT revealed the presence of bilateral multifocal areas of ground-glass opacities and consolidations at lower lobes; CT pulmonary angiogram excluded Pulmonary Artery Embolism (PAE). In addition, brain CT showed a focal area of increased density of the right parietal cerebral cortex associated to fronto-insular subarachnoid hemorrhage ipsilaterally. After the onset of respiratory failure, the patient was admitted in Intensive Care Unit, where he underwent mechanic ventilation.
Cerebral angiography revealed neither any arteriovenous malformations nor any aneurysms, but showed extensive thrombosis involving the right transverse and sigmoid sinus, ipsilateral internal giugular vein and deep cerebral venous system (in particular, the vein of Galen) (Figure 1) The day after, brain CT showed cerebral infarction of the right temporal and insular lobes with a hemorrhagic component, while Magnetic Resonance Venography (MRV) confirmed angio g raphic findings of CVST, which also extended at straight sinus.During the following days, another brain CT was performed and and demonstrated left temporal lobe infarction (Figure 2).
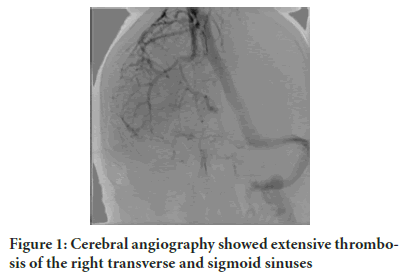
Figure 1: Cerebral angiography showed extensive thrombosis of the right transverse and sigmoid sinuses
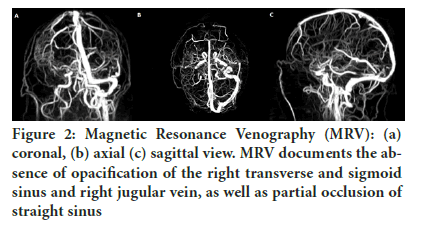
Figure 2: Magnetic Resonance Venography (MRV): (a) coronal, (b) axial (c) sagittal view. MRV documents the absence of opacification of the right transverse and sigmoid sinus and right jugular vein, as well as partial occlusion of straight sinus
Results and Discussion
More and more studies in literature document the hematological complications of SARS CoV-2 infection: in particular, the incidence of venous thromboembolism in hospitalized patients diagnosed with COVID-19 oscillates between 7.7% and 28% and it occurs even after anticoagulant therapy.
The incidence of arterial ischemic stroke as a neurological complication during COVID-19 disease is reported more frequently (Tu TM, et al., 2020), instead, only few cases reports document CVST. From the few available data in literature on this subject, our patient responds with some agreement with the epidemiological, clinical, radiological and laboratory characteristics of CVST in the COVID patient. The patient infected with SARS CoV-2 and CVST has a greater mean age than the general population diagnosed with CVST (approximately 51 vs 37 years, respectively) and is more frequently male (unlike the general population) (Mowla A, et al., 2020).
The patient may present an additional risk factor for thrombophilic diathesis, such as contraceptive hormone therapy, hereditary coagulopathies, history of cancer and obesity, as in our case, although CVST in COVID-19 disease can also arise regardless of the presence of these factors (Dakay K, et al., 2020). Even the clinical presentation of our patient does not differ from what emerges from literature: indeed, the most frequently described symptoms in these patients are headache, altered state of consciousness, seizures and focal neurological deficits (Mowla A, et al., 2020), although the last ones were not present in our case.
The agreement also concerns the most frequent sites of CVST affecting the venous sinuses, namely the transverse sinus (75%) and the sigmoid sinus (50%) (Tu TM, et al., 2020), although in our case the thrombosis subsequently affected the rectus sinus, also extending towards the contralateral venous hemisystem.
Several laboratory parameters are often altered in these patients, in particular an increase of the inflammation indices and an alteration of the coagulation parameters are characteristic (Nwajei F, et al., 2020), in fact in our case there are normal coagulation parameters and a normal platelet count but DDs and the markers of inflammation were elevated.
As regards the vascular districts involved in thrombotic phenomena, although pulmonary thromboembolism is the most frequent thrombotic complication in patients affected by COVID-19 (Klok FA, et al., 2020; Scardapane A, et al., 2021), in our case the CT pulmonary angiogram was always negative. Therefore, our experience suggests that a prothrombotic condition of the patient affected by COVID -19 does not exclude the presence of thrombosis in other districts even in absence of PAE. In our case, indeed, in addition to the involvement of the cerebral venous circulation, at a later time also the splanchnic district was found to be involved in thrombotic phenomena.
Another interesting fact that emerges from Literature is that the concomitant presence of SARS CoV-2 and CVST leads to a poorer prognosis than that of each of the two conditions taken individually: if the death rate for COVID- 19 and CVST is estimated at 5.6% and 15% respectively, for patients with both conditions it amounts to 45.5% (Tu TM, et al., 2020).
Although a clear causal link between SARS CoV-2 infection and the onset of CVST cannot be established, in relation to the limited literature on the subject, we suspect that COVID-19 infection may increase the risk of CVST, especially in patients with predisposing risk factors for hypercoagulability, such as obesity.
As headache is a non-specific symptom and is also found in patients affected by SARS CoV-2 infection in the absence of CVST (Bolay H, et al., 2020), the recognition of this condition could be difficult, with a consequent diagnostic delay (Zierau UT, et al., 2020).
Conclusion
Therefore, even in the absence of focal neurological deficits, the presence of headache and confusion in patients with diagnosed with COVID-19 should arise the suspicion of CVST for a rapid classification and adequate management of care, also in consideration of the fact that the prognosis of CVST in such patients is significantly poorer.
Acknowledgements
Authors’ contributions
All co-authors contributed equally to this work. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethics approval and consent to participate were obtained.
References
- Nwajei F, Anand P, Abdalkader M, Arasa VC, Aparicio HJ, Behbahani S, et al. Cerebral Venous Sinus Thromboses in Patients with SARS-CoV-2 Infection: Three Cases and a Review of the Literature. J Stroke Cerebrovasc Dis. 2020: 105412.
- Dakay K, Cooper J, Bloomfield J, Overby P, Mayer SA, Nuoman R, et al. Cerebral venous sinus thrombosis in COVID-19 infection: a case series and review of the literature. J Stroke Cerebrovasc Dis. 2020: 105434.
- Tu TM, Goh C, Tan YK, Leow AS, Pang YZ, Chien J, et al. Cerebral venous thrombosis in patients with COVID-19 infection: a case series and systematic review. J Stroke Cerebrovasc Dis. 2020: 105379.
- Mowla A, Shakibajahromi B, Shahjouei S, Borhani-Haghighi A, Rahimian N, Baharvahdat H, et al. Cerebral venous sinus thrombosis associated with SARS-CoV-2; a multinational case series. J Neurol Sci. 2020; 419: 117183.
- Klok FA, Kruip MJ, Van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191: 145-147.
- Scardapane A, Villani L, Bavaro DF, Passerini F, Ianora AA, Lucarelli NM, et al. Pulmonary Artery Filling Defects in COVID-19 Patients Revealed Using CT Pulmonary Angiography: A Predictable Complication?. Biomed Res Int. 2021; 21.
- Bolay H, Gül A, Baykan B. COVID-19 is a Real Headache!. Headache. 2020; 60(7): 1415-1421.
- Zierau UT, Martel L, Lahl W. COVID-19 and Varicose Veins: Common Causes of Deep Vein Thrombosis and Embolism. J Phlebol Lymphol. 2020; 13(2).
Author Info
Nicola Maggialetti1, Alessandra Gualano2*, Roberto Russo2, Rocco Umberto Accogli2 and Amato Antonio Stabile Ianora22Department of Diagnostic Imaging, School of Medicine, University Hospital of Bari, Italy
Received: 21-May-2021 Accepted: 04-Jun-2021 Published: 11-Jun-2021
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






