Research Article - (2023) Volume 14, Issue 12
Abstract
Objective: The present study aimed to compare the safety and efficacy of Intravenous Thrombolysis (IVT) between Mongolian young and older patients with Acute Ischemic Stroke (AIS).
Methods: Data of 115 AIS patients who received recombinant tissue Plasminogen Activator (rt-PA) between May 2013 and May 2023 at the Stroke Center of Third Central Hospital were retrospectively analyzed. Patients aged <50 years (n=31) compared with those aged ≥ 50 years (n=84) with regards to baseline characteristics, symptomatic Intracerebral Haemorrhage (sICH), functional outcomes at 3 months defined as “favorable” and “poor” (modified Rankin Scale score 0-2 vs. 3-6) including in-hospital mortality.
Results: 27% of patients were <50 years old (54.8% males; mean age 42.7 ± 5.8 years). Ischemic heart disease was significantly less common in younger patients than older (22.6% vs. 58.3%, p=0.018) andthe prevalence of other determined ethiology was higher (p<0.05) in patients aged <50 years. “Favorable” outcome at 3 months was significantly higher in young adults (61.3% vs.36.9%, p=0.033) and sICH was found in 3.3% of the patients aged <50 years (p=0.897) compared to 6.0% in the older than 50 years. Mortality was present in 9.7% of the patients aged <50 years and in 21.4% of the patients aged ≥ 50 years (p=0.182). Conclusion: We conclude that Mongolian young stroke patients treated with IVT had a more favorable outcome without an increased risk of sICH and mortality compared with older patients.
Keywords
Cerebral infarction, Thrombolytic treatment, Ischemic stroke
Abbreviations
AIS: Acute Ischemic Stroke; asICH: Asymptomatic Intracerebral Hemorrhage; DBP: Diastolic Blood Pressure; DNT: Door to Needle Time; IVT: Intravenous Thrombolysis; NIHSS: National Institute of Health Stroke Study; LAA: Large Artery Aherosclerosis, OTNT: Onset to Needle Time; SBP: Systolic Blood Pressure; sICH: Symptomatic Intracerebral Hemorrhage
Introduction
Ischemic stroke in young people can be devastating in terms of loss in productive years and its impact on a young person’s life, their families, and society in general. Almost two thirds of the global burden of stroke is borne by those in developing countries (Feigin VL, et al., 2021) and the incidence of ischemic stroke among young adults is on the rise globally (Scott CA, et al., 2022; Tibæk M, et al., 2016). Young patients with acute stroke from low and middle-income countries tend to have a higher three-month mortality rate compared to their counterparts from high-income nations (Béjot Y, et al., 2016; Boot E, et al., 2020).
The occlusion of cerebral artery causes a steady decrease in cerebral perfusion pressure within minutes, resulting in an ischemic penumbra and role of recombinant tissue plasminogen activator (alteplase) is to salvage the ischemic penumbra by restoring blood supply (Powers WJ, et al., 2019).
Based on a subgroup analysis of the National Institute of Neurological Disorders and Stroke (NINDS) trials, there was greater efficacy of IVT in younger patients with AIS than in older patients (National Institute of Neurological Disorders and Stroke rt-PA stroke study group, 1995). Moreover, according to the safety implementation data of (SITS-MOST) AIS study, it was shown that patients under 50 years of age have less complications of sICH and more functional recovery than older patients (Anzini A, et al., 2008). In Mongolia, first thrombolytic therapy applied in the stroke center of Third Central Hospital in 2013 and it was introduced into treatment practice and licensed. In spite of the ethiology, risk factors, clinical features and prognosis of ischemic stroke among young adults have studied (Tsagaankhuu D, et al., 2016; Jacob MA, et al., 2022) the safety and effectiveness of IVT with rt-PA (alteplase) are lacked in Mongolian young ischemic stroke patients. Therefore, this study aimed to compare outcomes in AIS patients after IVT at young (under 50 years), old (above 50 years) age groups.
Materials and Methods
Data collection
A retrospective observational study was conducted on data from the stroke department of Shastin Third Central Hospital, Mongolia. All medical records of consecutive patients treated with IVT (Alteplase, Boehringer Ingelheim, Germany) for AIS from May 2013 to 2023 were reviewed. AIS was defined as a focal neurological deficit of sudden onset that persisted beyond 24 hours or with evidence of acute brain ischemia on neuroimaging when symptoms lasted less than 24 hours. Intravenous rt-PA (alteplase) was administered at a dose of 0.9 mg per kilogram (maximum, 90 mg), with 10% given as an initial bolus within 1 minute and the remaining 90% as a constant infusion over a period of 60 minutes (Jauch EC, et al., 2013). The inclusion/exclusion criteria were based on the 2013 AHA/ASA Guidelines for the early management of patients with AIS (within 4.5 hours) (Jauch EC, et al., 2013). All patients or patient’s care providers gave written informed consent before thrombolysis, and all patients were followed up for 3 months. All patients had a baseline CT scan and a second scan performed within 24-36 hours after rt-PA infusion to detect any intracerebral hemorrhage.
Demographic data and clinical characteristics
Demographic characteristics, risk factors, stroke Onset to Treatment Time (OTT), Door-to-Needle Time (DNT), and complete general and neurological examinations were reviewed including the Glasgow Coma Scale (GCS) to assess the consciousness level and the National Institute of Health Stroke Scale (NIHSS) (Goldstein L, et al., 1989) to assess the stroke severity. Various subtypes of ischemic stroke as per the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria were determined (Adams Jr HP, et al., 1993). The clinical outcome was measured using the modified Rankin Scale (mRS) at 3 months. The mRS is a global measure of disability on a seven-level scale, with scores ranging from 0 (no symptoms) to 6 (death) (Mohamed WS, et al., 2021). Binary outcomes included favorable (mRS score 0-2) and poor (mRS 3-6). Safety outcomes were in-hospital mortality and symptomatic Intracerebral Hemorrhage (sICH). sICH was defined according to SITS-MOST criteria as local or remote parenchymal hemorrhage type 2 on the 22- to 36-hour posttreatment imaging combined with a neurological deterioration of >4 points on National Institutes of Health Stroke Scale (NIHSS) from baseline or from the lowest NIHSS value between baseline and 24 hours or leading to death (Anzini A, et al., 2008). Asymptomatic ICH involved hemorrhage on follow-up Computed Tomography (CT) without associated clinical deterioration. Magnetic Resonance Imaging (MRI) of the brain was done in suspected brain stem lesions, early ischemic stroke, and when follow-up CT brain is free. Cardiac evaluation including ECG and echocardiography was available.
Statistical analysis
All data were collected and statistically analyzed using IBM SPSS 26.0 for Windows (SPSS Inc., Chicago, IL, USA). According to the type of data, quantitative variables were expressed as the mean ± SD and median range. The qualitative data were expressed as a number or percentage. Difference and association of qualitative variables were statistically tested for significance using the chi-square test, Fisher exact test, and differences between the quantitative independent groups were tested using the t test or rank sum test of significance. All statistical tests were two-sided, and p-values of <0.05 were considered statistically significant.
Results
Patient baseline characteristics
Comparison of patient demographic data and baseline characteristics between the two groups is shown in Table 1. Of 115 AIS patients who received intravenous rt-PA, 31 (27.0%) were young adults aged 31-49 years (mean age 42.7 ± 5.8 years) and 84 (73.0%) were older adults aged 50-80 years (mean age 63.1 ± 7.8). The proportion of males was higher in both group (54.8% vs. 58.3%, p=0.832).
| Variables | Patients <50 years old (n=31) | Patients ≥ 50 years old (n=84) | p-value |
|---|---|---|---|
| Age (years; mean ± SD) | 42.7 ± 5.8 | 63.1 ±7.8 | <0.001* |
| Male, n (%) | 17 (54.8%) | 49 (58.3%) | 0.832 |
| Hypertension, n (%) | 20 (64.5%) | 65 (77.4%) | 0.231 |
| Ischemic heart disease, n (%) | 7 (22.6%) | 41 (48.8%) | 0.018* |
| Diabetes mellitus, n (%) | 3 (9.7%) | 12 (14.3%) | 0.756 |
| Dyslipidemia, n (%) | 12 (38.7%) | 41 (48.8%) | 0.402 |
| Atrial fibrillation, n (%) | 3 (9.7%) | 14 (16.7%) | 0.554 |
| Smoking, n (%) | 15 (48.4%) | 39 (46.4%) | 0.989 |
| Alcohol intake, n (%) | 9 (29%) | 16 (19%) | 0.309 |
| Blood glucose, mmol/L (median (IQR)) | 5.7 (4.0-19.1) | 6.4 (3.9-18.2) | 0.08 |
| SBP, mmHg (median (IQR)) | 137 (100-240) | 147 (98-205) | 0.082 |
| DBP, mmHg (median (IQR)) | 90 (60-164) | 92 (52-140) | 0.212 |
| Hyperdense artery signs, n (%) | 14 (45.2%) | 37 (44%) | 0.994 |
| NIHSS on admission (mean ± SD) | 13.6 ± 4.7 | 15.2 ± 5.4 | 0.163 |
| OTT, min (median (IQR)) | 210 (77-270) | 207 (105-270) | 0.644 |
| DNT (min; mean ± SD) | 112.9 ± 38.2 | 123.3 ± 38.6 | 0.204 |
| DNT ≤ 60 minutes, n (%) | 3 (9.7%) | 2 (2.4%) | 0.12 |
| Stroke subtypes, n (%) | |||
| LAA, n (%) | 6 (19.4%) | 19 (22.6%) | 0.803 |
| Cardiogenic embolism, n (%) | 11 (35.5%) | 42 (50%) | 0.208 |
| Small vessel disease, n (%) | 9 (29%) | 17 (20.2%) | 0.325 |
| Other determined etiology, n (%) | 3 (9.7%) | 0 | 0.018* |
| Undetermined etiology, n (%) | 2 (6.5%) | 6 (7.1%) | 0.984 |
Note: *p<0.05
IQR: Interquartile Range; SD: Standard Deviation
Table 1: Demographic data and baseline characteristics
The traditional risk factors for stroke, Ischemic Heart Disease (IHD) was significantly less common in young adults compared to older adults (22.6% vs.58.3%, p=0.018) and hypertension (64.5% vs.77.4%, p=0.231) and atrial fibrillation (9.7% vs.16.7%, p=0.554) were less common. Alcohol intake was slightly more prevalent among the young adults, although there was no significant difference compared to the older adults. There was no difference between the two groups in hyperdense artery signs, baseline serum glucose, Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP).
Young patients typically presented with low-median NIHSS at admission, which indicated less severe stroke symptoms. There was no significant difference in mean DNT and in median OTT between the two groups.
The prevalence of other determined etiology (p<0.05) was higher among the young adults, but no significant difference was observed in other stroke subtypes.
Outcomes of patients under 50 and above 50 years old age groups
Clinical outcome defined by mRS at 3 months is shown in Figure 1. In young adults, a higher percentage of patients had a favorable outcome compared to older adults (61.3% vs. 36.9%, p=0.033). The proportions of patients with sICH (3.3% vs.6.0%) and 3 months mortality (9.7% vs. 21.4%) were lower for the young adults compared to older adults, but not significantly (Table 2).
| Outcomes | Patients aged <50 years old n (%) | Patients aged ≥ years old n (%) | p-value |
|---|---|---|---|
| Favorable outcome | 19 (61.3%) | 31 (36.9%) | 0.033* |
| sICH | 1 (3.3%) | 5 (6.0%) | 0.897 |
| asICH | 1 (3.3%) | 6 (7.1%) | 0.672 |
| Mortality | 3 (9.7%) | 18 (21.4%) | 0.182 |
Note: *p<0.05; Favorable outcome was defined as mRS 0-2 at 3 months
Table 2: Outcome of patients in young and older age groups
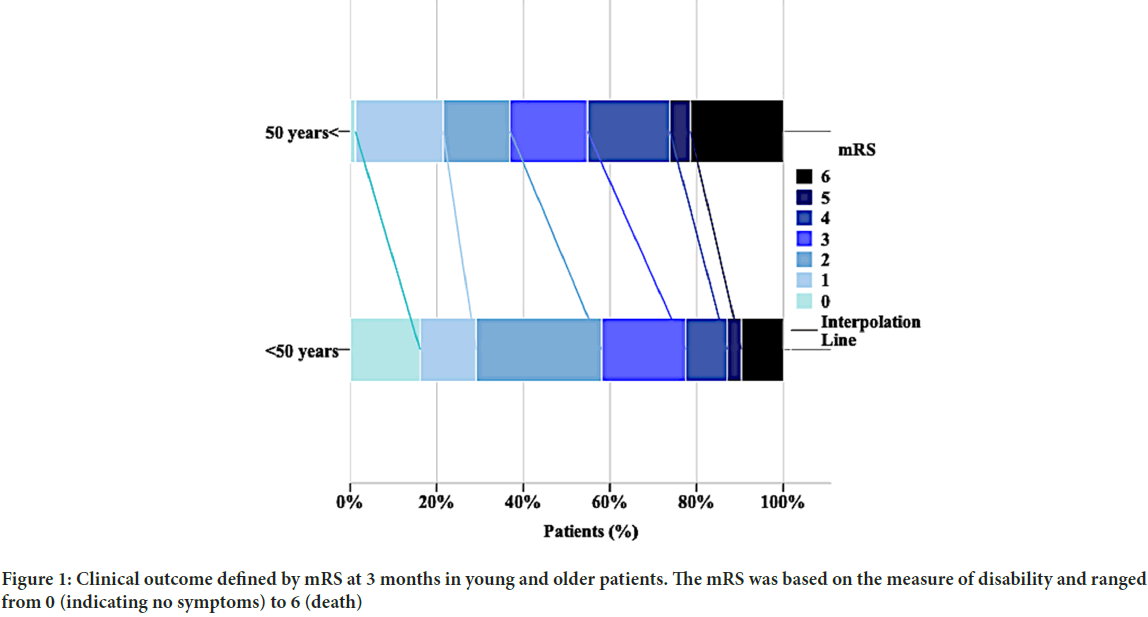
Figure 1: Clinical outcome defined by mRS at 3 months in young and older patients. The mRS was based on the measure of disability and ranged from 0 (indicating no symptoms) to 6 (death)
Discussion
Our study examined baseline characteristics and outcomes exclusively in young adult patients treated with IV-tPA for AIS compared with older patients. The favourable functional outcome and lower mortality among young adult stroke patients described by many others (National Institute of Neurological Disorders and Stroke rt-PA stroke study group; Jacob MA, et al., 2022; Ghandehari K and Moud ZI, 2006; Putaala J, et al., 2009). In our findings more than half of those treated with IVT had reached favorable functional outcome at 3 months follow-up compare to older patients treated with IVT (61.3% vs. 36.9%, p=0.033) and mortality rates were 9.7%. In study SITS-MOST patients aged 18-45 years treated within 3 hours, mortality rates were 5.5% and 54%-76% scored 0-1 and 0-2 on the 3-month mRS (Anzini A, et al., 2008). Except for the mortality rate, these findings are equivalent to ours. In post hoc analysis of the Safe Implementation of Treatments in Stroke-International Stroke Thrombolysis Registry (SITS-ISTR) trial showed that 72.1% of young adults achieved favorable outcome and 52% had no or minimal disability, as compared to 54.5% and 38.6%, respectively, of older adults. Data from a retrospective observational study based on a large hospital-based stroke registry in Southwest Germany indicated that IVT was effective in young adults, with favorable outcome (mRS ≤ 1 or not worse than pre-stroke) at discharge in 50% of patients aged 18-50 years compared to 36% in patients aged 51-80 years (Reuter B, et al., 2015). Putaala J, et al., 2009 found that proportions of dichotomized 3 months outcome scores did not differ significantly between cases and older alteplase-treated control subjects (40% and 48%, p=0.343). The differences between our results and others were likely because patients from previous studies were enrolled from single or multiple centers, while our data were from a hospital-based stroke registry with consecutively-enrolled patients.
The occurrence of sICH according to according to The Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST) criteria (Anzini A, et al., 2008) was lower in young adults compared with older adults, although there was no significant difference between the two groups. ICH is known to be an infrequent complication of IVT for the treatment of acute stroke (Norby KE, et al., 2013; Mustanoja S, et al., 2014). Data from a randomized, placebo-controlled trial in patients with ischemic stroke treated within 3 hours of symptom onset showed that approximately 30% of patients with post-thrombolytic intracerebral hemorrhage according to NINDS criteria (NINDS t-PA Stroke Study Group, 1997) had favorable outcomes (mRS 0-3) at 1 year. Moreover, other studies that compared clinical scores using multiple sICH definitions found no meaningful differences between sICH definitions (NINDS t-PA Stroke Study Group; Hacke W, et al., 1998; Asuzu D, et al., 2015). Above all, these findings indicated that the risk of sICH should not be a major concern when treating young stroke patients.
Finally, in our analysis, the 3 months mortality rate was lower in patients aged below 50 years than in older patients (9.7% vs. 21.4%), but there was no significant difference between the two groups. Putaala J, et al., 2009 evaluated 48 patients aged 16 to 49 years with hemispheric ischemic stroke treated with IVT, and none of the young patients died at 3 months. Mortality in our young adults was nearly half that of older patients, which was similar to the SITS-ISTR study results (young vs. older: 4.9% vs. 14.4%) (Toni D, et al., 2012).
Incidence of ischemic stroke in the young is relatively uncommon and the etiology is heterogeneous (Ji R, et al., 2013; Singhal AB, et al., 2013). Similarly, traditional risk factors in young stroke patients, including hypertension and ischemic heart disease, were less common than those in older patients (Jacob MA, et al., 2022; Ji R, et al., 2013; Béjot Y, et al., 2014) which was also recently reported in young population without IVT in a hospital-based cohort from China Rehabilitation Research Center (Du XX, et al., 2016). Consistent with previous results (Tsagaankhuu D, et al., 2016; Jacob MA, et al., 2022; Ghandehari K, et al., 2006; Ji R, et al., 2013) young stroke patients presented with more strokes of other determined etiology compared to older patients. Emerging studies have focused on identifying and managing the increasing prevalence of modifiable vascular risk factors in young adults; thus, their potential role in increasing the risk of ischemic stroke and stroke recurrence are worth highlighting (Du XX, et al., 2016; Singhal AB, et al., 2013).
The limitation of our study was that the study was conducted in a retrospective observational manner, and the number of young stroke patients was relatively small especially with regard to sICH, which may restrict our ability to evaluate multiple factors. Larger studies are needed to confirm our findings given our limited sample size, acute ischemic stroke treatment with IVT in young patients should be performed at least as actively as for older patients.
Conclusion
Finally, the evaluation of the 3 months efficacy of IVT is far from enough and in we should continue the follow-up of these treated patients, to identify the long-term efficacy of IVT in these young patients.
In conclusion, our analysis indicated that Mongolian young stroke patients with IVT had more favorable outcome without an increased risk of sICH and mortality compared to older patients. Although larger studies are needed to confirm our findings given our limited sample size, acute is chemic stroke treatment with IVT in young patients should be performed at least as actively as for older patients.
References
- Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, et al. Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021; 20(10): 795-820.
[Crossref] [Google Scholar] [Pubmed]
- Scott CA, Li L, Rothwell PM. Diverging temporal trends in stroke incidence in younger vs. older people: A systematic review and meta-analysis. JAMA Neurol. 2022; 79(10): 1036-1048.
[Crossref] [Google Scholar] [Pubmed]
- Tibæk M, Dehlendorff C, Jørgensen HS, Forchhammer HB, Johnsen SP, Kammersgaard LP. Increasing incidence of hospitalization for stroke and transient ischemic attack in young adults: A registry‐based study. J Am Heart Assoc. 2016; 5(5): e003158.
[Crossref] [Google Scholar] [Pubmed]
- Béjot Y, Delpont B, Giroud M. Rising stroke incidence in young adults: More epidemiological evidence, more questions to be answered. J Am Heart Assoc. 2016; 5(5): e003661.
[Crossref] [Google Scholar] [Pubmed]
- Boot E, Ekker MS, Putaala J, Kittner S, De Leeuw FE, Tuladhar AM. Ischaemic stroke in young adults: A global perspective. J Neurol Neurosurg Psychiatry. 2020; 91(4): 411-417.
[Crossref] [Google Scholar] [Pubmed]
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019.
[Crossref] [Google Scholar] [Pubmed]
- National Institute of Neurological Disorders and Stroke rt-PA stroke study group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333(24): 1581-1588.
[Crossref] [Google Scholar] [Pubmed]
- Anzini A, Niaz A, Durastanti L, Wahlgren N, Prencipe M, Toni D. Thrombolysis in young patients: The SITSMOST data. Cerebrovasc Dis. 2008; 25(Suppl 2): 3.
- Tsagaankhuu D, Guntev T, Dashjamts T, Gongor B, Avirmed T. Comparative study of ischemic stroke in patients aged above and below 50 years admitted to a tertiary care hospital in Ulaanbaatar. Cent Asian J Med Sci. 2016; 2(2): 143-152.
- Jacob MA, Ekker MS, Allach Y, Cai M, Aarnio K, Arauz A, et al. Global differences in risk factors, etiology, and outcome of ischemic stroke in young adults-a worldwide meta-analysis: The GOAL initiative. Neurology. 2022; 98(6): e573-e588.
[Crossref] [Google Scholar] [Pubmed]
- Jauch EC, Saver JL, Adams Jr HP, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44(3): 870-947.
[Crossref] [Google Scholar] [Pubmed]
- Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol. 1989; 46(6): 660-662.
[Crossref] [Google Scholar] [Pubmed]
- Adams Jr HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24(1): 35-41.
[Crossref] [Google Scholar] [Pubmed]
- Mohamed WS, Abdel Ghaffar AS, Abdel Gawad AE, Agban EL. Short-term outcome in ischemic stroke patients after thrombolytic therapy. Egypt J Neurol Psychiatr Neurosurg. 2021; 57(1): 1-8.
- Ghandehari K, Moud ZI. Incidence and etiology of ischemic stroke in Persian young adults. Acta Neurol Scand. 2006; 113(2): 121-124.
[Crossref] [Google Scholar] [Pubmed]
- Putaala J, Metso TM, Metso AJ, Mäkelä E, Haapaniemi E, Salonen O, et al. Thrombolysis in young adults with ischemic stroke. Stroke. 2009; 40(6): 2085-2091.
[Crossref] [Google Scholar] [Pubmed]
- Reuter B, Gumbinger C, Sauer T, Wiethölter H, Bruder I, Diehm C, et al. Intravenous thrombolysis is effective in young adults: Results from the Baden-Wuerttemberg Stroke Registry. Front Neurol. 2015; 6: 229.
[Crossref] [Google Scholar] [Pubmed]
- Norby KE, Siddiq F, Adil MM, Chaudhry SA, Qureshi AI. Long-term outcomes of post-thrombolytic intracerebral hemorrhage in ischemic stroke patients. Neurocrit Care. 2013; 18: 170-177.
[Crossref] [Google Scholar] [Pubmed]
- Mustanoja S, Haapaniemi E, Putaala J, Strbian D, Kaste M, Tatlisumak T. Haemorrhagic transformation of ischaemic stroke in young adults. Int J Stroke. 2014; 9(SA100): 85-92.
[Crossref] [Google Scholar] [Pubmed]
- NINDS t-PA Stroke Study Group. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. Stroke. 1997; 28(11): 2109-2118.
[Crossref] [Google Scholar] [Pubmed]
- Hacke W, Kaste M, Fieschi C, Von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet. 1998; 352(9136): 1245-1251.
[Crossref] [Google Scholar] [Pubmed]
- Asuzu D, Nyström K, Amin H, Schindler J, Wira C, Greer D, et al. TURN: A simple predictor of symptomatic intracerebral hemorrhage after IV thrombolysis. Neurocritical care. 2015; 23(2): 166-171.
[Crossref] [Google Scholar] [Pubmed]
- Toni D, Ahmed N, Anzini A, Lorenzano S, Brozman M, Kaste M, et al. Intravenous thrombolysis in young stroke patients: Results from the SITS-ISTR. Neurology. 2012; 78(12): 880-887.
[Crossref] [Google Scholar] [Pubmed]
- Ji R, Schwamm LH, Pervez MA, Singhal AB. Ischemic stroke and transient ischemic attack in young adults: Risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol. 2013; 70(1): 51-57.
[Crossref] [Google Scholar] [Pubmed]
- Singhal AB, Biller J, Elkind MS, Fullerton HJ, Jauch EC, Kittner SJ, et al. Recognition and management of stroke in young adults and adolescents. Neurology. 2013; 81(12): 1089-1097.
[Crossref] [Google Scholar] [Pubmed]
- Béjot Y, Daubail B, Jacquin A, Durier J, Osseby GV, Rouaud O, et al. Trends in the incidence of ischaemic stroke in young adults between 1985 and 2011: The Dijon Stroke Registry. J Neurol Neurosurg Psychiatry. 2014; 85(5): 509-513.
[Crossref] [Google Scholar] [Pubmed]
- Du XX, Yang K, Song LP, Li PK, Wang Q, Sun R, et al. Effects of professional rehabilitation training on the recovery of neurological function in young stroke patients. Neural Regen Res. 2016; 11(11): 1766.
[Crossref] [Google Scholar] [Pubmed]
- Singhal AB, Biller J, Elkind MS, Fullerton HJ, Jauch EC, Kittner SJ, et al. Recognition and management of stroke in young adults and adolescents. Neurology. 2013; 81(12): 1089-1097.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Delgermaa Tsagaankhuu1, Chimeglkham Banzrai2, Tsagaankhuu Guntev1* and Baigalmaa Gongor1,32Department of Neurology, Institute of Medical Sciences, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
3Stroke Department, Shastin Third Central Hospital, Ulaanbaatar, Mongolia
Citation: Tsagaankhuu D: Comparative Study of Intravenous Thrombolysis for Acute Ischemic Stroke in Mongolian Patients Aged Above and Below 50 Years
Received: 27-Nov-2023 Accepted: 11-Dec-2023 Published: 18-Dec-2023, DOI: 10.31858/0975-8453.14.12.757-761
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






