Research Article - (2022) Volume 13, Issue 7
Abstract
Background and aim: In 2020, with the advent of the COVID-19 pandemic, the demand for hospital beds in the intensive care unit has increased in a short time, but design protocols to prevent COVID-19 transmission do not yet exist, and architects are trying to make spatial changes to use protocols for other infectious diseases such as Ebola and tuberculosis.
Methods and results: In this article, we first compare the health infrastructure of Iran and other countries and examine the effect of these facilities on the control of this disease. Then, by collecting solutions of health care systems in successful countries, COVID-19 was controlled and finally, by collecting information obtained from previous researches, by conducting a questionnaire, these cases were tested. We go by specialists. The reliability of the questionnaire was calculated by calculating Cronbach’s alpha coefficient through retesting and correlation coefficient. The questionnaire was given to ten respondents two weeks apart, which the reliability coefficient obtained in two runs was higher than 1.19 and showed the high reliability of the research tool. Of the total number of respondents (54), 6 physicians (11.1%), 15 architects (hospital designers) (28.8%), 14 mechanical engineers (25.9%) and 19 civil engineers (hospital contractors) (35.2%). After collecting the data, the Shannon entropy method was used to weight the criteria. Then, the data is analyzed using the TOPSIS technique in Excel 2013 software.
Conclusion: The results show that future approaches in designing medical centers will be based on the axes of flexibility design, increasing hospital capacity, improving the prevention of infection, and changing the design approach of the hospital from short-term stay to community-based care.
Keywords
SARS-CoV-2, COVID-19, Infection design
Introduction
In late 2019, there was a report of an infectious disease from the branch of coronavirus respiratory infections in Wuhan, China (Gan WH, et al., 2020). Coronavirus is a pathogen that can be transmitted from animal to human and human to human (Bhagavathula AS, et al., 2020). The disease was named 19. It was detected through PCR polymerase chain reaction and culture of patients’ pharyngeal secretions (Zhu N, et al., 2020). The genome of this virus, which is the seventh coronavirus to infect humans, is 75%-80% similar to acute Coronavirus syndrome (CoV-SARS), 50% similar to Middle Eastern Respiratory Syndrome (CoV-MERS), and 96% similar to bat coronavirus (Arabi YM, et al., 2020). On January 30, 2020, the World Health Organization issued a statement declaring the outbreak of the new coronavirus a public health emergency for the entire world and declaring it a pandemic on March 11, 2020. (Euro surveillance editorial team, 2020) The arrival of the corona virus in Qom, Iran, was officially announced on February 19, 2010 (Euro surveillance editorial team, 2020).
Hospitals play an important role in the health system in providing essential medical care to the community, especially in critical situations. Hospitals tried to respond in an extremely short period of time to an unprecedented and sudden demand for emergency care and ICU beds for infectious diseases (Dolinger M and Marsh A, 2020). Demand for COVID-19 beds in acute care units has increased worldwide. The COVID-19 pandemics have eroded and obsolete all medical infrastructures (Dolinger M and Marsh A, 2020).
The COVID-19 pandemic has created unprecedented pressures on health care systems around the world (Ariadne Labs, 2020). The increase in respiratory and nosocomial infections following the increase in hospitalizations has forced the medical infrastructure to adapt quickly and provide emergency solutions (Dolinger M and Marsh A, 2020). The rate of infection and hospitalized patients has reached an unpredictable level. What Dr. Paul Farmer calls “staff, equipment, space, and systems” has reached its climax. According to Brian Langlandes, Director of the NBBJ, AIA: “The biggest issues facing health centers are capacity, equipment and staff, all of which must provide effective patient care in an efficient manner.”
Among these, there are many issues about the crisis of lack of equipment, medical staff and defects of medical systems, but less discussion has been raised about “space” (Dolinger M and Marsh A, 2020). What connects these issues is that medical staff (World Health Organisation is most vulnerable to infection) must stay healthy to protect patients, families and communities, and the design of the hospital space must protect the community (Dolinger M and Marsh A, 2020).
In fact, the hospital environment itself will help facilitate the spread of nosocomial infections (transmitted by the hospital), unless infection control protocols are established and communities adhere to them (Capolongo S, et al., 2020). Herein lays the issue: Valid protocols designed to prevent the transmission of COVID-19 do not yet exist, so hospitals are reviewing design and spatial changes and doing their best to use infectious disease control protocols. Others like Ebola and tuberculosis (Dolinger M and Marsh A, 2020).
The statement of the problem
The COVID-19 pandemic has become a pervasive crisis in Iran in recent days, endangering public health. But how prepared is the ICU infrastructure to deal with this crisis? In addition to the unknown nature of the disease, issues such as high virulence and lack of facilities required, including lack of hospital beds, doctor-nurse to bed ratio, equipment and care facilities such as personal protective equipment and ventilators, and high elderly population have caused major challenges for the health system.
Since the characteristics and severity of this disease are unknown and methods to deal with it have not been experienced so far, so how the hospital is prepared to deal with it is one of the main challenges.
While infection control protocols are rapidly being adopted, hospitals are not designed to easily support the pivotal support needed for infra structure changes in the Corona epidemic, posing a major challenge for architects and has created hospital designers (Capolongo S, et al., 2020).
The most important strategies for proper management of the disease and control of the disease transmission chain are rapid response to this problem. Statistics provided in different countries show that countries that reacted quickly were able to increase the number of deaths up to 10 times and the number of cases significantly and considerably reduces coronavirus (Pueyo T, 2020).
In this article, we first try to compare the health infrastructure of Iran and other countries and examine the effect of health facilities on the control of COVID-19. After that, by collecting the solutions of health care systems in successful countries, it was possible to control Quid and finally, by collecting data and information obtained from researches in this field, by conducting a questionnaire, these cases. We take it to the test stage by experts and prioritize it.
COVID-19 in Iran
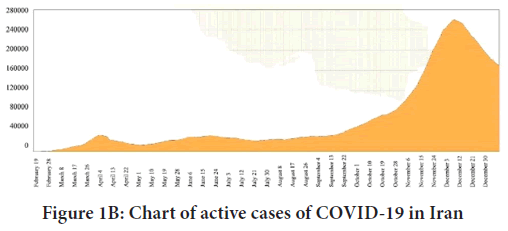
Corona spread in Iran (until January 5, 2021): According to the latest statistics released by the Ministry of Health as of January 5, 2021, the total number of patients is 1,255,620 and 55,748 people are dead. The resulting graphs show the ratio of mortality to active cases to date. The trend of increasing deaths due to COVID-19 in the country, along with the increase in hospitalizations to date, indicates a critical situation in the country (Figure 1).
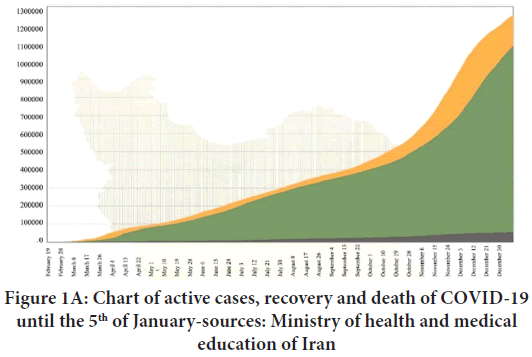
Figure 1A: Chart of active cases, recovery and death of COVID-19 until the 5th of January-sources: Ministry of health and medical education of Iran
Figure 1B: Chart of active cases of COVID-19 in Iran
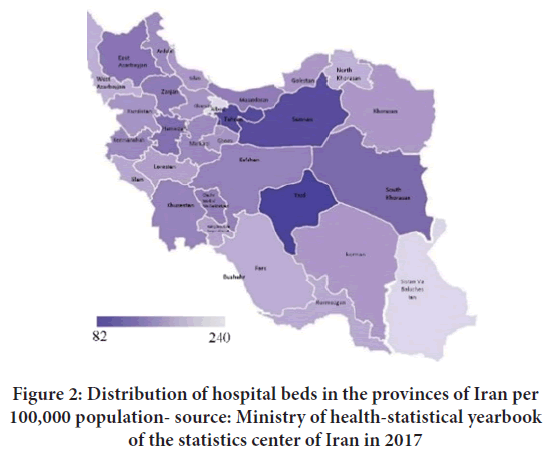
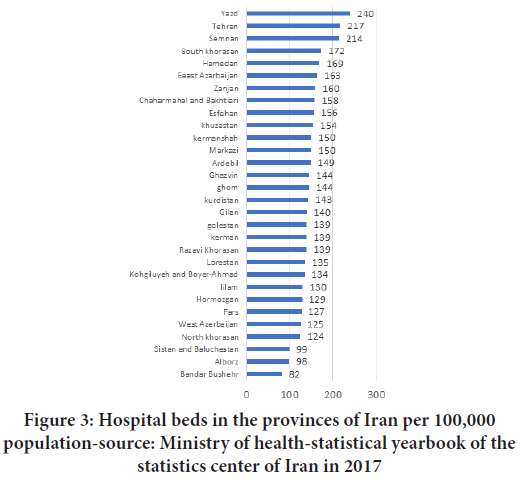
Active hospital bed per capita in Iran: One of the important indicators of treatment is per capita hospital bed. Using this index, a picture can be obtained of the level of preparedness of each region in the face of crisis. According to the data available in the World Bank Data Center, the per capita number of hospital beds in the world until 2011 is 271 beds per 100,000 people, while in Iran this rate was 155 beds until 2017 (IBRD-IDA, 2021). According to the statistics published on the data site, among the provinces of Iran, Yazd, Tehran and Semnan, respectively, have the highest rate of hospital beds in terms of population (IOD, 2019). The per capita hospital bed in Yazd is 240 beds, in Tehran 217 beds and in Semnan 214 beds per 100,000 populations. The provinces of Sistan and Baluchestan, Alborz and Bushehr are also the most deprived provinces in this regard. The per capita hospital beds in these three provinces are 99, 98 and 82 beds per 100,000 people, respectively. The average per capita hospital bed in the whole country is 155 beds per 100,000 people. The interactive map opposite shows the number of active hospital beds per 100,000 populations (IOD, 2019) (Figures 2 and 3).
Figure 2: Distribution of hospital beds in the provinces of Iran per 100,000 population- source: Ministry of health-statistical yearbook of the statistics center of Iran in 2017
Figure 3: Hospital beds in the provinces of Iran per 100,000 population-source: Ministry of health-statistical yearbook of the statistics center of Iran in 2017
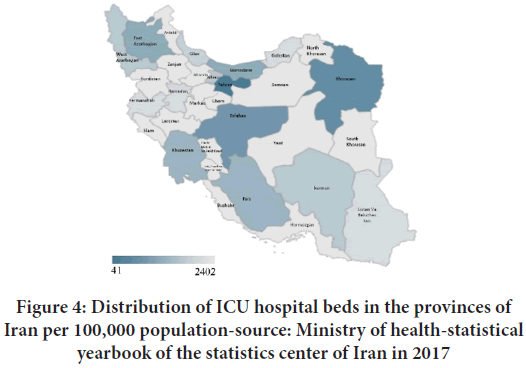
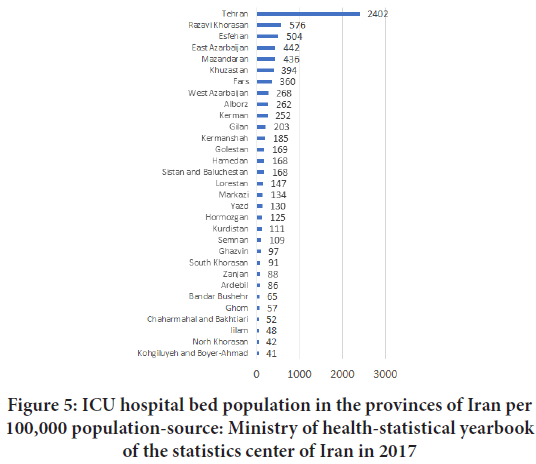
Intensive Care Unit (ICU): The interactive map opposite shows how 8,212 Intensive Care Units (ICUs) are distributed in the provinces of Iran. More than 2,402 ICI beds are located in Tehran, about 30% of the total available beds in the country. After Tehran, Khorasan Razavi, Isfahan and East Azarbaijan provinces are in the next positions with 576, 504 and 442 ICU beds, respectively. At the bottom of the table are Kohgiluyeh and Boyer-Ahmad provinces, North Khorasan and Ilam, according to which the total number of intensive care beds is 41, 42 and 48 beds, respectively (IOD, 2019) (Figures 4 and 5).
Figure 4: Distribution of ICU hospital beds in the provinces of Iran per 100,000 population-source: Ministry of health-statistical yearbook of the statistics center of Iran in 2017
Figure 5: ICU hospital bed population in the provinces of Iran per 100,000 population-source: Ministry of health-statistical yearbook of the statistics center of Iran in 2017
Comparison of health infrastructure in Iran and the world
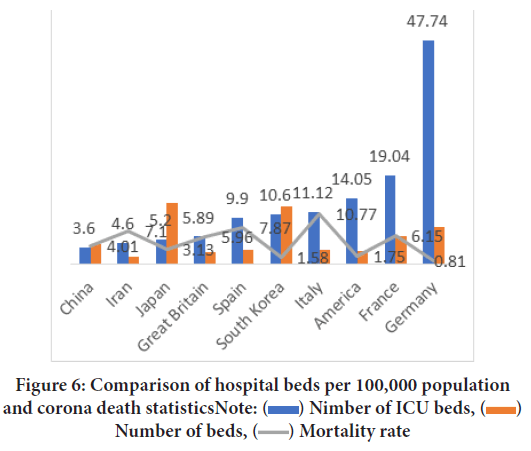
The global COVID-19 mortality rate is affected by many factors, including hospital bed capacity, ICU bed capacity, and negative pressure isolation. Research has shown that higher-income areas in the world have more acute care, ICUs, and hospital beds than low-income areas, so corona deaths are much lower than in other countries (Sussman N, 2020) (Figure 6).
Figure 6: Comparison of hospital beds per 100,000 population
and corona death statistics Note:  Nimber of ICU beds,
Nimber of ICU beds,  Number of beds,
Number of beds,  Mortality rate
Mortality rate
Therefore, this research shows that the capacity of hospital beds has a direct effect on the mortality rate of COVID-19. It can also indirectly reduce transmission by transporting infected people from the home to hospitals. Therefore, with the spread of infectious infection and increasing the occupancy of hospital beds, the mortality rate will increase (Sussman N, 2020).
According to global statistics and based on the experience of China, 4.7% of coronary heart disease patients need intensive care. According to our world in data site and the OECD in 2020, Germany has 47.74 beds in the intensive care unit per 100,000 people, which is the highest per capita ICI bed rate in the world. After Germany, France with 19.04 beds and the United States with 14.05 beds and then Italy with 11.12 beds have the most beds in the intensive care unit. South Korea is ranked 10th in the world with 10.6 ICU beds per 100,000 people. Iran, with a population of 83 million in 1398, has a total of 8,264 ICU beds throughout the country; that is about 4.6 ICU beds per 100,000 people (OECD, 2020; Our World in Data, 2020).
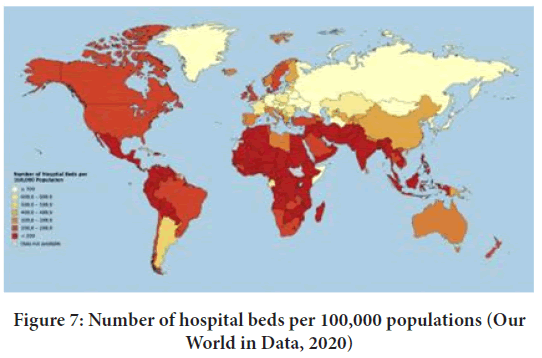
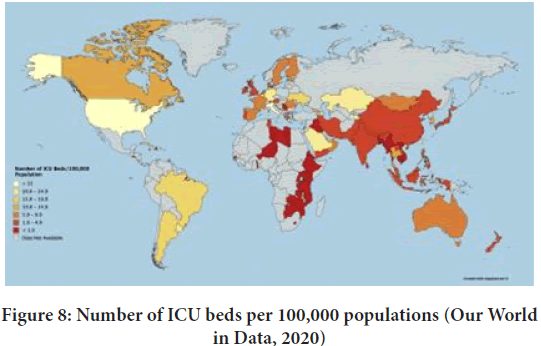
The lack of health infrastructure in the Iranian health system manifests itself during crises such as floods, earthquakes and the Corona pandemic. With the advent of the COVID-19 pandemic and the lack of hospital beds, the capacity of hospitals to receive coronary patients is saturated. Unfortunately, many patients are returned home and lose their lives due to lack of hospital space. In comparison with Iran compared to other countries, the number of hospital beds per 100,000 populations is less than 200, and ICU beds are between 1-1.49 (Figures 7 and 8).
Figure 7: Number of hospital beds per 100,000 populations (Our World in Data, 2020)
Figure 8: Number of ICU beds per 100,000 populations (Our World in Data, 2020)
COVID-19 crisis management in Iran
In this regard, the Ministry of Health of Iran announced 27 hospitals in Tehran and other cities as referral hospitals for the reception of COVID patients. The first step of these centres was to completely evacuate the hospital from hospitalized patients and prepare the wards for the reception of COVID patients and close the clinics. The treatment center then launched an emergency response program, and at the same time formed several working groups, including an emergency team, a prevention and control team, an emergency medical team, a security and training team. Establishing a fever clinic has been one of the most important measures of these hospitals. The hospital also suspended all non-emergency admissions and stopped all non-emergency surgeries (Jebelli B, et al., 2020).
After a short period of time, large convalescent homes were built in Tehran and some other cities in order to provide proper health services to COVID-19 patients. With the spread of the disease and the increase in the number of referrals during the epidemic, the number of hospitals for admission of patients was increased. Also, with the participation of other sectors, sports spaces, hotels, commercial centres and exhibitions were used as the setting up of convalescents (MHME, 2020).
We see in our country that in a situation where there is a health network in our big cities, with an accident, this network is used in normal conditions in excess of capacity and the necessary instructions and forecasts for the situation. There are no crisis causes the death toll in natural crises to rise. Hospitals alone are not responsible in times of crisis. And we have to look at this issue from a bigger perspective. During coronation, patients who go to the hospital for other illnesses develop coronary heart disease, and the hospital is unable to provide proper services to other patients. Hospitals themselves are a source of pollution.
Quick answer-global solutions
The countries with the highest number of COVID-19 conflicts are the United States, Italy, China, Spain, Germany and Iran (WHO, 2020). China builds core strategies based on effective and coordinated social distancing system, law-based quarantine solutions, scientific findings, and immediate interventions (including rapid patient detection, rapid reporting, rapid isolation, and immediate treatment) institution (MHME, 2020).
Japan has experienced three major policies-rapid diagnoses of patients, improvement of intensive care units, and empowerment of patient care systems, given that it has experienced 1,191 positive cases and 46 deaths from coronary heart disease over the past two weeks. He put acute respiratory on his agenda, and in addition to providing medical equipment and devices such as ventilators, ECMOs, and community lifestyle modifications were other Japanese proposals. At the same time, Japan is working to reduce the effects of economic and social devastation, improve the quality of hospital services and increase special beds (MHME, 2020).
South Korea has so far received 9,300 positive cases, 139 deaths (1.5% of deaths) and 4,500 recovered cases, and the coronation situation in the country is improving rapidly. Prompt and timely screening using the primary health care system as well as the use of primary health care to treat mild cases is one of South Korea’s main strategies. Also, people’s participation based on transparency and open expression by the government, justice in public access to diagnosis and treatment without any discrimination based on gender, ethnicity and location, close cooperation between headquarters and local governments, epidemiological research, optimal use of resources and strengthening the care system. It is also considered in the prevention and control of the disease (MHME, 2020).
Singapore has 683 positive cases, two deaths and 172 improvements so far. One of the main strategies in this country is the observance of compulsory social distance as a law, the ability of service providers to manage inpatients and outpatients, as well as supporting all health care workers who are working in the field of prevention or treatment. Strengthening the management of private hospitals, supporting service-providing manpower, and establishing isolated community-based centres are also among Singapore’s future plans (MHME, 2020).
Various solutions have been tested in the world to deal with the sudden increase in demand for treatment in such cases. Here are some key strategies: In order to overcome the saturation of space in existing hospitals, three main strategies have been adopted, each of which is explained below. We pay from them.
Prefabrication-portable field hospital: In 2003, with the outbreak of SARS, Xiaotangshan SARS Hospital in Beijing was built in just 6 days. In 2020, with the outbreak of the coronavirus, the Chinese government quickly concluded that local hospitals would be overwhelmed. Therefore, in less than two weeks, two private hospitals in Huoshenshan (1000 beds with 30 ICU units) were built in just 9 days and Leishenshan (1600 beds) in 10 days using prefabricated buildings for COVID-19 patients in Wuhan (Tejarat News, 2019) (Figure 9).
Figure 9: Hoshshan hospital from a far (Tejarat News, 2019)
Changing the use of existing buildings: This strategy is usually implemented in buildings that can become an emergency for crisis situations. Such as shopping malls, airports or schools were temporary treatment centers for 19 patients. However, these buildings have limited capacity for high-level surgery or diagnosis, lack of specialized support services, and remoteness from the main hospital (Capolongo S, et al., 2020).
Construction of closed hospital wards: This solution is mostly used in developed countries that design, build and even equip a department in times of crisis. But in the current situation in Iran and the lack of beds and ICU, this solution is not practical and economic for our country. But the US Department of Health and Human Services’ research and treatment quality agency recommends this solution for situations where the accident occurred with high casualties or requires quarantine.
Background research
In a study by a team of physicians and designers from Mount Sinai Children’s Hospital, MASS Architecture Group, and Ariadne Laboratories, fundamental changes in the spatial infrastructure of Mount Sinai Hospital, USA, using infection control guidelines and evidence-based design to address the prevalence of COVID-19 was determined. These studies were performed on three wards dedicated to COVID-19 patients, including paediatrics, adult surgery, and adult ICU. The measures taken are-
• Conversion of 260 hospital rooms into negative pressure isolation rooms using changes in the spatial structure of the ICU and the integration of the rooms and the creation of seamless walls and doors
• Spatial divisions of the plan based on the risk of transmission to red, green and orange thermal codes
• Use of HEPA air filters in each room
• Use of PPE personal protective equipment and recycling bins assigned to each unit and use of elevators for transporting infectious waste
• Reducing nursing stations and minimizing staff contact with patients using nurse computer stations in the hallway (Ariadne Labs, 2020).
Capulongo S, et al. provide a list of strategies for building intensive care capacity and reviewing design strategies for health care design for flexible nursing facilities. Strategies are organized into two categories:
• Design
• Operational
Design phase strategies are-
• Site location
• Physical structure
• Flexibility
• Physical program
• evidence-based design
Operational phase strategies are-
• Regional health centers
• Patient safety
• HVAC and air conditioning
• Finishing and joinery surfaces
Use of digital technologies (Capolongo S, et al., 2020).
Materials and Methods
In the first stage of the research, using banks and information resources and related resources that were extracted in the field of reviewing hospital plans after the COVID-19 pandemic, using related keywords. Keywords include SARS-CoV, SARS-CoV-2, COVID-19, Hospital, Healthcare facilities; reshape hospital design, redesign hospital space, infection design, Intensive Care Units (ICU). Google scholar was searched and the first 10 pages of URLs found (a total of 100 URLs per site for each keyword) were checked and the relevant information was extracted manually after overlapping. Then, searches were made on reputable domestic and foreign corporate sites and electronic databases during the period August 2003 to 2020. The database included search engines (research gate science direct, health scope) and Google Scholar search engine. Internal databases included (Iran doc, meg Iran, scientific database, Civilica, Liman consulting engineers internal journal). In the next stage, the obtained criteria were categorized accordingly.
Results
In order to determine the importance of the obtained criteria, a questionnaire was designed. In this study, content validity refers to the extent to which the criteria selected in the method represent the whole community of criteria that can be prepared from the subject of hospital design. To evaluate the validity of the questionnaire, CVR content validity ratio and CVI content validity index were used; thus, in order to determine the content validity ratio, the questionnaire was asked by 3 specialists and hospital engineers of Parsazeh Construction Company (1 architect, 1 civil engineer and 1 mechanical installation engineer). They were asked to review each item on a 3-part scale (necessary, useful, but not necessary and not necessary). The number obtained for all questions was greater than the Leucheh table number (0.62), so it indicated that the existence of relevant questions with a high level of significance according to the CVR formula is necessary and important in this tool. To determine the content validity index, a questionnaire was used to calculate CVI and three criteria of relevance or relevance, simplicity or fluency, and clarity or clarity were calculated based on a 4-part Likert scale. The results showed that all CVI score questions score above 1.16 (minimum acceptable score for the content validity index), so they were deemed appropriate. The reliability of the questionnaire was also calculated using Cronbach’s alpha coefficient through retest and correlation coefficient. Thus, the questionnaires were given to ten respondents two weeks apart, which the reliability coefficient obtained in two runs was higher than 1.19 and showed the high reliability of the research tool. Of the total number of respondents (54 people), 6 were doctors (11.1%), 15 were architects (hospital designer) (28.8%), 14 were mechanical facility engineers (hospitals) (25.9%) and 19 were civil engineers (Were hospital contractors (35.2%).
It should be noted that the physician participants in this study included the head of the Semnan medical system organization and specialists of Mahdieh Hospital, as well as the participating engineers from the personnel of Parsazeh co., The executive organization of government and public buildings and facilities co., Khaneh Sazi Iran project and management co., Liman consulting engineers co. and Mabna consulting engineers co.
In this study, in order to weigh the criteria, Shannon entropy method has been used. The most important advantages of this method are: the possibility of simultaneous use of multiple quantitative and qualitative characteristics, ease and simplicity of use, the possibility of changing the input information, expressing the results in this chapter after collecting and summarizing data using Shannon entropy statistical techniques and TOPSIS analyzes data using and using excel version 2013 software (Table 1).
| Characteristics | Abundance | percentage |
|---|---|---|
| Sex | ||
| Female | 17 | 30.90% |
| Male | 38 | 69% |
| Career | ||
| Physician | 6 | 10.90% |
| Architect (hospital designer) | 16 | 29.10% |
| Mechanical engineer | 14 | 25.50% |
| Contractor (hospital contactor) | 19 | 34.50% |
| Education | ||
| Diploma | 0 | 0 |
| BS | 40 | 72.70% |
| MA | 8 | 14.50% |
| DR | 7 | 12.70% |
Table 1: Demographic characteristics of the respondents
Discussion
Inferential analysis of data
After the descriptive analysis of the data, we proceed to the inferential analysis of the data. In inferential analysis, variables as well as research objectives are evaluated and tested.
Weighting of indicators based on Shannon entropy technique
Entropy is a very important concept in social sciences, physics and information theory. Once the data of a decision matrix is fully specified, the entropy method can be used to evaluate the weights. The clear idea above is that the greater the scatter in the values of an index, the more important that index is. Entropy in information theory is a measure of uncertainty expressed by the definite probability distribution P_i. The entropy calculation steps are as follows-
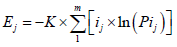
K is a constant value and is calculated from the following equation:

M is the number of decision matrix options. And:

Calculate the amount of uncertainty:

Finally, the weights are calculated as follows:

These calculations are used for the following decision matrix. It should be noted that in the entropy method, positive or negative indicators will not have an effect on the method of calculating weights. The output of the Shannon entropy test is shown in the table below (Table 2).
| Row | 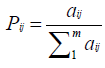 |
Indicators | |
|---|---|---|---|
| Weight | Entropy value | ||
| 1 | 0.35029 | 7.86002 | Architect (hospital designer) |
| 2 | 0.07879 | 1.76798 | Mechanical engineer |
| 3 | 0.33706 | 7.56313 | Contractor (hospital contactor) |
| 4 | 0.23387 | 5.24769 | Physician |
Table 2: Shannon technique output
Ranking using the TOPSIS technique
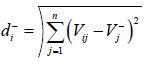
This method was proposed in 1981 by Huang and Eun. In this method, the factor or option is evaluated by an individual or a group of decision-makers. This technique is based on the concept that each selected factor should have the shortest distance with the positive ideal factor (the most important) and the maximum distance with the negative ideal factor (the least important factor). In other words, in this method, the distance of a factor with the ideal factor is measured positively and negatively, and this is the criterion for grading and prioritizing the factors. The steps of this method are-
Create a decision matrix: To form a decision matrix, we must first obtain the matrix of pairwise comparisons of factors for each index. To do this, according to experts, we bring the value and importance of each factor compared to other factors in line with the index presented in the square matrix. The principal diameter of this matrix is 1 (the importance of each factor relative to itself is 1). In this part of the research, since the pairwise comparison matrix was a 38 × 38 square matrix and could not be displayed on the page; therefore, the decision matrix is given directly. Using linear normalization and linear averaging methods, the pairwise comparison matrix is converted into a vector and placed in the columns of the decision matrix.
Create a pairwise comparison matrix to find the weights of the criteria: To measure the priority of each criterion, we use the pairwise comparison matrix. This means that we use it in terms of several experts and put the importance of each criterion in a matrix compared to the other criterion. Certainly, the main diameter of this matrix is 1 and is square. Any element above the main diameter is inversely below the original diameter. The weight of each criterion is determined by linear normalization and then linear averaging. In this study, due to having a criterion (impact rate), the weight of the criterion is equal to 1.
Normalize the decision matrix: In order to be comparable, the decision matrix is converted to a normalized matrix or an unbalanced matrix ( N1 ) using equation.

In this regard, (r) are the scores that the indicators have assigned to each of the criteria.
Create a rhythmic matrix: To obtain a rhythmic matrix, multiply each of the columns of the normalized matrix by the weight of the same column. In this study, because the criterion weight of the “impact rate” was 1, the matrix and the normalized matrix are the same.
Determining the positive ideal factor and the negative ideal: At this stage, the criteria that have been identified as the most important and least important criteria by the respondents should be identified. In other words, for positive indices, the positive ideal is the largest value of v and the negative ideal is the smallest value of v, also for negative indices, the positive ideal is the smallest value of v and the negative ideal is the largest value of v. Equations 2 and 3 state this.
In these relationships, there is j for positive indicators and J for negative indicators (Table 3).
| Positive deal (A+) | Negative deal (A-) |
|---|---|
| 0.051 | 0.037 |
| 0.013 | 0.007 |
| 5.00% | 0.036 |
| 0.034 | 0.025 |
Table 3: Positive and negative ideals
At this stage, the distance between each of the options from the positive ideal and the negative ideal is determined according to the following equations.
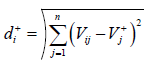
Where i=1,2,…, m
The above equation denotes the distance of options from the positive ideal
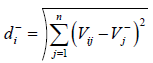
Similarly, this equation implies the distance of options from the negative ideal and calculates the degree of proximity of each factor to the positive ideal and negative ideal. At this stage, the degree of proximity of each indicates the positive ideal and the negative ideal. CL is obtained according to the mentioned equation-
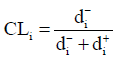
Calculating the proximity of indicators to ideal factors
At this point the options are ranked by value; In other words, any option that is higher will get a better rating, because it is further away from the negative ideal and also closer to the positive ideal.
Conclusion
Future approaches in the design of medical centers
Flexible design: Corona showed us how much I accepted flexibility in critical situations; Flexible environment is of great importance for maximum use of the environment and increase of facilities in pandemic. Combining proprietary flexibility with design allows architects to plan for the control of unforeseen events in the building in a future beyond the legal delivery period. In this regard, designing free plans in emergency departments, clinics and hospitalization that will help to appear by providing a wide space fit, to increase the space (without the need for a physical building). Restricting workspaces and space by partitions will also create social distance between people. In this regard, by reducing the waiting spaces and allocating more space to the emergency department, hospitalization and ICU will be available.
• Emergency and inpatient admissions and ICU cases are important, including:
• Emergency admission to the emergency hospital to increase information
• Eliminate all non-emergency functions of the hospital and the possibility of converting them to the required functions of the emergency
• Predict areas for emergency screening
• Prediction under the influence of opinion in the emergency
• Predicting separate sampling units in the emergency
• Changing the hospital use department and turning it into an isolation of airborne infection with dual use
• Reduce patient travel in the emergency room
• Predicting fever clinic in the emergency room
• Evacuation and relocation departments in the hospital if necessary
• Separation of physician from patient
• Body temperature control
• Collect samples
• Daily screening of service personnel
• Triage/outpatient clinic for acute respiratory infections
• Pharmacy forecast in fever clinic
• Consider a free plan to convert ICU beds to negative pressure isolators
• Convert hospitalized rooms to negative pressure isolators
• Predict multi-purpose spaces
Increase ICU admission capacity and negative pressure isolation: The lack of health infrastructure in the Iranian health system has manifested itself with the advent of the Corona pandemic. With the lack of hospital beds and injustice in the distribution of beds in the provinces, the capacity of hospitals to receive coronary patients is saturated, and unfortunately many patients return home and lose their lives due to the lack of hospital space.
In this regard, converting public and private buildings such as schools, universities and mosques into treatment camps and forecasting out-of-town locations to set up field hospitals with the help of prefabricated structures can help reduce the burden of visits and occupancy of beds. Hospital, but it should be considered that increasing the number of hospital beds and building medical centers in deprived areas to reduce the number of visits to provincial centers and the spread of infection should be one of the basic measures of the government.
Improve prevention of the spread of infection: According to the ministry of health, many people with COVID-19 have symptoms of coughing and sneezing that can infect a hospital at least two meters away. On the other hand, the accumulation and hospitalization of these patients in enclosed spaces can cause the spread of infection and in the absence of negative pressure; COVID-19 virus can be spread to other parts of the hospital. Therefore, in order to maintain the health of medical staff and reduce the burden of pollution in hospital units and enclosed places used, it is necessary to pay attention to the ventilation system and how the air moves.
• In this regard, the following items are important in designing the plan.
• Review of the air conditioning control system
• New arrangements for fresh air
• Installation of separate ventilation fans in the corona patients
• Use of HEPA filter in the air outlet of hospital rooms
• Using a combined system (natural and mechanical) in the hospital ward
• Internal ventilation control by intelligent systems
• Separating the hospital lobby and accepting it from the ventilation cycle and turning it into a semi-open space
• Filtering the exhaust air from the building, separating the emergency triage of the hospital and outpatient wards from other wards
• Implementation of medical gas splints
• Implementation of PTS system
• Separation of infectious sections from other sections
• Designing a separate route for personnel with the allocation of corridors and elevators
• Anticipation of hand washing stations and Personal Protective Equipment (PPE) at the entrances of the rooms
• Predicting the entrance space of a hospital with negative pressure
• Predict specific areas for families to visit patients
• Anticipation of separate operating room, recovery and dialysis for patients in the infectious ward
• Review plans to reduce traffic in inpatient wards
• Isolation of patients admitted to the inpatient ward upon arrival
Changing the hospital design approach from short-term to community-based care: In near future, the hospital design approach will change to short-term stay and community-based care. This will become part of the hospital infrastructure by reducing the number of in-person visits and remote monitoring of patients with the help of tele-health and will reduce the number of in-person visits and hospitalizations. In this case, better patient tracking and acceptance with a capable system will lead to the creation of a new effective outpatient system.
References
- Gan WH, Lim JW, Koh D. Preventing intra-hospital infection and transmission of coronavirus disease 2019 in health-care workers. Saf Health Work. 2020; 11(2): 241-243.
[Crossref] [Google scholar] [Pubmed]
- Bhagavathula AS, Aldhaleei WA, Rahmani J, Mahabadi MA, Bandari DK. Novel coronavirus (COVID-19) knowledge and perceptions: A survey of healthcare workers. MedRxiv. 2020.
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. NEngl J Med. 2020; 382(8): 727-733.
[Crossref] [Google scholar] [Pubmed]
- Arabi YM, Murthy S, Webb S. COVID-19: A novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020; 46(5): 833-836.
[Crossref] [Google scholar] [Pubmed]
- Euro surveillance editorial team. Note from the editors: World health organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro surveillance. 2020; 25(5): 200131e.
[Crossref] [Google scholar] [Pubmed]
- Dolinger M, Marsh A. Architecture can heal: Spatial literacy to protect COVID‐19 healthcare workers. Ethnogr Prax Ind Conf Proc. 2020; 1: 324-337.
- Redesigning hospital spaces on the fly to protect healthcare workers takeaways next steps. Ariadne Labs. 2020.
- Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020; 582(7813): 557-560.
[Crossref] [Google scholar] [Pubmed]
- Capolongo S, Gola M, Brambilla A, Morganti A, Mosca EI, Barach P. COVID-19 and healthcare facilities: A decalogue of design strategies for resilient hospitals. Acta Biomed. 2020; 91: 50-60.
[Crossref] [Google scholar] [Pubmed]
- Pueyo T. Coronavirus: Why you must act now. Politicians, community leaders and business leaders: What should you do and when. 2020.
- Hospital beds (per 1,000 people). The World Bank | Data (IBRD-IDA). 2020.
- Corona outbreak map in Iran and its comparison with hospital facilities. Iran open data (IOD). 2020.
- Sussman N. Time for bed (s): Hospital capacity and mortality from COVID-19. Covid Econ. 2020; 11: 116-131.
- Intensive care beds capacity. OECD. 2020.
- Intensive care beds per 100,000 people, 2020. Our World in Data. 2020.
- Jebelli B, Varahram M, Razlighi MS, Palizdar M, Ghazanchaei E. Management Strategies to control the COVID-19 crisis in Masih Daneshvari Hospital, Tehran, Iran. J Mil Med. 2020.
- Corona virus prevention and control guidelines. Ministry ofHealth, Medicine and Education (MHME). 2020.
- WHO report: Global research emergency coronaviruses 2020. World Health Organization (WHO). 2020.
- Report of zoom conference about COVID-19. Ministry of Health and Medical Education of the Islamic Republic of Iran and L. Asadi. 2020.
- How did China make two hospitals a day for a new corona virus. Tejarat News. 2019.
Author Info
Babak Fakhim1 and Zahra Jahed Bozorgan2*2Department of Landscape Architecture, Shahid Beheshti University, Tehran, Iran
Citation: Fakhim B: Determining and Prioritizing Effective Design Indicators in COVID-19 Pandemic Response
Received: 30-Jun-2022 Accepted: 22-Jul-2022 Published: 29-Jul-2022, DOI: 10.31858/0975-8453.13.7.468-475
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3