Research Article - (2022) Volume 13, Issue 2
Abstract
Aim of the study: The main aim of this study is to analyze the influence of obesity over the intraoperative and post-operative evolution, in the context of Total Laparoscopic Hysterectomy.
Material and methods: The study developed in the II nd Surgical Clinic of the Timisoara County Emergency Hospital Timisoara between 1st of January 2017 1st of January 2019 and it was applied to a general batch of 29 women patients diagnosed with benign pathology of the uterus and adnexa.
Results: The general batch we considered necessary some type of categorization of the women patients based on the BMI (Body Mass Index): Group A: BMI=19.5 kg/m2-24,9 kg/m2; Group B: BMI=25-29.9 kg/m2; Group C: BMI>30 kg/m2. A positive moderated co-relation between the number of the comorbidities and the BMI (r=0.493, pË, 0.05). Somehow self-explanatory, it was emphasized the fact that group B and C which contained mostly patients with the BMI limit over the usual one, it was remarked a proportional increase of the comorbidities at the same time with the increase of the BMI. A strong positive co-relation between the BMI and the intervention time (p=0.047), therefore, those two being tied by proportional increase relation. In this way we obtained a statistically significant co-relation between BMI and the post-operative complications (pË, 0.05) but with a low number of major complication on the general batch.
Conclusions: By analyzing the comorbidities and the post-operative evolution, minor differences were encountered between the study groups, and it was demonstrated that there is no reason to see a high BMI level as an obstacle in performing TLH.
Keywords
BMI, Comorbidities, Complications, Intervention time
Introduction
Obesity represents nowadays a high-level problem worldwide with social, economic, and medical implications (Mokdad AH, et al., 2001; Mokdad AH, et al., 2000; Mokdad AH, et al., 1999). Therefore, during the last years a true revolution has arisen regarding the way the suffering patients were to be treated from a surgery point of view. What we can confirm is that the ay laparoscopic and robotic surgery has evolved is truly amazing in such a way that the next decade is considered to become a gold standard regarding the way surgery will be performed (Hubert HB, et al., 1983; Lew EA and Garfinkel L, 1979; Gomel V and Taylor PJ, 1995). Moreover, because of practicing these methods, obese patients become a very special category in the surgical fields (National Institutes of Health, 1985; Pi-Sunyer FX, 1991; Manson JE, et al., 1990).
On the other hand, some authors considered obesity as a contradiction to everything that laparoscopic surgery means but with the release of more other studies that demonstrated the veracity and reliability of these methods, things have lessened a bit from their end. In 1989, Reich H was the one who performed the first total hysterectomy by means of laparoscopic surgery, method which was, however, improved over the years with the aim of expanding the applicability of this approach (Pitkin RM, 1976; Safran D, et al., 1993; Reich H, 1992; National Heart, Lung, Blood Institute, National Institute of Diabetes, Digestive, Kidney Diseases (US), 1998; Koh CH, 1998).
The main aim of this study is to analyze the influence of obesity over the intraoperative and post-operative evolution, in the context of Total Laparoscopic Hysterectomy.
Equipment and Method
The study developed in the II nd Surgical Clinic of the “Pius Brinzeu” County Emergency Hospital Timișoara between 1st of January 2017-1st of January 2019 and it was applied to a general batch of 29 women patients diagnosed with benign pathology of the uterus and adnexa, ASA score I-IV for whom a surgical intervention was needed, more exactly that of Total Laparoscopic Hysterectomy (TLH) and also of bilateral oophorectomy. The post-operative analysis of the patients was done inside of the clinic and it took place at: 1 month postoperative, 3 months, 6 months and 1 year and in order to obtain the most precise results regarding THL operative, the following inclusion criteria was established at the batch’s level:
• Age over 18
• Patients with uterine and/or ovarian benign pathology.
Exclusion criteria were:
• Patients with uterine and/or ovarian malignant pathology
Under the permission of the Ethic Commission, all data was input in a database starting with 1st of January 2017, where the information was memorized and organized in different tables with the help of Microsoft Excel program and the Rapid Miner program.
Within the general batch we considered necessary some type of categorization of the women patients based on the BMI and according to the criteria set out by the National Heart, Lung and Blood Institute (NHLBI). In this way we obtained study groups:
• Group A: BMI=19.5-24,9 kg/m2
• Group B: BMI=25-29.9 kg/m2
• Group C: BMI>30 kg/m2
Each patient experienced THL surgery and inside each group the following factors were analyzed: age, time spent in the hospital, size of the uterus in longitudinal axis, adnexal changes, the size of the skinfold, other comorbidities, presence/absence of cicatricial abdomen, the resume of the post-operative transit/movement, other complications, the suppression of drainage, reason of admittance in the hospital, ASA(American Society of Anaesthesiologists) score, result of the histopathologic test, how long the intervention took, quantity of lost blood during surgery and level of Hemoglobin both pre- and post-operative. With the help of the data obtained, it was possible to establish some ways of comparison between the 3 groups.
From a technical point of view, we used the following equipment and materials: optical trocar (10 mm/15 mm Ethicon Surgery) placed at umbilical level, 2 trocars of 5 mm (5 mm/10 mm Ethicon Surgery) located left and right paramedian at 4-5 cm under umbilical level, prehension clamp, Maryland forceps, 5 mm Ligasure clamp, AC Veress/Hasson cannula, monopolar hook, Schroeder uterine clam, respectively Clermont-Ferrand (Karl Stortz) manipulator clamp and uterine morcellator (Gyncare X-Tract Tissue morcellator; Ethicon).
For this type of surgery, i.e., THL surgery the standard position is the Lloyd-Davies one, where the level of pneumoperitoneum is between 12- 16 mmHg, depending on BMI, and the antibiotic prophylaxis is administrated through a mono-doses of 3rd generation cefotaxime 30-60 minutes pre-operative.
The method used for THL is highly similar with the classic method. After completing the pneumoperitoneum, the next step is the comprehensive exploration and locoregional stage, followed by sectioning the lombo-ovarian pedicles using the Ligasure clamp; from here on, the next step is sectioning of the anterior folds of the broad ligaments, these incisions getting united at the uterine isthmus level. Next stage consists of removing the bladder in embryologic plane, which will afterwards facilitate a safely approach of the uterine vascular network without interfering the ureters, and of the anterior colpotomy. The uterus is orientated upwards with the help of the Clermont-Ferrand manipulator, followed by the incision of the back sheets of the broad ligament, the sectioning of the uterosacral ligaments and of the peritoneum, which covers the posterior vaginal cul-de- sac. The next practice after the interception of the uterine pedicles is the circular cordotomy at the vaginal cul-de-sacs level, all this through using the monopolar hook, the section level being guided by the side of the uterine manipulator. The extraction of the surgical piece is done transvaginally being followed by laparoscopic colporrhaphy. In a Total Laparoscopic Hysterectomy, a small uterus can be removed whole through the vagina at the end of the procedure. If the uterus is large the tissue must be morcellated before extraction. Power morcellation has come under scrutiny recently because of concerns regarding the dissemination of uterine tissue. As suggested by Wright, dissemination of the cells during morcellation could be prevented with an appropriate preoperative workup that include a history and physical exam (uterine size), up to date cervical screening, and an endometrial biopsy if indicated.
In 2015, Winner B, et al. found that morcellation within an insufflated bag took twenty minutes longer than uncontained morcellation, with no increase in complications. And in 2016, Cohen et al. published a prospective in vivo study in which uterine tissue was stained with dye before morcellation, and the pelvis was inspected after morcellation (Mokdad AH, et al., 2001; Mokdad AH, et al., 2000; Mokdad AH, et al., 1999). Dye/tissue leakage was noted in 7 out of 76 cases, although the authors noted that most of the dye leakage was likely due to the method of introduction; actually spillage of tissue fragments was only noted in one case. Together, these studies indicate that power morcellation within a containment bag is feasible and effective, although efforts should be made to improve the technique. In 2016, the FDA (Food and Drug Administration Act) approved the first bag for contained morcellation (Hubert HB, et al., 1983; Lew EA and Garfinkel L, 1979; Gomel V and Taylor PJ, 1995). We use the morcellation technique if the long axis of the uterus is over 15 cm.
We have generated both a univariate and bivariate analysis for the 3 groups of study, respecting the parameters of each case. The differences between these 3 groups were evaluated using the Pearson coefficient, respectively the Fisher test, by establishing some reference values.
Results
The general batch of the study was made of 29 diagnosed patients with benign and pathology of the uterus and it was developed in the Surgical Clinic II of the “Pius Brinzeu” County Emergency Hospital Timisoara. Their age range was between 41 and 78 years old, with the average of 53.96 years. The average admission time was of 4.79 days and the BMI level of 29.1 kg/m2 (Figure 1).
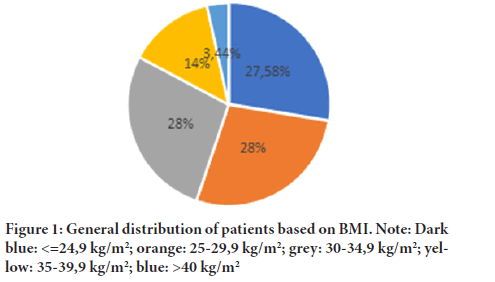
Figure 1:General distribution of patients based on BMI. Note: Dark blue: <= 24,9 kg/m2; orange: 25-29,9 kg/m2; grey: 30-34,9 kg/m2; yellow: 35-39,9 kg/m2; blue: >40 kg/m2
From the admission’s reasons point of view, we have obtained the following results: 82.75% of patients presented pains on the lower abdomen, 62.06% presented metrorrhagias, 27.58% menometrorrhagias, 10.34% spaniomenorrhea, 17.2% constipation, 20.6% polyuria, 10.34% fatigability. As a result of the clinical-paraclinical investigations, we processed data with mandatory value, such as: the dimension of the uterus in longitudinal axis, the evaluation of the annexes, the level of the skin fold, associated comorbidities, presence/absence of the cicatricial abdomen, restarting point of the intestinal transit, suppression of drainages, the result of the histopathological examination performed postoperative. We will present the general data regarding these parameters of the analysis process so that: when reporting to the dimension of the uterus in longitudinal axis which was basically determined both preoperative and postoperative, we have obtained an average value of 11.37 cm, the minimum of 6 cm, respectively the maximum of 25 cm. It was emphasized the fact that 34.4% of the patients presented ovarian cyst on the left side, associated with an average dimension of 3.1 cm. On the other hand, 37.9% were carries of ovarian cyst on the right side with an average dimension of 3.8 cm Moreover, as a result of the fallopian tubes analysis, it was concluded that 10.34% of our patients presented unilateral/bilateral hydrosalpinx (Figure 2).
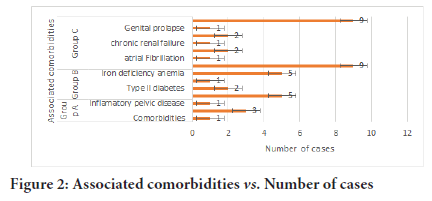
Figure 2:Associated comorbidities vs. Number of cases
From the point of view of the cicatricial abdomen, which was manifested to 24.14% of the patients (7 cases), in 75.86% cases (22 patients) can be discussed about intervention performed on the native abdomen. Moreover, regarding the post-operative recover, the average was of 27.7 hours while the drainage suppression was performed on an average of 35.1 post-operative. By analyzing the main comorbidities manifested inside the general batch, we obtained the following data: 51.72% (15 cases) presents HTA (Health Technology Assessment), 3.44% (1 case) atrial fibrillation, 6.89% (2 cases) congestive heart failure, 6.89% (2 cases) genital prolapse, 3.44% (1 case) chronic renal insufficiency, 58.6% (17 cases) iron deficiency anemia, 3.44% (1 case) pelvic inflammatory disease, 13.79% diabetes mellitus type II, 10.34% (3 cases) hypothyroidism, 37.93% (11 cases) hepatosteatosis. The ASA score at the batch’s level had the average of 2.5 and from the point of view of the histopathologic test we have obtained the following results; It can be easily observed the predomination of the benign pathology (angioleiomyoma, fibro angioleiomyoma, leiomyoma, adenomyosis) in 90% of the cases and a 10% of the malignant one (adenocarcinoma) after the HP exam. The average time of the intervention was of 118 minutes.
We considered necessary the division of the patients in 3 groups of study based on the level of BMI, so that the A group (27.8%) is made of patients with the age average of 50.1 years, BMI (kg/m2) between 19.5-24.9 kg/m2, with the average level of 23.3 kg/m2.
Group B (27.8%) is made of patients with the age average of 52.1 years old, BMI between 25-29.5 kg/m2 with the with the average level of 27.1 kg/m2.
Group C (44.82%) is made of patients with the age average of 57.4 years, BMI above 30 kg/m2 and with the average level of 33.8 kg/m2. The analysis of the main difficulties between the study groups was done by using the Clavien-Dindo classification.
With reference to the batch of the A group (8 patients, 27.58%), we obtained the following statistics: the average level of BMI was of 23.3 kg/m2; the average of the skin fold of 3.37 cm; the average age of the group was of 50.1 years; average time of admission of 4.25 days and the dimension of the longitudinal axis of uterus 10.25 cm. The clinical-paraclinical data emphasizes the fact that: 62.5% of the investigated patients presented ovarian cyst on the left side associated to the uterine pathology; 50% presented ovarian cyst on the right side and approximately 25% presented bilateral cyst. By analyzing the fallopian tubes, it was revealed 2 cases of unilateral hydrosalpinx. For what concerns the resume of the intestinal transit it took place approximately at 27 hours postoperative, while the suppression of drainage took place after approximately 31.5 hours (± 1,3 h). The average of ASA score at the group level is of 2.25 and by analyzing the Hemoglobin level it was obtained an average level of preoperative HB of 11.7 g/dl and postoperative of 10.9 g/dl. The average of the medical intervention time for the A group was of 106 minutes. As a result of the histopathological test it was observed that 37% of the cases presented as a main pathology the uterine angioleiomyoma and as follows: 25% fibro angioleiomyoma, 13% leiomyoma, 25% adenocarcinoma. We encountered 3 main medical difficulties inside the group A, categorized based on Clavien-Dindo I as it follows: fever 38.4°C (2 cases), functional dyspepsia (1 case), hypokalemia (1 case), their management being conservative.
Within group B (8 patients, 27.58%) the following data was obtained: BMI level was of 27.1 kg/m2 with the average of 4/25 cm for the skin fold. The average age at the batch’s level was of 52.1 years; the time of the admission approximately 4.8 days and the dimension of the longitudinal axis of approximately 14.3 cm. From the clinical-paraclinical point of view, it was emphasized the fact that approximately 37.5% (3 cases) of the patients within group B presented ovarian cyst on the left side, another 37.5% (3 cases) ovarian cyst on the right side and 12.5% (1 case) presented bilateral ovarian cysts. For these patients, the resume of the intestinal transit took more than 28.5 hours, while the suppression of drainage took approximately 33 hours (± 3,2). The average of the ASA score was of 2.5; through the dynamic analysis of the Hemoglobin (HB) level the preoperative level of HB obtained was of 11.6 g/dl while the postoperative one of 10.9 g/dl. The average of the intervention for this group was of 122 minutes.
By analyzing the data obtained through the histopathological test, 50% of the resection parts were fibro angioleiomyoma, 25% uterine leiomyoma, 12% angioleiomyoma and 13% uterine adenomyosis. Within this group, we encountered 3 medical difficulties: 2 Clavien-Dindo grade I and 1 Clavien-Dindo grade III b.
From those patients with Clavien-Dindo grade I, 1 case presented febrile syndrome (39°C) which, based on the section’s protocol, decreased after administrating antipyretic and another one presented a minor hemorrhagic syndrome with approximately 150-200 ml of blood at the drainage tubes level, faded at 24 hours post-operative by administrating hemostatic and coagulation factors. On the other hand, for what concerns the difficulties of grade III b, we encountered a lesion on the right ureter, partial sectioned, approximately 1/3 of its circumference within group C (13 patients, 44.82%) the following data was obtained: BMI level of 33.8 kg/m2 with an average of 5.9 cm of the skin fold; the average age was of 57.4 years; the average period of admission of 5.07 days and the dimension of the longitudinal axis of approximately 10.23 cm. The clinic-paraclinical data emphasized the fact that 15.38% (2 cases) of the patients presented associated ovarian cyst on the left side, while approximately 30.7% (4 cases) ovarian cyst on the right side. The analysis of the fallopian tubes distinguished 1 case of unilateral hydrosalpinx (7.6%). The resume of the intestinal transit post-operative took place approximately at 27.6 hours and the suppression of drainage took approximately after 37.8 hours. The average of the ASA score at the group level was of 2.8. As a result of the dynamic analysis of the Hemoglobin level it was obtained an average level of pre-operative of 10.1 g/dl, respectively 9.39 g/dl post-operative. The average time of the intervention for these patients was of 134 minutes (± 12). By analyzing the data obtained through the histopathological test, approximately 37% of the resection parts were uterine leiomyoma, 27% fibro angioleiomyoma, 18% angioleiomyoma, and 18% adenocarcinoma. This time again we encountered difficulties such as: 2 Clavien-Dindo grade I and 3 Clavien-Dindo grade III b. For the first type of difficulties we distinguished: 1 case of dyspepsia which was decreased by administrating antiemetics and antispasmodics; 1 case of cystitis, case in which the patient benefited of specialized urology consultation and a proper drug management administration until her release of the hospital. Taking into consideration the second type of difficulties, i.e., grade III b, we encountered the following: 2 cases of serous lesions at the ileum level where patients benefited of enterorrhaphy, thread 3-0 monofilament; 1 case of lesion on the inferior pole of the bladder, case which benefited of double-layer cystography.
By analyzing in detail the data obtained individually within each study group, it was emphasized the fact that there is a co-relation between the numbers of the comorbidities and the patients’ age (r=0.767, p˂0.04) and at the same time a positive moderated co-relation between the number of the comorbidities and the BMI (r=0.493, p˂0.05). Somehow self-explanatory, it was emphasized the fact that group B and C which contained mostly patients with the BMI limit over the usual one, it was remarked a proportional increase of the comorbidities at the same time with the increase of the BMI. The data presented in Table 1 shows a strong postive co-relation between the BMI and the intervention time (p=0.047), therfore, those two being tied by proportional increase relation. For those patients with a high BMI, the operatie time was extended due to the presence of excesive visceral fat which impeded the facial dissection and due to the tumoral dimension that manifested at the level of each batch of patients.
| Time of the intervention (minutes) | Blood loss intraoperative (ml) | Time in the hospital (days) | Minor complications | Major complications | Blood transfusion | Average weight of uterus (g) |
|---|---|---|---|---|---|---|
| 106,1 ± 12,2 | 83,61 | 4,25 | 4 | 0 | 1 | 181 |
| 122 ± 19,2 | 112 ± 11,2 | 4,8 | 2 | 1 | 2 | 194 |
| 134 ± 21,3 | 178 ± 23,2 | 5,07 | 2 | 3 | 3 | 194 |
| 0,047 | 0,05 | 0,04 | 0,89 | 0,05 | 0,05 | 194 |
Table 1: Strong postive co-relation between the BMI and the intervention time
It was also observed that concomitant with the BMI increase took place an increase of the uterus’s average weight, through which it was obtained a significant statistic co-relation (p˂0,042). For what concerns the time of the admission and the BMI, we observed a statistically significant and positive co-relation (r=0,280, p˂0,05) which means that for the obese patients the time spent in the hospital was way more extended comparted to those normo-ponderal. If we are to take the age and the dimension of the uterus in longitudinal axis at the general batch level, we obtained a statistically negative co-relation (r=-0.297, p˂0.05) since the uterus dimensions decreased while the age increased. For the obese patients, it was observed that the ovarian cyst associated to the uterine pathology increased at the same time with the increase of the BMI (r=0.827, p˂0.05) and at the same time it was emphasized a strongly positive co-relation between the dimension of the skin fold and BMI (r=0.712, p˂0.05).
With reference to the number of complications, we encountered 12 of them, out of which 8 were minor (Clavien-Dindo grade I), and 4 were major (Clavien-Dindo grade III b). The analysis shown in Table 1 emphasizes the fact that for some minor complications 4 were encountered within normo-ponderal patients, 2 within overweighed patients and 2 within obese patients (p=0.891). For what concerns the major complications, they were encountered mostly to the groups with a high BMI, while through the patients with a low BMI, there was no major complications encountered. In this way we obtained a statistically significant co-relation between BMI and the post-opearive difficulties (p˂0.05); on the other hand, for the obese patients there were higher chances of major complications (Clavien-Dindo˃III) compared to the other patients, all this due to the more laborious disection caused by the presence of the excesive fat tissue.
Discussion
Many classification of Laparoscopic Hysterectomy have been proposed, the most used being the 2003 one by Reich (Safran D, et al., 1993), wich divides the Laparoscopic Hysterectomy procedure into LAVH (Laparoscopically Assisted Vaginal Hysterectomy), LH (Laparoscopic Hysterectomy) and TLH (Total Laparoscopic Hysterectomy), the latter being when the entire operation is performed laparoscopically, with no vaginal component except removal of the uterus. For these reasons, we decided to (1) include in this study only TLH with suture of the vaginal vault by laparoscopic approach, (2) use the Clavien-Dindo morbidity scale, which is a reproducible simple system to grade complications, based on the therapy required to treat them, (3) select from the TLH literature only recent studies published after 2007, and with a sizable number of patients.
Uterine morcellation is sometimes required to perform a hysterectomy via a minimally invasive approach. Morcellation has become controversial recently because of concerns regarding dissemination of occult malignancy. However, laparoscopic hysterectomy results in significantly less morbidity and mortality than open hysterectomy. Potential solutions include a careful preoperative workup and performing morcellation contained within a bag. Winner et al. from Department of Obstetrics and Gynecology, Washington University in St. Louis, St. Louis, Missouri conclude after one study that contained power morcellation at the time of Total Laparoscopic Hysterectomy is associated with a 20-minute increase in operative time when compared with uncontained morcellation (Winner B, et al., 2015). In our clinic we use uncontained morcellation.
New devices and techniques that allow surgeons to offer more women the benefits of a minimally invasive approach should be further investigated and encouraged.
Conclusion
The whole team’s experience improved considerably during this study which focused on the improvement of the operative parameters. Moreover, the THL became a gold standard for the way the uterine/ovarian benign/ malign pathology was regarded whether the studied patients are obese or non-obese. Also, by analyzing the difficulties and the post-operative evolution, minor differences were encountered between the study groups, and it was demonstrated that there is no reason to see a high BMI level as an obstacle in performing TLH.
References
- Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001; 286(10): 1195-1200.
[CrossRef] [Google Scholar] [Pubmed]
- Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The continuing epidemic of obesity in the United States. JAMA. 2000; 284(13): 1650-1651.
[CrossRef] [Google Scholar] [Pubmed]
- Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991-1998. JAMA. 1999; 282(16): 1519-1522.
[CrossRef] [Google Scholar] [Pubmed]
- Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983; 67(5): 968-977.
[CrossRef] [Google Scholar] [Pubmed]
- Lew EA, Garfinkel L. Variations in mortality by weight among 750,000 men and women. J Chronic Dis. 1979; 32(8): 563-576.
[CrossRef] [Google Scholar] [Pubmed]
- Gomel V, Taylor PJ. Indications and contraindications of diagnostic laparoscopy. Diagnostic and operative gynecologic laparoscopy. 1995; 68-70.
[CrossRef] [Google Scholar] [Pubmed]
- National Institutes of Health. Health implications of obesity: National Institutes of Health consensus development conference statement. Ann Intern Med. 1985; 103(6): 1073-1077.
[CrossRef] [Google Scholar] [Pubmed]
- Pi-Sunyer FX. Health implications of obesity. Am J Clin Nutr. 1991; 53(6): 1595-603.
[CrossRef] [Google Scholar] [Pubmed]
- Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson RR, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 1990; 322(13): 882-889.
[CrossRef] [Google Scholar] [Pubmed]
- Pitkin RM. Abdominal hysterectomy in obese women. Surg Gynecol Obstet. 1976; 142(4): 532-536.
[Google Scholar] [Pubmed]
- Safran D, Sgambati S, Orlando III R. Laparoscopy in high-risk cardiac patients. Surg Gynecol Obstet. 1993; 176(6): 548-554.
[Google Scholar] [Pubmed]
- Reich H. Laparoscopic Hysterectomy. Dysmenorrhea. 1992; 613.
- National Heart, Lung, Blood Institute, National Institute of Diabetes, Digestive, Kidney Diseases (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institute of Health. 1998.
[Google Scholar] [Pubmed]
- Koh CH. A new technique and system for simplifying Total Laparoscopic Hysterectomy. J Am Assoc Gynecol Laparosc. 1998; 5(2): 187-192.
[CrossRef] [Google Scholar] [Pubmed]
- Winner B, Porter A, Velloze S, Biest S. Uncontained compared with contained power morcellation in Total Laparoscopic Hysterectomy. Obstet Gynecol. 2015; 126(4): 834-838.
[CrossRef] [Google Scholar] [Pubmed]
Author Info
Ionuț Faur1,2, Laurian Stoica1,2, Alexandru Isaic1,2, Ionel Nati3,4*, Cristi Tarță1,2 and Amadeus Dobrescu1,22Department of Medicinal Sciences, Victor Babes University of Medicine and Pharmacy, Timisoara, Romania
3Department of Obstetric and Gynecology, II nd Obstetric and Gynecology Clinic Dominic Stanca, Cluj-Napoca, Romania
4Department of Medicinal Sciences, Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania
Citation: Faur I: Differences among Obese Versus Nonobese Patients Undergoing Total Laparoscopic Hysterectomy: A Single Surgeon Experience
Received: 07-Feb-2022 Accepted: 21-Feb-2022 Published: 28-Feb-2022, DOI: 10.31858/0975-8453.13.2.69-73
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






