Mini Review - (2023) Volume 14, Issue 11
Abstract
This study delineates the phospholipid flexible carrier systems explored till date primarily for transdermal delivery. Although they are sometimes collectively called as flexible vesicular systems or simple transferosomes. But an articulate understanding of main difference between advanced transferosomes from the conventional one is needed. This paper explains basic difference in various flexible nano carries from transferosomes and the specific terminology used for them. This study is essentially useful for researchers to diligently coin the terms to novel drug delivery systems.
Keywords
Flexible vesicles, Transferosomes, Invasosomes, Ethosomes, Transdermal drug delivery
Introduction
Liposomes came into the picture in the late 1960s, when the time urged the need to develop alternatives drug delivery systems to bring about targetability and reduced unwanted exposure of the drug to the body. Dr. Alec. D. Bangham observed the bilayer character of phospholipids. Later in the early 1970s G. Gregoriad is suggested that these phospholipids can be used as a carrier for drug delivery and it might approximately take 30 years to come to market as a commercial product (V Sharma VK and Agrawal MK, 2021). Liposomes are phospholipid molecules. They are amphiphilic and have a hydrophilic head and a hydrophobic tail. The head is made up of a phosphate group which may further join with other molecules like serine, choline, etc. This phosphate group gives a polar character to the head. Two hydrophobic chains derived from fatty acids are joined to the phosphate group through glycerol molecules. These fatty acid chains give phospholipids a hydrophobic character. Phospholipids derived from soy or egg contains a variety of molecules of different chemistry. When comes in contact with water these phospholipids arrange themselves into bilayer vesicular system, having the capacity to accommodate active drug in it. Depending upon the type of fatty acid chains, their saturation or unsaturation, and polar head group, phospholipids are classified into various types (Table 1). E.g. phosphatidylethanolamine, phosphatidylinositol, phosphatidylcholine, and hydrogenated phosphatidylcholine. The human cell membrane resembles a sandwiched bilayer of phospholipids. Due to the chemical composition of liposomes similar to the cell membrane, liposomes were established as bio-compatible, biodegradable, and biologically safe. Also, they cover the drug inside them thereby protecting the drug from biological degradation. The unilamellar vesicles made from phospholipids produce vesicles of 10-200 nm diameter, hence called nanocarriers, which can easily get transported through the capillaries, whose average diameter is in the micrometre size range.
| Flexible-vesicular systems | ||
|---|---|---|
| Surfactant based | Penetration enhance based (sorption promoters/accelerants | Combination of surfactants and penetration enhancer based |
|
|
|
Table 1: Classification of flexible vesicular systems
Literature Review
The liposomes made up solely of phospholipids are rigid (Touitou E, et al., 2000). During 1990s, they were explored for transdermal delivery of drugs, poor penetration was observed through the skin (Touitou E, et al., 2000) (Zhang J, et al., 2020). It was studied by Cevc G and Blume G, 2001 that to increase the penetrability of liposomes, the surface has to be modified to make it more flexible and stress adaptable (Nayak D and Tippavajhala VK, 2021). Thus they end up synthesizing deformable vesicles with the use of an EDGE Activator (EA). The deformable vesicles have a special character to deform when stress is applied and can again reform to their original structure, without the loss of active drug from it. Thus, they are also termed flexible-liposomes. Over the last 30 years of their discovery, many different strategies have been applied to create more advanced form of flexible vesicles. Certain strategies include the use of permeation enhancers, such as fatty acids, surfactants, alcohols, phospholipids, cyclodextrins, and terpenes.
Deformable vesicles have stress-dependent activity. In human cells, the sterol is present in the phospholipid bilayer of the cell membrane which gives the capacity to deform themselves while in microcirculation. The studies of erythrocytes explain the various reasons and factors which impart fluidity to the cell membrane. The same concept was applied to liposomes to make them more flexible to pass through the stratum corneum. The flexibility is affected by many factors like the ratio of saturation to unsaturation present in the membrane, presence of cholesterol, the temperature in which vesicles are places, fatty acid chain length, etc. Since the discovery of the essence of flexi-liposomes and their applications in topical and transdermal delivery primarily, various strategies have been adopted to form advanced flexi-vesicular systems having different chemical compositions.
Discussion
Transferosomes
These were the first flexible phospholipid carriers, developed by Cevc G and Blume G, 2001 to increase the penetrability of diclofenac through the skin in early 90s. To the conventional liposomes, an EA was added, to impart flexibility to the liposomes. The resultant vesicles are found to deform themselves to get penetrate through the skin and reform once the penetration is done, thus termed as transferosomes. EA are amphiphilic agents, act as surface-active agents by imparting high radius of curvature. This means that, when EA is incorporated in the vesicle containing a phospholipid, the surfactants give the vesicles the capacity to reform to their initial form after the deformation or in other words give high rebound to the vesicular structure when the stress is released. Surfactants are single-chain amphiphilic molecules that distribute themselves in between the lipid bilayer making the layer flexible throughout. Some authors have also termed them as flexible-membrane vesicles (Sharma G, et al., 2017). Commonly used surfactants are sodium cholate, sodium deoxycholate, spans, and tweens. It was found that they can penetrate a pore size 10 times smaller than their diameter. The surfactant molecules arrange themselves in between the phospholipid layer, reducing the rigidity of phospholipid carriers. The vesicles thus form a bilayer wherein the vesicles will orient forming hydrophobic sandwiched between hydrophilic head facing outward and inward carrying a hydrophillic microenvironment. The main driving force that leads to the penetration of transferosome across skin is hydrotaxis. This was explained as a process where the hydrophilic surface of the vesicles helps to move the vesicle to the lower layer of the skin containing a high amount of water as compared to the upper layer, provided the skin is non-occluded (Zhang J, et al., 2020). These vesicles are formed using a 10%-15% w/w surfactant concentration. Transferosomes shows good flexibility and transdermal penetration but the major issue with the use of transferosomes is their self-stability. Transfersomes tend to undergo aggregation and fusion. The leakage of drugs from the vesicles is also reported (Khan I, et al., 2020).
To overcome this problem, modifications to transfersomes were done and protransferosomes were fabricated. These dry formulations are comprised of a thin lipid film (e.g. a mixture of a phospholipid, surfactant, drug and with or without cholesterol) deposited over carbohydrate carrier particles (e.g. sucrose, sorbitol or mannitol) (Khan I, et al., 2020). These formulations contain micro sized flexible vesicles which get converted in situinto transferosomes by absorbing water from the skin. These were said to have better stability, entrapment efficiency, and penetrability. Initial trials include the formulation of norgestrel in protransferosomes (Jain S, et al, 2003). The method of preparation of prothransfersomes involved mixing of phospholipids, surfactants, and drugs in alcohol and then warmed at 60°C-70°C to dissolve all ingredients. An aqueous phase containing 0.1% glycerol was added to the above mixture and warmed to get a clear solution. The solution was then cooled and converted into the gel (Jain S, et al, 2003). Another formulation was reported to be paclitaxel micro-protransfersome powder formulation a novel paclitaxel (PTX) loaded protransfersome tablet formulations for pulmonary drug delivery. The compression of powders into tablet form is appealing, offering several select advantages, including; ease of large scale manufacturing, handling, and packaging (Khan I, et al., 2020).
The beneficial effect of the formulation containing flexible-vesicular system has promoted the research in the category to form more advanced, auxillary modified, and novel flexible vesicles. Edge activators and penetrants were researched explicitly and their use is still emerging. Penetration enhancers may work in one or multiple different ways to promote the flux of the vesicles across the skin. The mode of action of penetrants is broadly categorized as the mechanism that disrupts the packing arrangement of lipid bilayer or by increasing the drug partitioning in the skin by acting as a solvent. Following are various novel vesicles formulated over time to increase the vesicular penetration (Williams AC and Barry BW, 2012).Ethosomes
These are the phospholipid vesicles containing high amount of ethanol in their composition, which act as penetration enhancer and gives elasticity to the vesicles. Sometimes also termed elastic nano-vesicles by some authors. Ethanol is used in 20%-45% in composition for ethosome formation (Touitou E, et al., 2000). Composition includes phospholipids (usually 2%-5% phosphatidylcholine), 20%-45% ethanol and water to 100% (w/w). Ethanol is known to interact with phospholipids of the stratum corneum and enhances lipid fluidity by causing lipid interdigitation effect. The vesicles thus formed have negative charge on them which is imparted by the presence of ethanol and the magnitude of it increases as the number of ethanol increases in the formulation. Ethosomes show better skin penetration both under occlusive and non-occlusive conditions (Chacko IA, et al., 2020) (Table 2). Also high ethanolic content imparts steric stabilization (Chacko IA, et al., 2020) and electrostatic repulsion of vesicles, thus affecting the vesicular size. The final concentration of phospholipid can be from 0.5%-10% of the final ethosome (Mishra KK, et al., 2019). A significant ‘Push effect’ is created by the synergistic use of ethanol, phospholipids, and stratum corneum, when formulated in a vesicular system than the simple hydroalcoholic solution. The penetration of ethosome is expected to be due to various factors like synergistic effect as explained above. Secondly, the ‘ethanol effect’ where ethanol interacts with the polar head of lipid present on phospholipids increases lipid fluidity, thus providing flexible character to the vesicles. Or ethanol directly affects the phospholipids of the stratum corneum (Paiva-Santos AC, et al., 2021).
| Mechanism of permeation/penetration | |
|---|---|
| Flexible nature of vascular membrane |
|
| Denaturation of phospholipid membrane (both vascular and skin cells) |
|
| Combination of flexible membrane and denaturant property |
|
Table 2: Mechanism of action of skin penetration/permeation
Ethosomes are further explored and modified for improvements. Transethosomes is a new term coined by song and coworkers in 2012 to a novel flexible carrier containing both Edge activator and ethanol (up to 30%) in combination (Song CK, et al., 2012). The first formulation was prepared using voriconazole and results claim that better skin penetration occurs as compared to ethosome or transferosome alone. The effect could be due to the synergistic role of ethanol and surfactant to increase skin penetration. Another study compared the transferosomes, ethosomes, and transethosomes of vitamin A and caffeine and concluded that transethosomes are more efficient in skin penetration than individual vesicles (Ascenso A, et al., 2015).
Another auxiliary modified form of ethosomes is binary ethosomes. These uses a combination of ethanol and other alcohols like propylene glycol or isopropyl alcohol (Paiva-Santos AC, et al., 2021). These vesicles are claimed to produce vesicles with smaller size, higher stability, and high permeation capacity than ethosome alone. It is essential to adjust the ratio of alcoholic composition in the formulation to optimize the formulation.
Ethanol and methanol when compared for their individual properties to alter the phospholipids, it was observed that ethanol acts as a better penetrant than methanol. Simulation studies showed that ethanol can pass through bilayer more easily (with time-lapse of less than 200 ns) than methanol (approximately in microseconds). Also, ethanol molecules tend to condense near the lipid water interface causing a sharp increase in their density as compared to methanol. The study was conducted on the DPPC bilayer by Patra M, et al., 2006. Various methods used to prepare ethosomes include cold method, hot method, mechanical dispersion method, transmembrane PH gradient method, etc.
Menthosomes
These were developed in the early 2010s, as an effort to bring about an alternate strategy to produce flexible liposomes with better penetration effect. Menthosomes includes phospholipids, surfactant, and menthol as permeation enhancer (Nayak D and Tippavajhala VK, 2021). Duangjit S, et al., 2012 were the first ones to report the menthosomes of meloxicam. They developed these deformable vesicles with phospholipids, cholesterol, cationic surfactant (cetylpyridinium chloride) and menthol as permeation enhancers. Menthosomes promote the skin permeation of drugs by improving the drug partitioning and diffusion of drugs (Chacko IA, et al., 2020). The comparison was made between mentosomes, transfersomes, and conventional liposomes to check the skin permeation of meloxicam. The menthosomes were claimed to be more efficient to permeate through skin. The cholesterol is believed to impart rigidity to phospholipid backbone by increasing the packing density of phospholipids, cationic surfactant act as edge activator which have a high radius of curvature and impart flexibility to vesicles; menthol alters the lipid microstructure both of skin tissues as well as of vesicles thus help in synergistically enhancing the permeation of the vesicles. The lipidic bilayer of human cells is made up of hexagonal and orthorhombic packing of lipid hydrocarbon chains. Menthol is observed to alter the hexagonal hydrocarbon chain packing. Thus affecting lipid arrangement and hence acting as a permeation enhancer (Duangjit S, et al., 2014).
Invasosomes
Use of natural penetration enhancers was also considered in vesicular system development as natural penetrants are more effective than synthetic penetrants (Figure 1). The natural penetrants offer less toxicity also. The effect of terpenes on bulfalin drug was checked by Chen J, et al., 2016. The same property was applied to formulate flexible vesicular carrier’s invasosomes. Terpenes show up to 8 times more enhancement than synthetic penetrants like oleic acid, lauric acid, SDS, azone, ethyl oleate, and ethyl lauric acid. Invasosomes are meant to deliver the drug deep into the skin or systemic circulation without invasive delivery. The composition includes phospholipids, ethanol (3% v/v), terpene(s) (1%-5%v/v) and water (Chacko IA, et al., 2020) (Nayak D and Tippavajhala VK, 2021). Terpenes consist of a repeated unit of isoprene (C5H8). Terpenes are hydrocarbon compounds and are known to be the primary constituents of essential oils from many plants (Babaie S, et al., 2020). The reported formulation has made size ranging from 100 nm to 13 µm (Apolinario AC, et al., 2021). The ethanol act by creating fluidizing effect by disturbing the lipid structure of the cell membrane. Terpenes act as permeation enhancers and have a role in percutaneous delivery. Penetration of invasomes is carried out in two different ways. The bigger vesicles are thought to disintegrate and release their content and increase the fluidity of the lipid membrane of the cells. The smaller vesicles are believed to remain intact and penetrate through the follicular transport pathway and/or narrow hydrophilic channels (Babaie S, et al., 2020). Limonene, carvone, and nerolidol were used as terpene penetration enhancers in the formulation of finasteride (Prasanthi D and Lakshmi KP, 2013). Others used cineole:citral:d-limonene (45:45:10), v/v in combination for transdermal delivery of temoporfin (Song CK, et al., 2012). While formulating invasosome other factors including skin type, pH values, and formulation ingredients should also be taken into account as the sources of experimental variabilities.
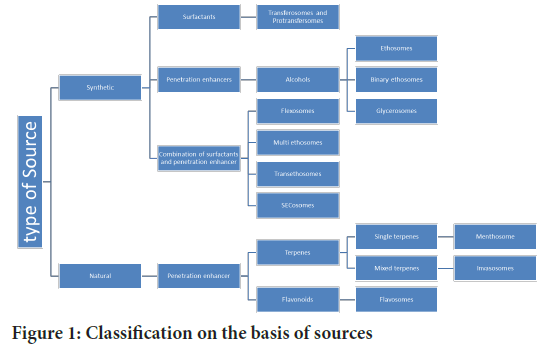
Figure 1: Classification on the basis of sources
Flavosomes
These are other vesicular systems developed by Zhang J, 2020 for meloxicam. Flavosomes are made up of phospholipids, cholesterol, surfactants (e.g cetyl pyridinium chloride), and flavonoids (Apolinário AC, et al., 2021). Generally used flavonoids are quercetin and dihydroquercetin (Zhang ZJ and Michniak-Kohn B, 2020). From the literature review, they concluded that flavonoids tend to deform the packing arrangement of a lipid bilayer. Thus formulated flavosomes increases vesicular deformability as well as the fluidity of the stratum corneum. The flavosomes thus prepared showed better deformability than transferosomes and shorter lag time than transferosomes (Zhang ZJ and Michniak-Kohn B, 2020).
Flexosomes
Some researchers claim flexosome formation using a mixture of phospholipid, ethanol, and tween 80. The formed formulation shows benefits of both the transfersomes and ethosomes (Abdel-Messih HA, et al., 2019) (Alomrani AH and Badran MM, 2017). Another researcher describes flexosomes wherein different combinations of surfactants are used. E.g. (Tweens, Spans, hexadecyl trimethyl ammonium bromide, sodium deoxycholate, etc.). They considered flexosomes as a specific type of transethosomes. Broadly, it can be stated that flexosomes may contain up to 2 surfactants and/or 2 penetration enhancers. This effort will synergistically affect the flexibility of the vesicles (Duangjit S, et al., 2012).
Multi-ethosomes
These vesicles claimed to have benefits of both binary ethosomes and transferosomes. They are composed of phospholipids, ethanol, Propylene glycol, edge activator (Tween 80), and specific penetration enhancer (Zhang L, et al., 2020). These show better colloidal stability and no drug leakage after 2 months.
Glycerosomes
The first attempt was made in 2013 using phospholipids, glycerol (10%- 30%), and water to form flexible vesicles of diclofenac sodium. The phospholipids were hydrated with glycerol aqueous solution and found effective than conventional liposomes, which are used as control (Manca ML, et al., 2013). These are prepared by thin-film hydration method, solvent spherule method, sonication method, and French pressure cell method (Gupta P, et al., 2020) Zhang K, et al., 2017 used essential oil as a penetration enhancer in combination with glycerols for topical administration of paeoniflorin. The formulation was composed of phospholipids, glycerol, cholesterol, and Speranskia tuberculate essential oil.
A better biodistribution of rifampicin was studied with hybrid glycerosomes. Trimethyl chitosan chloride-glycerosomes and sodium hyaluronate-glycerosomes were formulated and compared to check formulation effectiveness (Melis V, et al., 2016).
SECosomes
An ultraflexible siRNA-containing nanosome, prepared using phospholipids, cholesterol, sodium cholate, and 30% ethanol. They termed them as surfactant-ethanol-cholesterol nanosomes (Geusens B, et al., 2010).
General consideration for penetration enhancer
Physicochemical properties of penetration enhancers widely affect the degree of penetration enhancement for different drugs. For e.g partition coefficients, molecular weights, and solubilities of penetration enhancers affect their role in enhancement. Penetration enhancers used in combination with alcohols act synergistically such as azone, oleic acid (and other fatty acids), and terpenes with Propylene glycol. The penetrants have a concentration-dependent effect on the degree of enhancement (Williams AC and Barry BW, 2012).
Conclusion
Vesicular transdermal delivery is the most widely researched area when comes to non-invasive drug delivery system. Phospholipids are the backbone of this system. Along with the phospholipids other surfactants or penetrants are used as additives to make them flexible so that they can undergo better percutaneous or transdermal delivery. These surfactants and penetrants are also used in combination to synergistically improve the penetration. Apart from the transdermal drug delivery, these vesicles are also being explored for mucosal drug transfer and tissue targetability. The compositions and effect of various additives on entrapment efficiency and penetrability depend upon many factors. An issue still exists with the use of the terminology of such carriers. Use of terms like flexi-liposomes, elastic vesicles, deformable vesicles, and deformable liposomes is still primarily used while mentioning transferosomes only. This creates perplexity, as other vesicles are also flexible and able to penetrate the skin. So it is required to be more considerate while choosing the terminology for a novel vesicular system. A detailed analysis of formulation factors is also expected to be researched to provide new insights to understand better formulation strategies for flexible vesicular systems.
References
- Sharma VK, Agrawal MK. A historical perspective of liposomes-a bio nanomaterial. Mater Today. 2021; 45: 2963-2966.
- Touitou E, Dayan N, Bergelson L, Godin B, Eliaz M. Ethosomes-novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J Control Release. 2000; 65(3): 403-418.
[Crossref] [Google Scholar] [Pubmed]
- Zhang J, Froelich A, Michniak-Kohn B. Topical delivery of meloxicam using liposome and microemulsion formulation approaches. Pharmaceutics. 2020; 12(3): 282.
[Crossref] [Google Scholar] [Pubmed]
- Cevc G, Blume G. New, highly efficient formulation of diclofenac for the topical, transdermal administration in ultradeformable drug carriers, transfersomes. Biochim Biophys Acta. 2001; 1514(2): 191-205.
[Crossref] [Google Scholar] [Pubmed]
- Nayak D, Tippavajhala VK. A comprehensive review on preparation, evaluation and applications of deformable liposomes. Iran J Pharm Res. 2021; 20(1): 186.
[Crossref] [Google Scholar] [Pubmed]
- Sharma G, Thakur K, Setia A, Amarji B, Singh MP, Raza K, et al. Fabrication of acyclovir-loaded Flexible Membrane Vesicles (FMVs): Evidence of preclinical efficacy of antiviral activity in murine model of cutaneous HSV-1 infection. Drug Deliv Transl Res. 2017; 7(5): 683-694.
[Crossref] [Google Scholar] [Pubmed]
- Khan I, Apostolou M, Bnyan R, Houacine C, Elhissi A, Yousaf SS. Paclitaxel-loaded micro or nano transfersome formulation into novel tablets for pulmonary drug delivery via nebulization. Int J Pharm. 2020; 575: 118919.
[Crossref] [Google Scholar] [Pubmed]
- Jain S, Sapre R, Umamaheswari RB, Jain NK. Protransfersomes for effective transdermal delivery of norgestrel preparation and in vitro characterization. Indian J Pharm Sci. 2003; 65(2): 152-160.
- Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev. 2012; 64: 128-137.
[Crossref] [Google Scholar] [Pubmed]
- Chacko IA, Ghate VM, Dsouza L, Lewis SA. Lipid vesicles: A versatile drug delivery platform for dermal and transdermal applications. Colloids Surf B Biointerfaces. 2020; 195: 111262.
[Crossref] [Google Scholar] [Pubmed]
- Mishra KK, Kaur CD, Verma S, Sahu AK, Dash DK, Kashyap P, et al. Transethosomes and nanoethosomes: Recent approach on transdermal drug delivery system. Nanomedicine. 2019.
- Paiva-Santos AC, Silva AL, Guerra C, Peixoto D, Pereira-Silva M, Zeinali M, et al. Ethosomes as nanocarriers for the development of skin delivery formulations. Pharm Res. 2021; 38(6): 947-970.
[Crossref] [Google Scholar] [Pubmed]
- Song CK, Balakrishnan P, Shim CK, Chung SJ, Chong S, Kim DD. A novel vesicular carrier, transethosome, for enhanced skin delivery of voriconazole: Characterization and in vitro/in vivo evaluation. Colloids Surf B Biointerfaces. 2012; 92: 299-304.
[Crossref] [Google Scholar] [Pubmed]
- Ascenso A, Raposo S, Batista C, Cardoso P, Mendes T, Praça FG, et al. Development, characterization, and skin delivery studies of related ultradeformable vesicles: Transfersomes, ethosomes, and transethosomes. Int J Nanomedicine. 2015;10: 5837-5851.
[Crossref] [Google Scholar] [Pubmed]
- Patra M, Salonen E, Terama E, Vattulainen I, Faller R, Lee BW, et al. Under the influence of alcohol: The effect of ethanol and methanol on lipid bilayers. Biophys J. 2006; 90(4): 1121-1135.
[Crossref] [Google Scholar] [Pubmed]
- Nayak D, Tippavajhala VK. A comprehensive review on preparation, evaluation and applications of deformable liposomes. Iran J Pharm Res. 2021; 20(1): 186.
[Crossref] [Google Scholar] [Pubmed]
- Duangjit S, Obata Y, Sano H, Kikuchi S, Onuki Y, Opanasopit P, et al. Menthosomes, novel ultradeformable vesicles for transdermal drug delivery: Optimization and characterization. Biol Pharm Bull. 2012; 35(10): 1720-1728.
[Crossref] [Google Scholar] [Pubmed]
- Duangjit S, Obata Y, Sano H, Onuki Y, Opanasopit P, Ngawhirunpat T, et al. Comparative study of novel ultradeformable liposomes: Menthosomes, transfersomes and liposomes for enhancing skin permeation of meloxicam. Biol Pharm Bull. 2014; 37(2): 239-247.
[Crossref] [Google Scholar] [Pubmed]
- Chen J, Jiang QD, Chai YP, Zhang H, Peng P, Yang XX. Natural terpenes as penetration enhancers for transdermal drug delivery. Molecules. 2016; 21(12): 1709.
[Crossref] [Google Scholar] [Pubmed]
- Babaie S, Del Bakhshayesh AR, Ha JW, Hamishehkar H, Kim KH. Invasome: A novel nanocarrier for transdermal drug delivery. Nanomaterials. 2020; 10(2): 341.
[Crossref] [Google Scholar] [Pubmed]
- Apolinario AC, Hauschke L, Nunes JR, Lopes LB. Lipid nanovesicles for biomedical applications:‘What is in a name’? Prog Lipid Res. 2021; 82: 101096
[Crossref] [Google Scholar] [Pubmed]
- Prasanthi D, Lakshmi KP. Iontophoretic transdermal delivery of finasteride in vesicular invasomal carriers. Pharm Nanotechnol. 2013; 1(2): 136-150.
- Zhang ZJ, Michniak-Kohn B. Flavosomes, novel deformable liposomes for the co-delivery of anti-inflammatory compounds to skin. Int J Pharm. 2020; 585: 119500.
[Crossref] [Google Scholar] [Pubmed]
- Abdel-Messih HA, Ishak RA, Geneidi AS, Mansour S. Tailoring novel soft nano-vesicles ‘Flexosomes’ for enhanced transdermal drug delivery: Optimization, characterization and comprehensive ex vivo-in vivo evaluation. Int J Pharm. 2019; 560: 101-115.
[Crossref] [Google Scholar] [Pubmed]
- Alomrani AH, Badran MM. Flexosomes for transdermal delivery of meloxicam: Characterization and anti-inflammatory activity. Artif Cells Nanomed Biotechnol. 2017; 45(2): 305-312.
[Crossref] [Google Scholar] [Pubmed]
- Zhang L, Li X, Zhu S, Zhang T, Maimaiti A, Ding M, et al. Dermal targeting delivery of terbinafine hydrochloride using novel multi-ethosomes: A new approach to fungal infection treatment. Coatings. 2020; 10(4): 304.
- Manca ML, Zaru M, Manconi M, Lai F, Valenti D, Sinico C, et al. Glycerosomes: A new tool for effective dermal and transdermal drug delivery. Int J Pharm. 2013; 455(1-2): 66-74.
[Crossref] [Google Scholar] [Pubmed]
- Gupta P, Mazumder R, Padhi S. Glycerosomes: Advanced liposomal drug delivery system. Indian J Pharm Sci. 2020; 82(3): 385-397.
- Zhang K, Zhang Y, Li Z, Li N, Feng N. Essential oil-mediated glycerosomes increase transdermal paeoniflorin delivery: Optimization, characterization, and evaluation in vitro and in vivo. Int J Nanomedicine. 2017; 12: 3521-3532.
[Crossref] [Google Scholar] [Pubmed]
- Melis V, Manca ML, Bullita E, Tamburini E, Castangia I, Cardia MC, et al. Inhalable polymer-glycerosomes as safe and effective carriers for rifampicin delivery to the lungs. Colloids Surf B Biointerfaces. 2016; 143: 301-308.
[Crossref] [Google Scholar] [Pubmed]
- Geusens B, Van Gele M, Braat S, De Smedt SC, Stuart MC, Prow TW, et al. Flexible nanosomes (SECosomes) enable efficient siRNA delivery in cultured primary skin cells and in the viable epidermis of ex vivo human skin. Adv Funct Mater. 2010; 20(23): 4077-4090.
Author Info
Palwinder Kaur*Citation: Kaur P: Flexible Vesicular Systems: A Mini Review on the Explored Areas for Transdermal Delivery
Received: 13-Oct-2023 Accepted: 27-Oct-2023 Published: 03-Nov-2023, DOI: 10.31858/0975-8453.14.11.701-705
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






