Review Article - (2023) Volume 14, Issue 2
Abstract
Food intolerance, often known-as Food Allergy (FA), is an abnormal immunological response to a food protein or component. The severity of a Food Allergy reaction varies. Immune responses can be mediated by IgE, non-IgE, or both in some situations. The gut considers dietary proteins to be foreign antigens, and those who are allergic to them have an immunological reaction to them. The body triggers an allergic reaction when IgE binds to the dietary allergen. Vomiting, itching, rashes, breathing difficulties, and other symptoms of an allergic reaction vary from mild to severe. If the allergic symptoms are detected, then it’s critical to eliminate the allergen-containing foods from your diet. In the event of accidental exposure, epinephrine should be given intramuscularly. Cow’s milk, peanuts, eggs, shellfish, and fish are all common foods that cause allergic responses. Immunotherapy, anti-IgE therapy, probiotics, and gene therapy are some of the additional treatment options.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Keywords
Food Allergy (FA), Hypersensitivity, Anaphylaxis, Epinephrine
Introduction
The immune system’s reaction to food is known as a Food Allergy (FA). The gut considers dietary proteins to be foreign antigens, and those who are allergic to them have an immunological reaction to them. Because FA is a dysregulation of immunological tolerance mechanisms, the tolerance is the suppression of this reaction (Valenta R, et al., 2015). Food allergies are becoming more common among people, impacting roughly 10% of the population and causing substantial problems for patients, such as dietary limitations, fear of inadvertent ingestion, and the potential of severe reactions, all of which reduce quality of life. Food allergies are a negative health consequence that develops as an immunological response in response to a trigger (Savage J, et al., 2016). Vomiting, itching, loose bowels, rashes, difficulty breathing, low blood pressure, swelling of the tongue, and other signs and symptoms of allergy varies from mild to severe. After coming into contact with the allergen for a few minutes to several hours, the reaction begins. Anaphylaxis develops as symptoms intensify. FA is sometimes confused with food poisoning or food intolerance, although the two are not the same and are not caused by an immunological response.
Cow’s milk, peanuts, eggs, shellfish, and fish are all common foods causing allergic responses (Sicherer SH and Sampson HA, 2014). Food allergies are more common in young children; for example, 50%-60% of children overcome milk and egg allergies, whereas 22 percent of children outgrow peanut allergies and 9-14 percent of children outgrow tree-nut allergies by the age of two to six years (Rad AH, et al., 2021). The body triggers an allergic reaction when IgE binds to the dietary allergen. Because there is no definite treatment for allergic reactions, effective care for IgE-mediated allergic reactions relies solely on rigorous avoidance of allergens, awareness of the allergy, and the reduction of symptoms. It is critical to recognize an allergy early on and learn how to manage it. IgE production against food allergens is the most common immune-mediated abnormal reaction to food allergens, which is followed by inflammation generated and mediated by eosinophil’s and T cells (Martino D, et al., 2014). When allergen-specific IgE antibodies interact with the high affinity receptor (FcRI-expressed on basophils and mast cells) and low affinity receptor (FcRII-present on monocytes, platelets, macrophages, and lymphocytes), acute allergic symptoms develop. The binding of IgE to FcRI causes receptor cross-linking and the release of mediators to begin. Basophils, like mast cells (primary effector cells in acute IgE-mediated reactions), play a crucial role in the initial immunological response, according to studies. Inflammatory mediators such as histamine and leukotrienes, inflammatory cytokines (IL-4 and IL-13), proteases (tryptase), and other chemotactic molecules are released as a result (Stone KD, et al., 2010). IgE epitope on allergen, higher levels, and strong affinity of allergen specific IgE all raise the strength of the acute allergic reaction. In addition, IL-4 stimulates the formation of mast cells in the intestine. The late phase of the immune response includes steroid-sensitive eosinophil and basophil reflux, as well as Granulocyte Macrophage Colony Stimulating Factor (GM-CSF). Eosinophilic esophagitis is also triggered by basophil reactions. Enteric eosinophils have been found to play a function in inflammation and to exert control over dendritic cells in the start of primary Th2 cell-mediated immune responses. After 24-48 hours of allergen interaction, late phase immune responses occur, which mimic a type 4 hypersensitivity reaction including allergenic specific T cells activated by IgE independent and IgE dependent pathways (Martino D, et al., 2014). Patients with food hypersensitivity have a high rate of histamine release from tryptase-negative cells, such as basophils. The common and important food allergens all have the same size, 10-70 kD, are water soluble glycoproteins, and are resistant to proteases, heat, and acid. The impaired epithelium barrier of the body, the allergen, and some non-allergenic dietary components are the main causes of allergy sensitization. Extrinsic factors such as anti-inflammatory medicines, alcohol, or stress, as well as intrinsic variables such as mutations and inheritance, impair the barrier function of the epithelium of the intestine, causing the body to become sensitive for the food protein (Savage J, et al., 2016).
Food Allergy can be classified widely into 3 types:
• IgE-mediated allergy reactions occur when IgE antibodies are activated in response to interaction with an allergen. Food allergies caused by IgE have virtually immediate consequences after ingesting the allergen-containing food. The most typical symptoms in this scenario are reddening of the skin, vomiting, hives, and anaphylaxis in extreme cases.
• Non-IgE mediated-the gastrointestinal tract is predominantly affected rather than the cutaneous systems or respiratory. Immune reactions to food occur in the absence of food-specific IgE antibodies in this case. These are delayed responses, and the onset of an allergic reaction might take up to 48 hours. Diarrhea, vomiting, bloating, and other symptoms are typical (Valenta R, et al., 2015).
• Food allergies that affect both IgE and non-IgE pathways are known as mixed food allergies. Milk allergy is a common cause of an allergic response. After 6-48 hours after ingestion, it manifests due to IgE-independent mechanisms and the action of Th2 cells (Sidbury R, et al., 2014). Eosinophilic esophagitis is the most prevalent symptom in this situation.
Following a diagnosis of FA, it is critical to exclude allergen-containing foods from the diet. To treat an allergic reaction caused by an accidental exposure, epinephrine should be injected intramuscularly into the lateral thigh. Food avoidance, as well as detecting and managing allergy and anaphylactic reactions, should be taught to patients and their families. Depending on the intensity of the allergic reaction, therapies such as immunotherapy, gene therapy, and anti-IgE therapies can be used to treat it (Gernez Y and Nowak-Węgrzyn A, 2017). Table 1 shows the organs impacted, as well as the symptoms and immunopathology associated with IgE-mediated Food Allergy.
| S. No. | Organ | Symptoms | Immunopathology |
|---|---|---|---|
| 1 | Skin | Angioedema, urticaria, pruritus, Oral Allergy Syndrome (OAS), flush | IgE mediated degranulation of mast cell or basophil |
| Atopic or Protein contact dermatitis | Facilitated by T cell (with or without involvement of IgE) | ||
| 2 | Respiratory | Edema in larynx or pharynx, cough, hoarseness of voice | IgE mediated degranulation of mast cell or basophil |
| Bronchial asthma, Rhino conjunctivitis | Mediated by T cell | ||
| 3 | Gastrointestinal tract | Anorexia, colitis, vomiting, diarrhea, pain in abdomen, gastroenteritis | Degranulation of mast cell or basophil mediated by IgE |
| Gastroenteritis | Mediated by T cell | ||
| Eosinophilic esophagitis and gastroenteritis | Activation of eosinophil by cytokines | ||
| 4 | Cardiovascular system | Low Blood Pressure (BP), tachycardia, cardiac dysrhythmia, vascular collapse, anaphylaxis | IgE mediated degranulation of mast cell or basophil |
| 5 | Nervous system | Confusion, loss of consciousness, anxiety, irritability | IgE facilitated degranulation of mast cell or basophil; also, T cell facilitated (with or without IgE) |
Table 1: Food allergies mediated by IgE and their mechanism of action on the organs
Literature Review
Food Allergy (FA)
In simple terms, food allergies, also known as food intolerance, are an abnormal immunological reaction to a food protein or food component. The severity of a Food Allergy reaction varies. Immune responses can be mediated by IgE (immediate response), non-IgE (delayed response), or both (in some situations) (Osborne NJ, et al., 2011). Food allergies put a strain on affected people and their families due to dietary and social restrictions, anxiety due to the likelihood of severe reactions, and fear of an accidental reaction and death, all of which diminish quality of life. Despite the seriousness of the health problems caused by food allergies, particularly in children, no single treatment has been discovered to be effective. FA has been identified as a serious public health concern that has a considerable influence on life of both patients as well as their families by the National Academies of Sciences, Engineering, and Medicine (NASEM) (Bute JJ, et al., 2021). Some food allergies can be addressed early in infancy, while others, such as fish, peanut, and shellfish allergies, are lifetime. Because there is no definitive treatment for allergic reactions, effective therapy of IgE-mediated allergic reactions relies solely on rigorous avoidance of allergens, awareness of the allergy, and symptom reduction (Sicherer SH and Sampson HA, 2014). It is critical to recognize an allergy early on and learn how to manage it. Food allergies affect 6-8 percent of children, according to the Centers for Disease Control and Prevention. The person may acquire an allergy to the food he has been eating for years without experiencing any adverse effects. When the body reacts to food poisoning, the immunological response is mislabeled as a Food Allergy in certain cases. Food allergies are caused by a variety of circumstances, including maternal tobacco use, blood IgE levels, maternal ingestion of highly allergic foods, and hereditary factors (Skypala I and Venter C, 2009). The prevalence of rhinitis, asthma, and eczema has increased as people’s immune systems have become more compromised.
IgE production against food allergens is the most common immune-mediated aberrant reaction to food allergens, which is followed by inflammation generated and mediated by eosinophils and T cells. Certain proteins in food, such as amylase trypsin inhibitors found in wheat and a few oligosaccharides found in milk, trigger inflammation in the intestine by activating TLR-4 (Tall Like Receptor-4). Some recent researchers have discovered that CD4+ T cells in children with food allergies differ from those in children who do not have a Food Allergy (Martino D, et al., 2014). There are several hypotheses that claim that family size reduction as well as spontaneous improvement in personal hygiene has a role in the development of IgE-mediated allergies. Along with that an anthroposophical lifestyle, which includes eating of organic food grown without the use of antibiotics, has been shown to reduce allergy cases. The term allergic sensitization refers to the body’s initial immunological response to an allergen. Allergic sensitizations can occur in two ways: One is class I-food allergens, which are oral allergens that produce gastrointestinal sensitivity. The other is class II food allergens, often known as aeroallergens, such as pollen, which cause immune system sensitivity through the respiratory tract. The impaired epithelium barrier of the body, the allergen, and some non-allergenic dietary components are the main causes of allergy sensitization. Extrinsic factors such as anti-inflammatory medicines, alcohol, or stress, as well as intrinsic variables such as mutations and inheritance, impair the barrier function of the epithelium of the intestine, causing the body to become sensitive to food protein (Oyoshi MK, et al., 2014).
When a person is exposed to a food allergen, their immune system is activated, and the allergen is processed by APCs and allergen-specific Th2 cells, triggering the production of IgE antibodies (Vercelli D and Geha RS, 1992). The switching of pathways is induced by the cytokines and allergen-specific IgE production. IgE and T cell memory occur when primary sensitization occurs and a class switch is performed for IgE production. When the body experiences for the second time, the secondary immune reaction is triggered. In the intestine, there are various cellular processes that regulate primary allergy sensitization and tolerance. When antigen is delivered by APC and interacts with C-type lectin receptors, the body can become tolerant. The body does not require T cells in the case of class II food allergens that impact the respiratory tract (Paul WE and Zhu J, 2010). A number of preventative and therapeutic treatments for allergies are now being developed, including processes of allergic sensitization, progression of the disease, and establishing resistance to allergens, in addition to many approaches aimed at enhancing therapeutic efficacy and diagnostic accuracy (Pfaar O, et al., 2019).
Pathogenesis
Food allergies start a sequence of immune responses in the body against the allergen, which can be IgE mediated, mixed IgE (call mediated), or non-IgE mediated. When food allergens come into contact with the body, a Food Allergy develops. As the allergen enters the bloodstream via the gastrointestinal tract, symptoms appear at the site where the allergen comes into contact with the body, such as the esophagus, mouth, or intestine. Even the circulatory and nervous systems are compromised in severe cases (Asarnoj A, et al., 2012). When allergen-specific IgE antibodies interact with the high affinity receptor (FcRI-expressed on basophils and mast cells) and low affinity receptor (FcRII-present on monocytes, platelets, macrophages, and lymphocytes), acute allergic symptoms develop. The binding of IgE to FcRI causes receptor cross-linking and the release of mediators to begin. Basophils, like mast cells (primary effector cells in acute IgE-mediated reactions), play a crucial role in the initial immunological response, according to studies. Inflammatory mediators such as histamine and leukotrienes, inflammatory cytokines (IL-4 and IL-13), proteases (tryptase), and other chemotactic molecules were released (Stone KD, et al., 2010). Patients with food hypersensitivity have a high rate of histamine release from tryptase-negative cells, such as basophils. The common and important food allergens all have the same size, 10-70 kD, are water soluble glycoproteins, and are resistant to proteases, heat, and acid. Some immune stimulatory substances, such as Ara h 1, a glycoprotein allergen from peanuts that is heat stable and resistant to digestion by digestive enzymes, and also works as a Th2 adjuvant, may also play a role in sensitization (Asarnoj A, et al., 2012).
IgE epitope on allergen, higher levels, and strong affinity of allergen specific IgE all raise the strength of the immediate allergic reaction. In addition, IL-4 stimulates the formation of mast cells in the intestine. The late phase of the immune response includes steroid-sensitive eosinophil and basophil reflux, as well as Granulocyte Macrophage Colony Stimulating Factor (GM-CSF). Eosinophilic esophagitis is also triggered by basophil reactions caused by thymic stromal lymphopoietin (Stone KD, et al., 2010). Enteric eosinophils have been found to play a function in inflammation and to exert control over dendritic cells in the start of primary Th2 cell-mediated immune responses. After 24-48 hours of allergen interaction, late phase immune responses occur, which mimic a type 4 hypersensitivity reaction including allergenic specific T cells activated by IgE independent and IgE dependent pathways (Groschwitz KR and Hogan SP, 2009). APCs in allergy patients express a low affinity CD23 receptor that is employed for allergen presentation, which is aided by IgE. Th2 cells (IL-4, IL-5, and IL- 13) and Th1 cells, which release interferon gamma and cause epithelium damage, cause the symptoms of atopic dermatitis.
Mechanism of action
Oral Allergy Syndrome (OAS) is produced by the immune system’s hypersensitization to respiratory allergens with similar structures to food allergens, which might result in a cross-reactive immunological response. The most frequent form of OAS is caused by a large birch tree bet v 1 allergen, but it also causes a cross-reactive immune response with allergens found in plant-based foods such as carrots, apples, celery, and almonds, resulting in acute allergic reactions. Because these dietary allergens are processed by the gastrointestinal tract, allergy symptoms appear only when a considerable amount is consumed, and anaphylactic shock does not develop in his situation (Ivković-Jureković I, 2015). Oral tolerance is determined by the ability of the gastrointestinal barrier to become immunologically active. This barrier is made up of epithelial cells connected by a thick mucus layer and tight junctions, as well as bile salts, luminal border enzymes, and high pH, all of which reduce the immunogenicity of antigens. In addition, innate (polymorphonuclear leukocytes, Natural Killer Cells (NKCs), epithelial cells, Tall Like Receptors (TLRs), and macrophages) and adaptive immunity (IgA, cytokines, intra-epithelial and laminar lymphocytes, and Peyer’s patches) both protect the body from foreign antigens and allergens and provide an active barrier (Commins SP, et al., 2016).
In favor of sensitization, when the active immunological barrier dysregulates then the oral tolerance may be breached. Dysregulation may occur as a result of various environmental influences such as reduced exposure to viruses and germs, excessive omega 6 consumption, low dietary antioxidants, vitamin D shortage or increase, and poor omega 3 Poly Unsaturated Fatty Acid intake (PUFA). Furthermore, Th2 dysregulation may arise as a result of a disruption in the balance of the controlled connection between APCs, regulatory T cells, and epithelial cells, which determine the type of T cell response elicited by a food allergen (Mojtabavi N, et al., 2022). CD4+, CD25+ cells (which secrete beta-Transforming Growth Factor (TGF)), Th3 cells, TR1 cells, cells that secrete IL-10, gamma delta T cells, and CD8+ suppressor cells are regulatory T cells that play a significant part in oral tolerance (Food Reactions, 2005). Because sensitization occurs through the respiratory route in OAS, oral tolerance is bypassed, and unlike allergens found in food (e.g., birch pollen protein), which is tolerated because digestive enzymes destabilize it, pollen allergens generate very significant Th2 inflammation and allergic sensitization. These regulatory T cells function on specific organs, explaining why food allergic disorders are localized rather than systemic, as in the case of eosinophilic esophagitis or atopic dermatitis (Bégin P, et al., 2011).
In non-IgE mediated Food Allergy responses, food immunological reactions occur independently of food specific IgE antibodies. Antibodies that develop as a result of gastrointestinal inflammation are less well understood. TNF alpha is a key player in patients with food-induced enterocolitis (Nowak-Węgrzyn A, et al., 2015). An alternative mechanism for Food Allergy is the mixed reaction, which contains both IgE-dependent and IgE-independent pathways. Milk allergy is a common cause of an allergic response. After 6-48 hours after ingestion, it manifests due to IgE-independent mechanisms and the action of Th2 cells (Sicherer SH and Sampson HA, 2014). When possible, food allergens are taken up by the small intestine have GALT (Gut Associated Lymphoid Tissue), the active process of immunological tolerance begins (Pabst O and Mowat AM, 2012). Immune tolerance is maintained by several types of cells conveying antigen from the gut lumen enter towards the lamina propria, then passing allergen to lymphoid tissue, which shows the antigen and activates T cell response, and finally returning immune receptor cells to the gut (Spergel JM, 2006). Dendrites are disseminated across intestinal epithelial cells, and allergens in the gut are transmitted to dendritic cells by macrophages. T regulatory cells proliferate as a result of the secretion of IL-10 by macrophages.
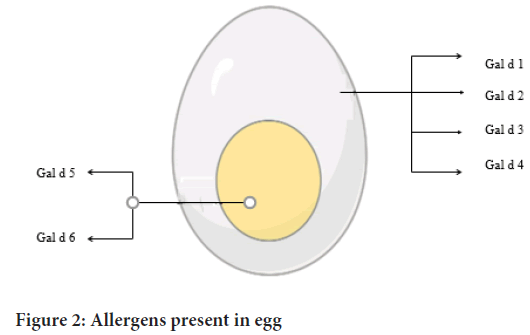
When active food allergens passes through or between epithelial cells in a transcytosis or paracytosis way, it is caught from the gut lumen. M (micro fold) cells and myeloid cells then take up the trapped food allergen. Approximately 2% of total dietary proteins pass totally intact through the intestinal epithelium via transcytosis and are then transferred to secondary lymphoid tissues or the liver for presentation (Rescigno M, et al., 2001). Inflammatory stimuli automate the tolerance to food allergens mediated by dendritic cells, triggering the allergic response mediated by Th2 cells and other cell types (Figure 1).
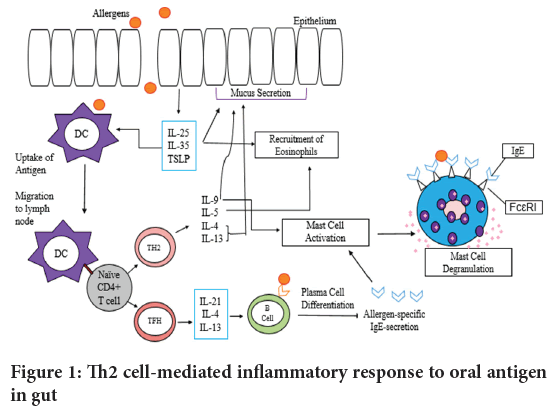
Figure 1: Th2 cell-mediated inflammatory response to oral antigen in gu
When dietary antigens are exposed to the skin, inflammatory cytokines (IL-33, IL-25, and TSLP-thymic stromal lymphopoietin) are generated by epithelial cells in the skin, which act on dendritic cells and shift the immune response to a Th2 cell-related immune response rather than a tolerogenic response (Paul WE and Zhu J, 2010). Additionally, during oral immunotherapy, allergen specific IgE levels decrease while protein IgG4 levels increase (Sugimoto M, et al., 2016).
Diagnosis of food allergies
The history and family history of allergic patients with hypersensitive immune systems are the first things clinicians look for. Since, the increase in the IgE mediated food allergies is found to occur largely within the single generation. It’s unlikely to identify any changes in the human genome, despite of the fact that genetics play a role in the occurrence of Food Allergy (Peters RL, et al., 2022). Because these immune reactions occur relatively soon after food consumption and target important organs, having a history would be beneficial in recognizing antigenic allergens and preparing the body for possible allergic reactions. As a result, understanding the individual’s history will help them prepare for any allergy reactions that may arise. As we all know, acute hypersensitivity immunological reactions happen in a matter of minutes. On the other hand, T cell mediated and mixed allergic reactions have a delayed beginning and therefore individuals with FPIES (Food Protein Induced Enterocolitis Syndrome) begin to experience symptoms after one and a half hours of ingestion. Clinical history can also be used to evaluate the duration of the first and final allergic episodes to determine whether hypersensitivity is decreasing or rising. All of these variables, combined with the assessment of the quantity that causes the allergic reaction, aid in the planning of the diagnostic procedure (Spergel JM, et al., 2004). The self-mediated transport of antigen to secondary lymphoid tissue aids in the establishment of tolerance. The following are some of the approaches for identifying food allergies:
•Clinical History Examination: This is the initial step in diagnosing food allergies, and it offers information on the immunogenic mechanism as well as a clinical representation of allergic reactions to food that vary among ranges. While obtaining a medical history, several critical elements must be considered, including potential allergy triggers, the type of immunological reaction, the presence of co-factors, the time interval between food intake, and the onset of symptoms. Food allergies have no defined pathognomonic symptoms, but the immune system’s quick reactions guide the diagnosis. The clinical history evaluation lacks specificity and sensitivity (NIH, 2018).
•Skin Prick Test (SPT): This is an excellent and quick method of determining Food Allergy sensitivity using fresh food or food extracts. These tests are not only repeatable, but they are also relatively inexpensive. It is safe to use on people of all ages because it causes little discomfort and provides results in 15 minutes. SPT has a high degree of accuracy, and a negative result rule out an IgE-mediated reaction (Randhawa S and Bahna SL, 2009).
•Atopy patch test: This test involves putting food extracts to the skin for 48 hours and is used to determine probable triggers for people with eosinophilic esophagitis.
•In vitro testing: In severe atopic dermatitis, an in vitro examination is performed. Radioallergosorbent Tests (RASTs) and Florescence Enzyme Immunoassay (FEIA) assays can be used to detect food-specific IgE antibodies in the blood. The use of serum IgE testing methods aids in the identification of dietary allergens. Furthermore, these tests should be performed after a thorough assessment of the patient’s medical history, as these tests may produce false positive results, resulting in unnecessary food elimination and, ultimately, nutritional deficiency. In vitro testing should therefore be chosen based on medical history. Higher serum-IgE levels indicate immunological responsiveness; however, these levels might vary depending on a variety of circumstances (such as the time the food was consumed, age, and population) (Pols DH, et al., 2015).
•Basophil activation testing: Being the part of an ex vivo functional assays, basophil activation testing is identified as an effective biomarker of reactivity and tolerance for the diagnosis and treatment of Food Allergy. However, its use is still limited worldwide (Keswani T and Patil SU, 2021).
In vitro and in vivo testing is only useful for detecting sensitization, not for diagnosing clinical allergies. They can’t help with prognosis or severity of reactions, thus it’s crucial to combine the data with the patient’s clinical history.
Treatment of food allergies
The basic strategy for treating food allergies is to completely avoid foods that have been identified as allergens. Allergens tend to enter the body through the consumption of allergen-containing foods, contact with allergens existing on surfaces harboring them, and then touching one’s eyes or nose. Touching or breathing food containing allergens should be avoided by persons with high sensitivity. Due to the potential of anaphylaxis, patients with allergies should be educated to use auto-injectable epinephrine and must have antihistamines or epinephrine with them (Deschildre A and Lejeune S, 2018). Immunotherapy, anti-IgE therapy, probiotics, postbiotics, gene therapy, and other treatments are available. Postbiotics with unique properties such as a safe profile, longer shelf life, resistance to mammalian enzymes, and stability in a variety of digestive system conditions, have a safe suppression against their parent live cells, and also improve immune tolerance and treat FA without causing any side effects or infections, especially in infants (Rad AH, et al., 2021).
•Pharmacotherapy: People with IgE-mediated food allergies can be medicated to relieve the signs and symptoms. These are carefully chosen based on the contribution of IgE-mediated mast cell or basophil degranulation (anti-leukotrienes, epinephrine, antihistamines, anti-IgE, etc.) or T cells or eosinophil activation (steroids, anti-IL5, etc.) to the allergic reaction (Lieberman P, et al., 2010).
a) Epinephrine: The first-line treatment for anaphylaxis is epinephrine. When used in a timely manner, it aids in the reversal of allergic reactions. Epinephrine reduces edema and airway blockage, improves blood circulation, tightens blood vessels, and raises heart rate. If symptoms do not improve in 5-15 minutes after the initial dose, a second dose should be administered (Sicherer SH, et al., 2017).
b) Antihistamines: Antihistamines are used to treat minor allergic reactions, although they do not help with all anaphylactic symptoms. They inhibit the effect of histamine, which induces blood vessel dilatation and leakage of plasma proteins. Diphenhydramine is one of the most regularly used antihistamines for treating food allergies.
c) Glucocorticoid steroids: These are used to reduce the immune system’s effects induced by the release of chemicals as a result of an allergic reaction. These can be given orally or by injection, but the effects are usually sluggish (Sicherer SH, 2006).•Immunotherapy: Immunotherapy is a preventative treatment for allergen-induced allergic responses. Immunotherapy entails increasing the dose of the substance, or allergen, to which the person is allergic over time. Desensitization occurs when a patient can eat a considerable amount of a food allergen without experiencing a reaction as a result of successful immunotherapy. Immunotherapy can also help in rhinitis and asthma by reducing inflammation. The types of immunotherapies used to treat food allergies are listed below (Lucendo AJ, et al., 2014).
a) Oral Immunotherapy (OIT): In this therapy, the patient is given a little amount of food in a limited dose, with the dose rising every two weeks under the supervision of a medical practitioner, in order to achieve a maintenance dose for desensitization (Nurmatov U, et al., 2017).
b) Epicutaneous Immunotherapy (EPIT): This therapy involves applying a patch to the skin that contains a solubilized allergen. This strategy has been found to be effective in the instance of mice and peanuts (Mondoulet L, et al., 2011). These are relatively safe, have little side effects, and are simple to use.
c) Sublingual Immunotherapy (SLIT): This technique of therapy involves placing a liquid or dissolvable pellet containing allergen extracts beneath the tongue and holding it there for a few minutes before eating or spitting it out. As a result, there are little adverse effects, although it isn’t as effective as OIT (Pajno GB, et al., 2018).
Types of food allergies and allergens
Allergies to foods or their components are frequently hereditary and are usually discovered in childhood. Although, there are also various other risk factors focusing the outdoor physical environment which play the major role in the expansion of Food Allergy, for instance vitamin D, air pollution, environmental greenness and pollen exposure (Peters RL, et al., 2022). Because of differences in dietary choices, the prevalence of food allergies is known to vary geographically. Allergic responses can happen to any meal that is taken. In Table 2, the most common food allergies are listed.
| S. No. | Source | Allergens | Symptoms | References |
|---|---|---|---|---|
| 1 | Egg | Gal d 1, Gal d 2, Gal d 3, Gal d 4, Gal d 5 | Swelling, anaphylaxis, sometimes flatulence and vomiting | Caubet JC and Wang J, 2011 |
| 2 | Fish | Aldolase A, Tropomyosin, Beta-enolase, Parvalbumin, Vitellogenin | Anaphylaxis, Oral Allergy Syndrome (OAS), respiratory reactions, sometimes vomiting | Sicherer SH and Sampson HA, 2014; Tong WS, et al., 2018 |
| 3 | Mustard | Sin a 1 (in yellow mustard) Bra j 1 (in brown mustard) | Eczema, rash, hives, facial swelling, abdominal pain wheezing, conjunctivitis, diarrhea, nausea, vomiting, acid reflux, anaphylaxis, dizziness, chest pain, asthma, respiratory problems, | Pesek RD and Jones SM, 2015 |
| 4 | Shellfish | Tropomyosin | Anaphylaxis, respiratory symptoms, Oral Allergy Syndrome (OAS), rhinitis, conjunctivitis, gastrointestinal symptoms, | NHS, 2018 |
| 5 | Milk | Alpha lactalbumin and Beta lactoglobulin, Alpha S1, Alpha S2, Beta and kappa casein | Skin rash, hives, constipation, diarrhea, vomiting, stomach pain, flatulence, colitis, nasal congestion, migraine, dermatitis, blisters, anaphylaxis | Caffarelli C, et al., 2010 |
| 6 | Wheat | Gluten, Albumin, Globulin and Gliadin | Celiac disease, temporary mental incompetence, eczema, hives, asthma, “baker’s asthma”, hay fever, angioedema, abdominal cramps, diarrhea, anemia, nausea, vomiting and exercise induced anaphylaxis | Scherf KA, et al., 2016 |
Table 2: Food, its allergens and the symptoms
Peanut allergy: Peanuts are high in critical nutrients including Vitamin B and E, as well as dietary minerals like phosphorus, manganese, magnesium, and calcium. In comparison to other tree nuts, they have roughly 25 g of protein per 100 g. Although peanuts are high in proteins, fats, and fibers and low in carbohydrates, making them effective in weight-loss diets, a small number of people are allergic to them, making them harmful. It also decreases the quality of life for those who suffer from this allergy, and as a result, it is gradually becoming a major health concern around the world. Because peanut is a legume, it is distinguished from tree nut allergies (Bao Y, et al., 2013). This allergy occurs when a person’s immune system fails to produce a typical hypersensitivity response to peanut proteins. In comparison to other food allergies, it is a leading cause of anaphylaxis and death. Because of the persistence, prevalence, and severity of type 1 hypersensitivity reactions, this allergy is known as the most severe allergy. This allergy can cause fatal systemic reactions in the cardiovascular, genitourinary, respiratory, and gastrointestinal systems. Until present, 13 peanut allergens (Ara h 1-h 13) from seven different protein families have been identified. 95 percent of people with peanut allergies have specific IgE to Ara h 2 (a member of the Colutin family), making it a more potent allergen than Ara h 1 (Belongs to Vicilin family) Ara h 6, which is 59% identical to Ara h 2, has the same allergenicity as Ara h 2 (Koppelman SJ, et al., 2004).
The symptoms are caused by the interaction of IgE and a few other anaphylatoxins, which release histamine from mast cells. The histamine produced causes arteriole vasodilation and bronchiole constriction, resulting in bronchus spasm. The majority of these reactions develop within 20 minutes, and approximately 90% of these reactions include skin manifestations such as redness, rashes, and itching. Anaphylactic attack is the most severe reaction; it is a life-threatening reaction that requires prompt treatment with epinephrine. Breathing difficulties, diarrhea, dizziness, very low blood pressure, swelling of the tongue, lip, and throat, and loss of consciousness are all symptoms of this assault. Acute vomiting, dysrhythmia, laryngeal edema, stomach cramps, and a weak pulse are some of the other prevalent symptoms (Loza C and Brostoff J, 1995).
This allergy originates when a person’s immune system incorrectly recognizes peanut protein as antigen. When dendritic cells recognize peanut allergens as pathogens, they display them on Major Histocompatibility Complex (MHC) Class II receptors, which T lymphocytes recognize. The TH2 cells subsequently proliferate, causing the release of cytokines such as IL-4, IL-5, and IL-13, which attach to IgM subtype cells. IgE, which binds to FcRI on eosinophils, basophils, and mast cells, differentiates as a result of this receptor-cytokine interaction. This induces cell degranulation and the release of chemokines, which produces inflammation and allergy symptoms (Al-Muhsen S, et al., 2003). Peanut allergens cause the immune system to respond by producing IgE antibodies. Some of these peanut allergens may be modified enzymatically or non-enzymatically to make them bind to the ligands on APCs (Antigen Presenting Cells). Glycosylation modifies Ara h 1, which regulates immunological modulatory responses by inducing lectin receptors on dendritic cells, resulting in the production of cytokines and the initiation of a Th2 response. If the person breaths in dust or aerosols containing peanut, such as peanut flower or oil spray, the allergic reaction may begin.
Skin prick tests are used to determine food allergies by recognizing particular IgE linked to cutaneous mast cells. A glycerinated allergen extract is dropped on the patient’s skin in this test. The skin is then pierced with the probe and compared to saline, with the positive allergy test resulting in a 3 mm larger wheal than the saline one. There hasn’t been a solution for this allergy until now, save that person with it should avoid peanuts completely and pay special attention to the food they eat (Koppelman SJ, et al ., 2004). There is also immunotherapy, which appears to diminish allergy sensitivity by exposing people to little amounts of peanuts on a regular basis. In addition, the United States approved a peanut allergen powder in January 2020, which essentially mitigates allergic responses and anaphylaxis that may occur. Despite the fact that this medication has proven to be effective, those who use it must continue to avoid peanuts in their diets. In the event of an anaphylactic reaction, epinephrine injection is the sole treatment that will only treat the reaction; therefore, individuals must carry epinephrine auto injectors such as the Auvi-Q, EpiPen, or Twinject with them at all times. Antihistamines such as Benadryl (diphenhydramine) and loratadine (Claritin) are also effective in the treatment of acute allergic reactions. The issues of peanut allergy can be controlled by educating and informing patients and their families about the symptoms of allergic responses, as well as teaching them how to use injectable epinephrine correctly (Benedé S, et al., 2016).
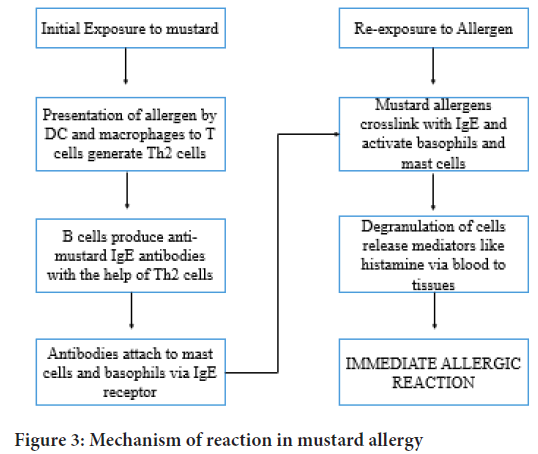
Egg allergy: Because it contains roughly 12% protein and a wide range of minerals, vitamins, and vital amino acids, eggs are considered a nutritious food with a high nutrient density. The nourishment in eggs can be found in both the white and yolk. Proteins, niacin, riboflavin, chlorine, potassium, magnesium, sodium, sulphur, and zinc make up albumin. The yolk is made up of lipids and vitamins such as A, B12, D, E, and folic acid. Copper, calcium, and phosphorus are among the minerals found in it (Caubet JC and Wang J, 2011). Hens’ eggs are a major source of food allergens all throughout the world, with a high frequency in youngsters. The immune system of the body becomes sensitized or overreacts to the proteins found in egg whites or yolks, resulting in an allergy. This allergy is most common in infancy; however, the majority of children outgrow it during their development years (Urisu A, et al ., 2015). There are five main proteins in eggs that have been identified as allergens and are referred to as Gal d 1-5. The protein allergens contained in egg white are Gal d1 (ovomucoid), Gal d2 (ovalbumin), Gal d3 (ovotransferrin), and Gal d4 (lysozyme). The most common allergy is ovomucoid, which has a slim possibility of being outgrown. The egg yolk, on the other hand, contains the Gal d5 allergen, which is alpha-livetin protein, which causes allergic reactions such as rhinitis and asthma. After being heated, several allergens in egg white retain their allergenicity (Caubet JC and Wang J, 2011) (Figure 2).
Figure 2: Allergens present in egg
Allergic reactions in children who are allergic to eggs can range from a slight rash to anaphylaxis. The most common reactions are hives or skin irritation. Other allergic responses include runny nose, sneezing, nasal congestion, nausea, coughing, and shortness of breath. Adult-onset egg allergies are extremely unusual, but there are a few exceptions. Adults may have itching or watery eyes, wheezing or coughing, and swelling of the lips or eyelids (Sicherer SH and Sampson HA, 2014). This allergy can become severe in some situations, affecting the respiratory tract and even blood circulation. Eczema on the scalp, cheeks, and other regions of the body can also affect young children (Pols DH, et al ., 2015). Egg allergy is an IgE-mediated allergic reaction that can cause atopic dermatitis and eosinophilic esophagitis. Egg whites are sometimes referred to as histamine liberators because they cause mast cells to release histamine. This mechanism is classified as a pharmacological reaction and is also known as pseudo-allergy. Because this is not a real IgE-mediated allergic reaction, it is classified as a food intolerance (Al-Saud B and Sigurdardottir ST, 2018).
Eating eggs and foods containing eggs, such as baked or graded foods, meringue, frostings, pastas, and so on, is the obvious cause. Basically, a person’s immune system overreacts to the protein found in eggs, and allergic reactions can be induced even when modest amounts of egg are consumed (Martorell A, et al ., 2013). There is also another source, which is from vaccines, such as influenza vaccines, which are made by incorporating live virus into fertilized chicken eggs, then harvesting and purifying the viruses, but a small amount of egg white proteins remains, which may arouse the immune system of children who are allergic to eggs.
A skin prick test can be used to diagnose this allergy, which is similar to peanut allergy (SPT). Blood tests are also used to determine the amount of IgE antibody present in blood cells. Stopping eating eggs or anything containing eggs is the best strategy to avoid and manage an egg allergy. Because eggs are a hidden element in many foods, people must be vigilant about the food they consume (Tang A, 2003). Antihistamines are used to alleviate the symptoms of a mild egg allergy, and an epinephrine shot is required if an anaphylactic reaction occurs. Prednisone, a glucocorticoid drug, can also be used to prevent Type 1 hypersensitivity. Oral immunotherapy (OIT) for desensitization to egg allergies is currently being researched (Romantsik O, et al ., 2018).
Fish allergy: Humans have relied on fish and fish products as a key source of protein all across the world. It supplies 34 calories per capita per day on average. It is also a good source of fat-soluble vitamins A, D, E, and K, as well as vital fatty acids, which are necessary for proper physiological functioning. Oily fish, which are high in omega 3 fatty acids, can aid to reduce systemic inflammation and lower the risk of cardiovascular disease. Omega 3 fatty acid consumption can also aid to reduce the chance of a deadly heart attack (NHS, 2018). Although fish has a significant nutritional value, it is also one of the eight most prevalent food allergies, which can become serious and lead to death. Fish allergens have been discovered in several regions of the body, including the skin, blood, bones, muscle, and milt (seminal fluid). This allergy is particularly common in children. And it lasts a lifetime. It’s especially common in locations where there’s a lot of seafood consumption. This allergy triggers hypersensitive immunological responses to the proteins found in the fish. Aldolase A, tropomyosin, beta-enolase, parvalbumin, and vitellogenin are some of the most prevalent fish allergies. The most common fish allergen is parvalbumin, which is found in muscle and aids with calcium binding. In humans, its beta subtype has been linked to IgE-mediated allergy reactions. Furthermore, enolase and aldolase have the potential to cause severe allergic reactions (Ruethers T, et al ., 2018).
Fish allergy symptoms are similar to those of other food allergies. Hives, sneezing, headaches, indigestion, diarrhea, nausea, difficulty breathing, stuffy nose, vomiting, and swelling of the lips, tongue, and eyelids are all symptoms. Depending on the person’s immune system, the symptoms may become severe, affecting blood circulation and respiratory tract, causing the person to pass out, and the allergic reaction may result in anaphylactic shock (Prester L, 2016). It is usually brought on by eating fish or using fish products. Also, cutaneous contact with fish allergens, such as inhaling or handling raw fish, might cause allergies.
SPT is similar to other food allergies in that a little amount of allergen is applied to the skin and then analyzed to determine the specific allergen. Anti-parvalbumin antibody is created by the body in reaction to allergens found in fish, and blood antibody tests are used to check for it. The conformation of this allergy is determined by measuring fish specific serum IgE (Tong WS, et al ., 2018). Antihistamines are medications that are recommended to help people avoid allergic reactions. A severe allergic reaction, such as anaphylaxis, necessitates the administration of epinephrine shots.
Mustard allergy: The seeds from the mustard plant (Brassica nigra) are used to make mustard condiments. It can be flavored in whole, cracked, or ground form with lemon juice, water, salt, and vinegar. The taste of the seed is harsh and pungent. It can also be used to season soups, marinate meats, and so on. Mustard seeds are about 4 tsp Kcal and are high in selenium and omega 3 fatty acids. Mustard oil that has been extracted can also be used in a variety of ways. Myrocynase and glucocinolates such as sinalbin and sinigrin are found in the seed. With the help of the myrocynase enzyme, mustard oil is made up of a variety of isothiocyanate chemicals that are generated from glucocinolates (Vidal C, et al., 1991). The varying concentrations of glucocinolate and isothiocyanate in mustard seeds cause different intensities of flavor. Mustard allergy is the most common spice allergy, with high rates in the United Kingdom, Canada, and India. Sin a1 is the most common allergen in yellow mustard, while Bra j1 is the most common allergen in brown or oriental mustard. Any portion of the mustard plant can induce severe allergic reactions, including anaphylaxis. Mustard allergy triggers IgE-mediated responses with a quick onset, affecting the respiratory tract, skin, and gastrointestinal tract within minutes (Pesek RD and Jones SM, 2015). Mustard allergy usually develops before the age of three, and it frequently causes severe symptoms during the first episode of allergic reaction
Even a modest amount of mustard, in any form, can induce a quick increase in histamine levels. The person becomes dizzy and light-headed within a few minutes. Breathing problems, hives, urticaria, itching, vomiting, nasal congestion, stomach pain, nausea, wheezing, and swelling of the face, tongue, nose, and lips are some of the other symptoms the person is experiencing. The victim may also have life-threatening anaphylactic shock (Kanny G, et al., 1995). To diagnose an allergy, SPT or blood tests can be used. Another, more accurate test is to eat a small amount of mustard and progressively increase the amount to see whether you have an adverse reaction. A person with a mustard allergy should always keep an Epi-Pen on hand in case of anaphylactic shock (Figure 3).
Figure 3: Mechanism of reaction in mustard allergy
Shellfish allergy: Shellfish refers to aquatic invertebrates that are consumed as food. It contains mollusk (also scallops, mussels), crustacean (lobsters, shrimps, crabs), and cephalopod (lobsters, shrimps, crabs) tissues (octopus, squid). Shellfish is a term that refers to both marine and freshwater invertebrates that are edible. They come in a variety of meals and styles, such as steamed or fried. Depending on the variety and cooking method, they might have a sweet or briny flavor. They are low in calories but high in good fats (omega 3 fatty acids), minerals, and lean proteins (Venugopal V and Gopakumar K, 2017). Iron, vitamin B12, and magnesium are also abundant in them. A few species of shellfish are high in zinc, which strengthens the immune system and functions as an antioxidant. Aside from the nutritional value of shellfish, a small percentage of people are allergic to the protein found in them and have a hypersensitive immune system. One of the most prevalent food allergens is shellfish proteins. This allergy can start in childhood and continue throughout maturity. Allergic reactions to shellfish allergens can develop as a result of immune system-mediated effects as well as non-immunological activities. Tropomyosin, which acts through an IgE-dependent mechanism, is the most common allergen responsible for crustacean allergy. Because there are so many chemical agents and compounds that might produce an allergic reaction, determining the exact cause of a shellfish allergy is challenging. Shellfish include a small number of possible poisons that can impair the immune system (Thalayasingam M and Lee BW, 2015).
The crustacean group causes the majority of allergic reactions in the shellfish family, and those with this allergy can tolerate mollusks. Shellfish allergy symptoms vary from person to person, and it is not required to have eaten it to have an allergic reaction. The skin, gastrointestinal tract, respiratory tract, and cardiovascular system can all be affected by shellfish hypersensitivity. Dizziness, rashes, indigestion, diarrhea, wheezing, stomach cramps, and difficulty breathing are the most typical symptoms of shellfish allergy. These symptoms can also become life-threatening, leading to anaphylaxis. Other indications of his allergy include cyanosis (pale or blue skin), hoarse voice, weak pulse, cough, swelling of the tongue and lips, and so forth (Tong WS, et al., 2018). If a shellfish allergy is suspected, skin prick tests or blood tests are used to detect for shellfish-specific IgE in the body. Antihistamines such as diphenhydramine can be used to treat this allergy, and prednisone can be used to stop the type 1 hypersensitivity reaction (NHS, 2018). To treat anaphylactic shock, an EpiPen should be carried.
Milk allergy: Milk is the initial food for humans, and it contains various nutritional values that are necessary for body growth and development. It is a nutrient-dense meal generated by mammary glands to supply nutrition (van Winckel M, et al., 2011). Milk can come from a cow, a goat, a buffalo, or a camel. Milk is a necessary component for bone and tooth formation, preventing cardiac problems, and increasing immunity, among other things. Protein, calcium, vitamin A and D, phosphorus, riboflavin, and vitamin B12, zinc, potassium, choline, selenium, and magnesium are all abundant in milk. People experience allergic or hypersensitive reactions despite these benefits and great nutritional value. Milk allergy is an immune system hypersensitivity reaction produced by the alpha-S1 casein protein found in cow milk (Caffarelli C, et al., 2010). Because the symptoms of milk allergy are similar to those of lactose intolerance, they are frequently mistaken or misread. Lactose intolerance occurs when a person lacks the lactase enzyme required for lactose processing (a form of sugar present in milk). One of the top eight food allergies is milk allergy. This allergy develops at an early age, and only a small percentage of children outgrow it.
When milk proteins are heated, they get denatured and lose their 3D shape, reducing their allergenicity. As a result, baked items containing dairy ingredients may be accepted by certain people. Fresh milk, on the other hand, can cause an allergic reaction. Dairy ingestion of even a few milligrams can trigger an IgE-mediated immunological response (Taylor SL and Hefle SL, 2006). Cow’s milk contains six allergenic proteins: alpha S1, alpha S2, beta and kappa casein (casein protein), alpha lactalbumin, and beta lactoglobulin (whey proteins). The symptoms of this allergy vary from person to person, and they usually appear after a few minutes after drinking milk or eating dairy products. Wheezing, itching, hives, coughing, shortness of breath, swelling of the lips, throat, and tongue, abdominal pains, watery eyes, diarrhea, skin rash, sinus infection, bloating, and difficulty swallowing are all signs of this allergy. If the allergy affects the respiratory tract or blood circulation, there is a serious risk of death (Caffarelli C, et al., 2010). Wheezing indicates the impact on the respiratory tract; the airway becomes obstructed, and the person is unable to breathe. When a person’s blood circulation is compromised, his or her pulse becomes weak, and the situation becomes as serious as anaphylaxis. If an anaphylactic reaction is not treated with an epinephrine shot, the person will experience vasodilation, which can result in death in some cases.
The person’s history of allergic responses is used to diagnose this allergy. The SPT method involves putting a tiny drop of milk on the skin and seeing if the skin becomes itchy and red, indicating that the person is allergic to milk (Cuomo B, et al., 2017). In addition, serum IgE specific to milk proteins is evaluated, and a blood test is performed to detect the quantity of antibodies. A component blood test is also available to determine the type of proteins which stimulates the allergic reaction. Oral Immunotherapy (OIT) can be used to desensitize a person (Yeung JP, et al., 2012). Antihistamines are prescribed for mild allergic reactions, and prednisone is given to prevent the late phase of a type 1 hypersensitivity reaction. The person is given an epinephrine shot to lower hypersensitivity in severe allergic reactions, such as anaphylaxis.
Furthermore, the updated guidelines from the European Academy of Allergy and Clinical Immunology (EAACI) recommend avoiding feeding breastfed infant’s regular cow’s milk formula in the first week of life, feeding infants well cooked eggs instead of raw/uncooked pasteurized eggs in their diet, and introducing peanuts in an age-appropriate form as a part of complementary feeding in those populations where there is a peanut allergy (Halken S, et al., 2021).
Wheat allergy: Wheat is a grass that is farmed all over the world for its seed, which is a cereal grain. It belongs to the Triticum genus. It is a significant carbohydrate source. Wheat is in high demand due to its unusual sticky and viscoelastic qualities, which are derived from the gluten proteins found in it. It contains a protein concentration of 13%, which is high when compared to other cereals. It’s a good source of vitamins, minerals, and fiber. Wheat can be crushed into flour or semolina in its natural state. It can also be dried and germinated for the production of malt, or crushed or cut into groats. Wheat husks are also used in a variety of ways. Bread, noodles, biscuits, crackers, pizza, oatmeal, pasta, doughnuts, gravy, vodka, cakes, beer, and breakfast cereals all contain wheat. Wheat contains 327 kcal per 100 gm and is a good source of manganese, niacin, phosphorus, and a few B vitamins. It comprises 71% carbs, 13% water, 1.5 percent lipids, and 75%-80% proteins. Gluten accounts for 13% of the total protein found in wheat. Wheat allergy is characterized by hypersensitivity to the protein found in wheat. Wheat allergy, like all other food allergies, causes an IgE and mast cell reaction. Wheat has various allergenic components, including prolamins, serene protease inhibitors, and glutelin’s, which are the most common allergens among the 27 possible allergens found in wheat (Akagawa M, et al., 2007). The seed storage proteins in wheat are divided into four categories: Albumin, glutelin, prolamin, and globulin. Celiac disease is caused by gluten. Glutenin is divided into nine subunits, each of which is linked to wheat allergies. Allergic reactions can occur after a person consumes wheat or a food product containing wheat, or even after inhaling wheat blossom. Wheat is perceived as a danger by the immune system, which triggers a hypersensitive reaction that can be fatal. Symptoms of an allergic reaction can occur minutes or even hours after intake.
Wheat sensitivity varies from person to person, and allergic reactions are sometimes unpredictable. Even a modest amount can trigger an IgE-mediated allergic reaction, which can progress to anaphylaxis. Eczema, eye irritation, itchiness in the throat or mouth, coughing, hoarse voice, abdominal pain, nausea, diarrhea, vomiting, hives, low pulse rate, redness of the face, difficulty breathing, and even anaphylaxis are all possible signs of this allergy (Lieberman P, et al., 2010). If a person is suspected of having this allergy, SPT is the most common test used to determine gluten sensitivity in wheat. The doctor injects a little quantity of pure wheat protein under the individual’s skin, and if it becomes inflamed or itchy, the allergy is proven. A blood test is another approach for determining if a person has a Food Allergy and measuring IgE levels. The individual should eat a gluten-free diet. A person with modest allergy symptoms should take over-the-counter antihistamines, and in the event of an anaphylactic reaction, the person should be given an epinephrine shot (Scherf KA, et al., 2016; Foong RX and Santos AF, 2021).
Discussion and Conclusion
Food Allergy is a frequent and fatal disorder that impacts the lives of those who suffer from it, as well as their families. Food allergies are on the rise and are impacting both children and adults. The primary precaution to take to avoid this syndrome is to avoid food allergens. There are various measures to avoid developing this illness, such as avoiding high allergy-provoking foods (peanuts, almonds, and eggs) in a pregnant woman’s diet. This is something that needs to be taken into account during the last few months of pregnancy as well as while breastfeeding. As the prevalence of food allergies grows, new models and methodologies are needed to better understand the pathophysiology of IgE-mediated and cell-mediated allergic reactions. Because of its rising incidence, IgE-mediated Food Allergy has become a major clinical issue. The therapist’s assessment is crucial for proper diagnosis and treatment. Diagnostic tests such as a skin prick test, food-specific serum IgE testing, and OIT are performed based on the patient’s history. Food allergies can be treated by avoiding allergen-containing foods and administering epinephrine for allergic reactions as soon as possible, even though immunotherapy has become the gold standard for Food Allergy prevention and treatment. However, even with this strategy, there is a resurgence of Food Allergy after the maintenance dose of the food allergen is stopped, and it also leads to desensitization. In vitro tests, which are commonly employed in the treatment and prevention of food allergies, are critical for assisting immunotherapy without the risk of anaphylactic shock.
References
- Valenta R, Hochwallner H, Linhart B, Pahr S. Food allergies: The basics. Gastroenterology. 2015; 148(6): 1120-1131.
[Crossref] [Google Scholar] [Pubmed]
- Savage J, Sicherer S, Wood R. The natural history of food allergy. J Allergy Clin Immunol Pract. 2016; 4(2): 196-203.
[Crossref] [Google Scholar] [Pubmed]
- Sicherer SH, Sampson HA. Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014; 133(2): 291-307.
[Crossref] [Google Scholar] [Pubmed]
- Rad AH, Maleki LA, Kafil HS, Abbasi A. Postbiotics: A novel strategy in food allergy treatment. Crit Rev Food Sci Nutr. 2021; 61(3): 492-499.
[Crossref] [Google Scholar] [Pubmed]
- Martino D, Joo JE, Sexton-Oates A, Dang T, Allen K, Saffery R, et al. Epigenome-wide association study reveals longitudinally stable DNA methylation differences in CD4+ T cells from children with IgE-mediated food allergy. Epigenetics. 2014; 9(7): 998-1006.
[Crossref] [Google Scholar] [Pubmed]
- Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol. 2010; 125(2): 73-80.
[Crossref] [Google Scholar] [Pubmed]
- Sidbury R, Tom WL, Bergman JN, Cooper KD, Silverman RA, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: Section 4. Prevention of disease flares and use of adjunctive therapies and approaches. J Am Acad Dermatol. 2014; 71(6): 1218-1233.
[Crossref] [Google Scholar] [Pubmed]
- Gernez Y, Nowak-WÄ?grzyn A. Immunotherapy for food allergy: Are we there yet? J Allergy Clin Immunol Pract. 2017; 5(2): 250-272.
[Crossref] [Google Scholar] [Pubmed]
- Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J Allergy Clin Immunol. 2011; 127(3): 668-676.
[Crossref] [Google Scholar] [Pubmed]
- Bute JJ, Bowers C, Park D. Parents’ communication work in the management of food allergies. Health Commun. 2021: 1-10.
[Crossref] [Google Scholar] [Pubmed]
- Skypala I, Venter C. Food hypersensitivity: Diagnosing and managing food allergies and intolerance. John Wiley and Sons. 2009.
- Oyoshi MK, Oettgen HC, Chatila TA, Geha RS, Bryce PJ. Food allergy: Insights into etiology, prevention, and treatment provided by murine models. J Allergy Clin Immunol. 2014; 133(2): 309-317.
[Crossref] [Google Scholar] [Pubmed]
- Vercelli D, Geha RS. Regulation of isotype switching. Curr Opin Immunol. 1992; 4(6): 794-797.
[Crossref] [Google Scholar] [Pubmed]
- Paul WE, Zhu J. How are TH2-type immune responses initiated and amplified? Nat Rev Immunol. 2010; 10(4): 225-235.
[Crossref] [Google Scholar] [Pubmed]
- Pfaar O, Agache I, de Blay F, Bonini S, Chaker AM, Durham SR, et al. Perspectives in allergen immunotherapy: 2019 and beyond. Allergy. 2019; 74: 3-25.
[Crossref] [Google Scholar] [Pubmed]
- Asarnoj A, Nilsson C, Lidholm J, Glaumann S, Östblom E, Hedlin G, et al. Peanut component Ara h 8 sensitization and tolerance to peanut. J Allergy Clin Immunol. 2012; 130(2): 468-472.
[Crossref] [Google Scholar] [Pubmed]
- Groschwitz KR, Hogan SP. Intestinal barrier function: Molecular regulation and disease pathogenesis. J Allergy Clin Immunol. 2009; 124(1): 3-20.
[Crossref] [Google Scholar] [Pubmed]
- IvkoviÄ?-JurekoviÄ? I. Oral allergy syndrome in children. Int Dent J. 2015; 65(3): 164-168.
[Crossref] [Google Scholar] [Pubmed]
- Commins SP, Jerath MR, Cox K, Erickson LD, Platts-Mills T. Delayed anaphylaxis to alpha-gal, an oligosaccharide in mammalian meat. Allergol Int. 2016; 65(1): 16-20.
[Crossref] [Google Scholar] [Pubmed]
- Mojtabavi N, Dekan G, Stingl G, Epstein MM. Long-lived Th2 memory in experimental allergic asthma. J Immunol. 2002; 169(9): 4788-4796.
[Crossref] [Google Scholar] [Pubmed]
- Food Reactions. Allergies. Food Reactions. 2005.
- Bégin P, des Roches A, Nguyen M, Masse MS, Paradis J, Paradis L. Freezing does not alter antigenic properties of fresh fruits for skin testing in patients with birch tree pollen-induced oral allergy syndrome. J Allergy Clin Immunol. 2011; 127(6): 1624-1626.
[Crossref] [Google Scholar] [Pubmed]
- Nowak-WÄ?grzyn A, Katz Y, Mehr SS, Koletzko S. Non-IgE-mediated gastrointestinal food allergy. J Allergy Clin Immunol. 2015; 135(5): 1114-1124.
[Crossref] [Google Scholar] [Pubmed]
- Pabst O, Mowat AM. Oral tolerance to food protein. Mucosal Immunol. 2012; 5(3): 232-239.
[Crossref] [Google Scholar] [Pubmed]
- Spergel JM. Nonimmunoglobulin E-mediated immune reactions to foods. Allergy Asthma Clin Immunol. 2006; 2(2): 1-8.
[Crossref] [Google Scholar] [Pubmed]
- Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001; 2(4): 361-367.
[Crossref] [Google Scholar] [Pubmed]
- Sugimoto M, Kamemura N, Nagao M, Irahara M, Kagami S, Fujisawa T, et al. Differential response in allergenâ?specific IgE, IgGs, and IgA levels for predicting outcome of oral immunotherapy. Pediatr Allergy Immunol. 2016; 27(3): 276-282.
[Crossref] [Google Scholar] [Pubmed]
- Peters RL, Mavoa S, Koplin JJ. An overview of environmental risk factors for food allergy. Int J Environ Res Public Health. 2022; 19(2): 722.
[Crossref] [Google Scholar] [Pubmed]
- Spergel JM, Beausoleil JL, Fiedler JM, Ginsberg J, Wagner K, Pawlowski NA. Correlation of initial food reactions to observed reactions on challenges. Ann Allergy Asthma Immunol. 2004; 92(2): 217-224.
[Crossref] [Google Scholar] [Pubmed]
- NIH. Identifying causes of food allergy and assessing strategies for prevention. National Institute of Allergy and Infectious Diseases. 2018.
- Randhawa S, Bahna SL. Hypersensitivity reactions to food additives. Curr Opin Allergy Clin Immunol. 2009; 9(3): 278-283.
[Crossref] [Google Scholar] [Pubmed]
- Pols DH, Wartna JB, van Alphen EI, Moed H, Rasenberg N, Bindels PJ, et al. Interrelationships between atopic disorders in children: A meta-analysis based on ISAAC questionnaires. PLoS One. 2015; 10(7): e0131869.
[Crossref] [Google Scholar] [Pubmed]
- Keswani T, Patil SU. Basophil activation test in food allergy: Is it ready for real-time?. Curr Opin Allergy Clin Immunol. 2021; 21(5): 442-447.
[Crossref] [Google Scholar] [Pubmed]
- Deschildre A, Lejeune S. How to cope with food allergy symptoms? Curr Opin Allergy Clin Immunol. 2018; 18(3): 234-242.
[Crossref] [Google Scholar] [Pubmed]
- Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010; 126(3): 477-480.
[Crossref] [Google Scholar] [Pubmed]
- Sicherer SH, Simons F, Mahr TA, Abramson SL, Dinakar C, Fleisher TA, et al. Epinephrine for first-aid management of anaphylaxis. Pediatrics. 2017; 139(3): e20164006.
[Crossref] [Google Scholar] [Pubmed]
- Sicherer SH. Understanding and managing your child's food allergies. JHU Press. 2006: 131-134.
- Lucendo AJ, Arias Á, Tenias JM. Relation between eosinophilic esophagitis and oral immunotherapy for food allergy: A systematic review with meta-analysis. Ann Allergy Asthma Immunol. 2014; 113(6): 624-629.
[Crossref] [Google Scholar] [Pubmed]
- Nurmatov U, Dhami S, Arasi S, Pajno GB, Fernandezâ?Rivas M, Muraro A, et al. Allergen immunotherapy for IgEâ?mediated food allergy: A systematic review and metaâ?analysis. Allergy. 2017; 72(8): 1133-1147.
[Crossref] [Google Scholar] [Pubmed]
- Mondoulet L, Dioszeghy V, Vanoirbeek JA, Nemery B, Dupont C, Benhamou PH. Epicutaneous immunotherapy using a new epicutaneous delivery system in mice sensitized to peanuts. Int Arch Allergy Immunol. 2011; 154(4): 299-309.
[Crossref] [Google Scholar] [Pubmed]
- Pajno GB, Fernandezâ?Rivas M, Arasi S, Roberts G, Akdis CA, Alvaroâ?Lozano M, et al. EAACI Guidelines on allergen immunotherapy: IgEâ?mediated food allergy. Allergy. 2018; 73(4): 799-815.
[Crossref] [Google Scholar] [Pubmed]
- Bao Y, Han J, Hu FB, Giovannucci EL, Stampfer MJ, Willett WC, et al. Association of nut consumption with total and cause-specific mortality. N Engl J Med. 2013; 369(21): 2001-2011.
[Crossref] [Google Scholar] [Pubmed]
- Koppelman SJ, Wensing M, Ertmann M, Knulst AC, Knol EF. Relevance of Ara h1, Ara h2 and Ara h3 in peanutâ?allergic patients, as determined by immunoglobulin E Western blotting, basophil-histamine release and intracutaneous testing: Ara h2 is the most important peanut allergen. Clin Exp Allergy. 2004; 34(4): 583-590.
[Crossref] [Google Scholar] [Pubmed]
- Loza C, Brostoff J. Peanut allergy. Clin Exp Allergy. 1995; 25(6): 493-502.
[Crossref] [Google Scholar] [Pubmed]
- Al-Muhsen S, Clarke AE, Kagan RS. Peanut allergy: An overview. CMAJ. 2003; 168(10): 1279-1285.
[Google Scholar] [Pubmed]
- Benedé S, Blázquez AB, Chiang D, Tordesillas L, Berin MC. The rise of food allergy: Environmental factors and emerging treatments. EBioMedicine. 2016; 7: 27-34.
[Crossref] [Google Scholar] [Pubmed]
- Caubet JC, Wang J. Current understanding of egg allergy. Pediatr Clin North Am. 2011; 58(2): 427-443.
[Crossref] [Google Scholar] [Pubmed]
- Urisu A, Kondo Y, Tsuge I. Hen's egg allergy. Chem Immunol Allergy. 2015; 101: 124-130.
[Crossref] [Google Scholar] [Pubmed]
- Al-Saud B, Sigurdardottir ST. Early introduction of egg and the development of egg allergy in children: A systematic review and meta-analysis. Int Arch Allergy Immunol. 2018; 177(4): 350-359.
[Crossref] [Google Scholar] [Pubmed]
- Martorell A, Alonso E, Boné J, Echeverría L, López MC, Martín F, et al. Position document: IgE-mediated allergy to egg protein. Allergol Immunopathol. 2013; 41(5): 320-336.
[Crossref] [Google Scholar] [Pubmed]
- Tang A. A practical guide to anaphylaxis. Am Fam Physician. 2003; 68(7): 1325-1332.
[Google Scholar] [Pubmed]
- Romantsik O, Tosca MA, Zappettini S, Calevo MG. Oral and sublingual immunotherapy for egg allergy. Cochrane Database Syst Rev. 2018; 4(4):CD010638.
[Crossref] [Google Scholar] [Pubmed]
- NHS. Fish and shellfish. National Health Service. 2018.
- Ruethers T, Taki AC, Johnston EB, Nugraha R, Le TT, Kalic T, et al. Seafood allergy: A comprehensive review of fish and shellfish allergens. Mol Immunol. 2018; 100: 28-57.
[Crossref] [Google Scholar] [Pubmed]
- Prester L. Seafood allergy, toxicity, and intolerance: A review. J Am Coll Nutr. 2016; 35(3): 271-283.
[Crossref] [Google Scholar] [Pubmed]
- Tong WS, Yuen AW, Wai CY, Leung NY, Chu KH, Leung PS. Diagnosis of fish and shellfish allergies. J Asthma Allergy. 2018; 11: 247.
[Crossref] [Google Scholar] [Pubmed]
- Vidal C, Diaz C, Sáez A, Rodriguez M, Iglesias A. Anaphylaxis to mustard. Postgrad Med J. 1991; 67(786): 404.
[Crossref] [Google Scholar] [Pubmed]
- Pesek RD, Jones SM. Anaphylaxis in food allergy. Chem Immunol Allergy. 2015; 101: 191-198.
[Crossref] [Google Scholar] [Pubmed]
- Kanny G, Fremont S, Talhouarne G, Nicolas JP, Moneret-Vautrin DA. Anaphylaxis to mustard as a masked allergen in" chicken dips". Ann Allergy Asthma Immunol. 1995; 75(4): 340-342.
[Google Scholar] [Pubmed]
- Venugopal V, Gopakumar K. Shellfish: Nutritive value, health benefits, and consumer safety. Compr Rev Food Sci Food Saf. 2017; 16(6): 1219-1242.
[Crossref] [Google Scholar] [Pubmed]
- Thalayasingam M, Lee BW. Fish and shellfish allergy. Chem Immunol Allergy. 2015; 101: 152-161.
[Crossref] [Google Scholar] [Pubmed]
- van Winckel M, Vande Velde S, de Bruyne R, van Biervliet S. Clinical practice: Vegetarian infant and child nutrition. Eur J Pediatr. 2011; 170(12): 1489-1494.
[Crossref] [Google Scholar] [Pubmed]
- Caffarelli C, Baldi F, Bendandi B, Calzone L, Marani M, Pasquinelli P. Cow's milk protein allergy in children: A practical guide. Ital J Pediatr. 2010; 36(1): 1-7.
[Crossref] [Google Scholar] [Pubmed]
- Taylor SL, Hefle SL. Food allergen labeling in the USA and Europe. Curr Opin Allergy Clin Immunol. 2006; 6(3): 186-190.
[Crossref] [Google Scholar] [Pubmed]
- Cuomo B, Indirli GC, Bianchi A, Arasi S, Caimmi D, Dondi A, et al. Specific IgE and skin prick tests to diagnose allergy to fresh and baked cow’s milk according to age: A systematic review. Ital J Pediatr. 2017; 43(1): 1-10.
[Crossref] [Google Scholar] [Pubmed]
- Yeung JP, Kloda LA, mcDevitt J, Benâ?Shoshan M, Alizadehfar R. Oral immunotherapy for milk allergy. Cochrane Database Syst Rev. 2012; 11(11): CD009542.
[Crossref] [Google Scholar] [Pubmed]
- Halken S, Muraro A, de Silva D, Khaleva E, Angier E, Arasi S, et al. EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Pediatr Allergy Immunol. 2021; 32(5): 843-858.
[Crossref] [Google Scholar] [Pubmed]
- Akagawa M, Handoyo T, Ishii T, Kumazawa S, Morita N, Suyama K. Proteomic analysis of wheat flour allergens. J Agric Food Chem. 2007; 55(17): 6863-6870.
[Crossref] [Google Scholar] [Pubmed]
- Scherf KA, Brockow K, Biedermann T, Koehler P, Wieser H. Wheatâ?dependent exerciseâ?induced anaphylaxis. Clin Exp Allergy. 2016; 46(1): 10-20.
[Crossref] [Google Scholar] [Pubmed]
- Foong RX, Santos AF. Biomarkers of diagnosis and resolution of food allergy. Pediatr Allergy Immunol. 2021; 32(2): 223-233.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Malavika Pillai1, Hina Alim1, Ahmad Ali1 and Nimisha Patel1,2*2Department of Life Sciences, J.C. Bose University of Science and Technology, Haryana, India
Citation: Pillai M: Food Allergies: Their Complications and Treatment
Received: 02-Jan-2023 Accepted: 27-Jan-2023 Published: 03-Feb-2023, DOI: 10.31858/0975-8453.14.2.61-70
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3