Research Article - (2021) Volume 12, Issue 11
Haematological Indices and Obstetric Outcomes among Pregnant Women with Preeclampsia at Iringa Regional Tanzania
Salum Suleimani Luyeko*, Athanase Lilungulu and Maria Angelica RweyemamuAbstract
Introduction: Preeclampsia is a common problem in pregnancy after 20 weeks of gestation age. This is when the systolic blood pressure is 140 and above and diastolic blood pressure is above 90 mm Hg with proteinuria. Hematological system is affected and can result into low platelets, low hemoglobin level, high packed cells volume, and reduced red blood cells; this can result in bad obstetric outcome. This study aimed to assess the hematological indices in preeclampsia and their maternal outcomes.
Objectives: Assessment of Hematological indices and maternal outcomes among women with Preeclampsia.
Material and methods: The study was conducted at Iringa Regional referral hospital, it was cross sectionals study. The sample size was 100 participants. Data were collected by using a well-structured questionnaire which has been tested, the information’s collected. Full blood count investigation done in a Cimex 300 machine.
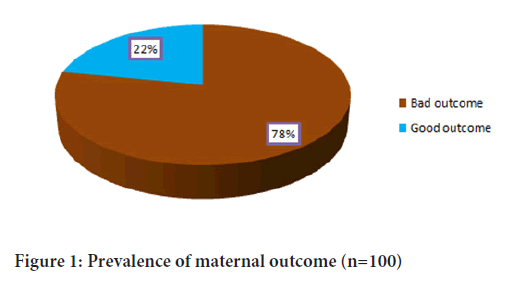
Results: During the study above 18 years of age 44% had diastolic above 160 mm Hg, 44% had platelets below 150, 31% had high hematocrit and 59% had low hemoglobin levels. Among the respondents 78% had bad maternal outcomes. Those with gestation age below 37 weeks are statistically significant with bad maternal outcomes; the blood loss above 500 mls was statistically significant with the bad maternal outcomes
Conclusion: The finding of this study show that the preeclampsia and severe preeclampsia can result into changes in hematological indices and this can result into adverse obstetric outcomes. The study will help to improve better care of the women with preeclampsia and reduce hospital stay.
Keywords
Preeclampsia, Hematological indices, Hematocrit
Introduction
Hypertensive disorders in pregnancy are very common problems in pregnancy with the prevalence of 5%-10%. These are among the causes of maternal and fetal morbidity and mortality, in Sweden the prevalence is 1.5%, 7.5% in Brazil, 3.8% in Ethiopia, 2.6% in Saudi Arabia (Bodur H, et al., 2005). The hypertensive disorders in pregnancy are classified as pre Eclampsia, gestation hypertension, Eclampsia, preeclampsia superimposed in chronic hypertension and chronic hypertension in pregnancy. Preeclampsia is defined as blood pressure of systolic ranging from 140 mmHg and above and diastolic blood pressure of 91 mmHg and above with proteinuria (Maembe LE, 2012). When the blood pressure is 160 and above systolic and 110 and above diastolic with or without sigs of end organ damage like blurred vision, severe headache, epigastric pain, raised serum creatinine, low platelets, and raised liver enzymes which are ALAT and ASAT indicating the severe preeclampsia even if there is no protein in urine.
The cause of preeclampsia is unknown but there are various risk factors which can contribute to the condition which are family history of preeclampsia, primigravida, a woman with history of preeclampsia in previous pregnancy, change of partner in the current pregnancy, obesity, age below 18 years and above 35 years, multiple pregnancy, women with diabetes mellitus and in nulliparity women (Mahande MJ, et al., 2013).The abnormal placentation is due to failure of the trophoblast to penetrate to the spiral vessels which cause the spiral blood vessels failed to be remodeled failure of remodeling of the spiral arteries result into narrowing of blood vessels and ischemia nutrition to the fetus (Tomimatsu T, et al., 2017). Normally the trophoblast penetration to the myometrium start at the 12 weeks of gestation and is completed at 20 weeks of gestation, this is the reason of the preeclampsia to develop after 20 weeks of gestation age, The condition is associated with adverse maternal fetal outcomes like Intra uterine fetal death (IUFD), Intra uterine fetal growth retardation (IUFGR), Low birth weight, early neonatal death, maternal convulsions, prematurity, premature labour, anemia, Hemolysis, elevated Liver Enzymes and low Platelets syndrome (HELP), Postpartum Hemorrhage(PPH), Renal failure, Cardiac failure, abruption placenta (Basak SK, et al., 2015). This abnormal placentation also leads to production of toxic factors in the maternal circulation which result into inflammation and endothelial dysfunction.
This preeclampsia and Eclampsia have multisystem effects, the system which are commonly affected are the central nervous system which there is blurred vision, severe headache, and convulsions, in gastrointestinal system there is liver failure which can result into raised liver enzymes. In Respiratory system there is pulmonary edema. The other system is urinary system which present with anuria and raised serum creatinine.
The hematological system is commonly affected in this there is low platelets, low hemoglobin level, raised hematocrit which are commonly affected (Martanti LE, et al., 2020). The causes of low platelets is due to excessive consumption of the platelets due to endothelial damage, the low hemoglobin level is due to microangiopathic hemolysis and high hematocrit level is due to the contracted circulatory volume following edema (Jhajharia N and Verma M, 2019).
The effects of the preeclampsia and the changes in hematological indices can result into various obstetric outcomes like postpartum hemorrhage, increased caesarean deliveries, maternal death, premature labor intrauterine feta death, low APGAR score, low birth
weight, prematurity, increased NICU admission and early neonatal death. This study is done to assess patterns in hematological indices and associated obstetric outcomes among women with preeclampsia and severe preeclampsia at IRRH.
In Tanzania many studies has been done but not yet published. At Iringa Regional Referral hospital no any study done in hematological indices in preeclampsia and severe preeclampsia. The study will bring good understand of the patterns of hematological indices which will result into better care of the women with preeclampsia and reduce bad maternal outcomes.
Materials and Methods
Study area
It was Hospital based cross sectional study, conducted at Iringa Regional Referral Hospital in antenatal and labor ward. The IRRH is situated in Iringa region located in the southern highland of Tanzania. The region have total area of 35,743 square kilometers, it have 4 administrative districts namely kilolo, Mufindi, Iringa District and Iringa municipal. The region has population of 941238 where 489,186 are females Iringa regional referral hospital have 445 hospital beds, the obstetric wards have 47 beds. There are 3 specialists, 3 medical officers, 2 assistant medical officers 51 nurses of different levels, 8 cleaners. The neonatal resuscitation is done in labor ward and in theatre on a special resuscitation bed. Total number of patients admitted in obstetric ward in 2019 was about 1500 and among them 3500 delivered by caesarean section and 2479 delivered by caesarean section. The participants were obtained in the antenatal ward and labor ward.
Study design
Hospital based cross sectional study conducted from August 2020 to February 2021
Study population
Pregnant women in their 3rd trimester with pre-eclampsia admitted in the antenatal wards and labor ward at IRRH were recruited.
Inclusion criteria
Pregnant women in third trimester with preeclampsia admitted in antenatal attending Labor ward for delivery.
Exclusion criteria
Pregnant women with any medical condition like bleeding disorders, mentally sick, women with history of chronic hypertension, women with Anemia in the current pregnancy and those who refused to participate in the study.
Sample size calculation
The sample size was calculated using the formula as used by Kish and Leslie formula
Where
N=Desired sample size
z=The standard normal deviate, set at 1.96 which corresponds to the 95% confidence limit.
p=Expected population proportion pre-eclampsia in Tanzania which is about 6%
1-p=Proportion of people without condition 0.994%
d=Margin of error (5%).
N=86
Sampling technique
IRRH was chosen purposively. The participants were recruited through convenient random sampling
Data collection
Data was collected by using a prepared questionnaire with wellstructured questions. Those pregnant mothers who fulfilled the criteria’s were enrolled, the convenient sampling technique were employed until the required sample size were achieved. Before collecting the data, all the participants were given a consent form, they passed through it and make sure they understood and signed, those below 18 years their mothers or relatives red the form for them and signed it. Those who didn’t know how to sign they applied the finger print. Those who were unwilling to participate the study they were excluded from the study, Data collection on social demographic characteristics were done. Thorough history taking and physical examination were done to rule out conditions like epigastric pain, severe headache and blurred vision were done, observation to the fetus for the Apgar score and birth weight were done. Blood pressures of the women were checked and invasive procedures of collecting venous blood sample were done. I was responsible for collection of data and sample.
Blood collection, transport and handling
Standard operating procedures established by IRRH and the textbook of diagnostic microbiology were followed during blood collection. The client identification number, age and time of collection of blood sample were labeled on the ethylene diamine Tetra acetic Acid tube. 4.5 ml of blood sample were drawn from the antecubital vein on the anterior part of the arm, equipment like tourniquet, 10 cc syringes and swabs were used during the collection procedure. Prior collection of the blood sample, the anterior cubital vein identified and the site cleaned by sterile swab soaked in spirit and the blood drowned and put in the EDTA tube, after being collected, the samples stored in the cold box and after every one hour the collected samples were taken to laboratory. In the laboratory samples were measured by the hematological machine known as SYSMEX XP 300. The blood in the laboratory is well mixed with in the EDTA tube clean cell pack and stomatolyser. The tube is placed in a plot then the button clicked, then after a time a sound click is heard and the sample removed from the machine and after 30 min the result was red, printed and interpreted.
Independent variables
Independent variables in this study were the preeclampsia.
The intermediate variables
These are investigations or the results of the patterns of hematological indices which are red blood cells counts, platelets count, packed cell volume, hemoglobin level mean corpuscular volume and mean corpuscular hemoglobin concentration.
Dependent variables
These are the obstetric outcomes; maternal outcomes, these are PPH, premature labour, maternal death, mode of delivery and pulmonary edema. Fetal outcomes are admission in NICU, stillbirth, prematurity, low Apgar score below 7 at 5 minutes and early neonatal death.
Data entry and analysis
Data management and quality assurance: Quality assurance procedures were observed during data collection. The collected data was checked if completely filled in the questionnaire at the end of each day during data collection. For full blood count procedure, the IRRH standard operating procedure was strictly observed.
Statistical analysis: All statistical analysis performed using SPSS, version 25.0 (IBM Inc., Chicago). Categorical variables were summarized as the frequency with percentages, while continuous variables summarized as means with standard deviations and range. The p-value, OR, and 95% confidence interval were tested. Factors with significant Odds Ratio (OR) were subjected to binary logistic regression to determine the Adjusted Odds Ratio (AOR).
Ethical clearance: Before conducting the research, I obtained letters of permission from the University of Dodoma, Directorate of Research, and through the Department of Public Health to undertake the study. The proposal discussed at the department and college then submitted for ethical review by UDOM ethical committee under the director of postgraduates. A copy of Ethical clearance was obtained and a copy sent to IRRH management for approval. Strict adherence to rules and regulations during the process of researching to avoid any physical or emotional harm by considering protocol, a complete description of the aims of the study, informed consent of respondent’s and confidentiality of the information sources was maintained.
Women who refused to consent to participate in the study received the same quality of care as the other participants. Advice and reassurance were given to the subjects where appropriate, researcher-designed patient’s identity numbers instead of real names, which remained anonymous, and any participant was free to withdraw from the study at any time when she feel uncomfortable to continue with the study.
Results
This chapter presents the research findings and answers of the questions which were raised before the research and presented in percentage, tables, pie charts and graphs.
Social demographic characteristics of the study participants
Overall respondents this study conducted between June to December 2020 at Iringa Regional Referral hospital there were 100 participants who were pregnant women with preeclampsia in their third trimester of pregnancy. Their age ranged from 18 to 40 years with mean of 25.85 ± 6.85 majority of them (88%) had above 18 years while minority (12%) had 18 or less years of age. More than half of respondents (70%) had primary education or below, and those with secondary education and above were (30%) (Table1). Among those participants (60%) were living in the urban areas while (40%) were living in the rural. Regarding marital status a bit over half were married (68%) and (32%) were not married. (35%) of all respondents were self-employed, (38%) were peasants, (16%) were housewives and only (11%) were employed. During the study (49%) of respondents was primipara, 47 (47%) had 3-4 parity and only four percent had above 4 parity. Among the participants (51%) had gestation age of 37 and above and 49 (49%) had gestation age of below 7 weeks (Table 1).
| Variable | Frequency | Percentage | |
|---|---|---|---|
| Age | 25.85(6.85) | 18-40 | |
| ≤ 18 | 14 | 14 | |
| 19-29 | 53 | 53 | |
| 30+ | 33 | 33 | |
| Education level | |||
| Primary and below | 70 | 70 | |
| Secondary and above | 30 | 30 | |
| Residency | |||
| Urban | 40 | 40 | |
| Village | 60 | 60 | |
| Marital status | |||
| Single | 32 | 32 | |
| Married | 68 | 68 | |
| Occupation | |||
| Housewife | 16 | 16 | |
| Self employed | 35 | 35 | |
| Employed | 11 | 11 | |
| Peasant | 38 | 38 | |
| Parity | |||
| 1 | 49 | 49 | |
| 2-3 | 47 | 47 | |
| 4+ | 4 | 4 | |
| Gestation age in weeks | |||
| <37 | 49 | 49 | |
| 37+ | 51 | 51 | |
Table 1: Demographic characteristics of respondents among women with haematological changes in preeclampsia (100)
Table 2 shows investigations, among 100 respondents, (56%) had systolic blood pressure below 160 mm Hg, and (44%) had systolic blood pressure below 160 mm Hg. Among them, (51%) had diastolic blood pressure below 80 mm Hg and those with diastolic blood pressure above 80 mm Hg were (49%). Among the respondents (47%) had platelets below 150 and about (53%) had platelets 150 or above. In the study, majority (69%) had RBC above 3.5 and (31%) had RBC 3.5 or less. there were (65%) respondents who had PCV below 3.5 and (31%) had PCV 3.5 or above. Regarding HB level, (59%) respondents with Hb level below 11 gm/dl and (41%) had Hb level of 11 gm/dl or above. Majority of respondents (70%) had MCV level below 84 and (30%) of them MCV above 84. Furthermore majority of participants (95%) had MCHC 27 or above meanwhile only five percent of them had MCHC below 27 (Table 3).
| Outcomes | Frequency | Percentage |
|---|---|---|
| Premature labor | ||
| Yes | 49 | 49 |
| No | 51 | 51 |
| Mode of delivery | ||
| SVD | 42 | 42 |
| C/S | 58 | 58 |
| Blood loss in mls | ||
| <500 | 49 | 49 |
| 500+ | 51 | 51 |
| Maternal death | ||
| Yes | 3 | 3 |
| No | 97 | 97 |
| Convulsion | ||
| Yes | 15 | 15 |
| No | 85 | 85 |
Table 2: Maternal outcomes of respondents with haematological indices in pre eclampsia
| Hematologic indices | Frequency | Percentage |
|---|---|---|
| Platelets | ||
| <150 | 47 | 47 |
| ≥ 150 | 53 | 53 |
| RBC | ||
| <3.5 | 13 | 13 |
| 3.5-4.5 | 44 | 44 |
| >4.5 | 43 | 56 |
| PCV | ||
| <35 | 65 | 65 |
| ≥ 35 | 35 | 35 |
| MCV | ||
| <84 | 70 | 70 |
| ≥ 84 | 30 | 30 |
| MCH | ||
| <27 | 46 | 46 |
| ≥ 27 | 51 | 51 |
| MCHC | ||
| <27 | 5 | 5 |
| ≥ 27 | 95 | 95 |
| Hb | ||
| <11 | 54 | 54 |
| ≥ 11 | 46 | 46 |
Abbreviations: PCV: Packed Cell Volume; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Hemoglobin; MCHC: Mean Corpuscular Hemoglobin Concentration
Table 3: Haematological indices among the women with preeclampsia (N=100)
Maternaloutcomes of respondents with hematological indices in preeclampsia
Among 100 respondents included in this study, approximately half of them (49%) had premature labor and (51%) had no premature labor (Table 3). A bit over half of respondents (58%) delivered by caesarean delivery meanwhile (42%) delivered by SVD. Among all respondents (51%) had a history of excessive blood loss during delivery meanwhile (49%) of them had no excessive blood loss during delivery During the study three respondents died and about (15%) developed convulsions (Table 3).
Association of maternal outcome by demographics and other predictors
Table 4 presents association of maternal outcome by several predictors based on chisquare test and fisher’s exact test. It was observed that maternal outcome is significantly associated with gestation age in weeks (p<.0001) and blood loss units (p=0.0485). With respect to gestation age, large proportional of bad maternal outcome was observed among those pre term mothers (97.96%) while those term mothers had proportional of (87.80%). With regard to blood loss units, those respondents who loosed more than 500 units of blood had large proportional of bad maternal outcome (87.80%) as compared those mothers who lose 500 units or less (71.19%). Other factors were not significantly associated with maternal outcome. With regard to parity although were not significant (p=0.7389) those primipara had large proportional of bad outcome (81.63%) as compared to multipara (74.51%).
| Variables | Bad | Good | Chi square | p-value |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age | ||||
| ≤ 18 | 12(85.71) | 2(14.29) | 1.0681 | 0.5862 |
| 19-29 | 42(79.25) | 11(20.75) | ||
| ≥ 30 | 24(72.73) | 9(27.27) | ||
| Education level | ||||
| Primary and below | 53(75.71) | 17(24.29) | 0.7104 | 0.3993 |
| Secondary and above | 25(83.33) | 5(16.67) | ||
| Residency | ||||
| Urban | 34(85.00) | 6(15.00) | 1.9037 | 0.1677 |
| Village | 44(73.33) | 16(26.67) | ||
| Marital status | ||||
| Single | 22(66.67) | 11(33.33) | 3.6867 | 0.0548 |
| Married | 56(83.58) | 11(16.42) | ||
| Occupation | ||||
| Non employed | 12(75.00) | 4(25.00) | - | 0.7477* |
| Employed | 66(78.57) | 18(21.43) | ||
| Parity | ||||
| 1 | 40(81.63) | 9(18.37) | 0.7389 | 0.39 |
| 02-Mar | 38(74.51) | 13(25.49) | ||
| Gestation age in weeks | ||||
| <37 | 48(97.96) | 1(2.04) | 22.3046 | <.0001 |
| 37+ | 30(87.80) | 21(41.18) | ||
| Blood loss units | ||||
| ≤ 500 | 42(71.19) | 17(28.81) | 3.8931 | 0.0485 |
| >500 | 36(87.80) | 5(12.20) | ||
| Systolic blood pressure | ||||
| <160 | 43(75.44) | 14(24.56) | 0.5068 | 0.4765 |
| 160+ | 35(81.40) | 8(18.60) | ||
| Platelets | ||||
| <150 | 40(85.11) | 7(14.89) | 2.6098 | 0.1062 |
| 150+ | 38(71.70) | 15(28.30) | ||
| RBCS | ||||
| <3.5 | 10(76.92) | 3(23.08) | 0.051 | 0.9748 |
| 3.5-4.5 | 34(77.27) | 10(22.73) | ||
| >4.5 | 34(79.07) | 9(20.93) | ||
| PCV | ||||
| <3.5 | 51(78.46) | 14(21.54) | 0.0231 | 0.8793 |
| 3.5+ | 27(77.14) | 8(22.86) | ||
| MCV | ||||
| <81 | 66(77.65) | 19(22.35) | - | - |
| 81+ | 12(80.000 | 3(20.00) | ||
| Hb | ||||
| <11 | 48(81.36) | 11(18.64) | 0.9444 | 0.4221 |
| 11+ | 30(73.17) | 11(26.83) | ||
Table 4: Factors associated with maternal outcome in women with haematological changes in preeclampsia based on cross tabulation (n=100)
Binary logistic analysis in women with hematological changes in preeclampsia for factors associated with maternal outcome.
Binary logistic with unadjusted and adjusted analysis was further used to assess factors associated with maternal outcome; the result is presented in Table 5. It was reviled that in unadjusted analysis maternal outcome was significantly associated with only gestation age in weeks (p=0.0008) whereby those mothers who had 37 or above weeks were significantly less likely to have bad outcome as compared to those below 37 weeks of gestation age (OR=0.030, p=0.0008). In adjusted analysis gestation age in weeks and blood loss units were significantly associated with maternal outcome. With respect to gestation age, those respondents who had 37 or above were significantly less likely to have bad maternal outcome as compared to those with less than 37 weeks of gestation age (AOR=0.025, p=0.0006). With respect to blood loss units, those mothers who loosed more than 500 units of blood were significantly more likely to have bad maternal outcome as compared to those who loose less than 500 units (AOR=3.935, p=0.0385). Others factors like platelets and MCV were not significantly associated with maternal outcome (Table 5) (Figure 1).
| Variable | Unadjusted analysis OR(95%CI) | p-value | Adjusted analysis OR(95%CI) |
p-value | |
|---|---|---|---|---|---|
| Gestation age in weeks | |||||
| <37 | Reference | 0.025(0.003, 0.207) | 0.0006 | ||
| 37+ | 0.030(0.004, 0.233) | 0.0008 | |||
| Blood loss units | |||||
| ≤ 500 | Reference | 3.935(1.076, 14.399) | 0.0385 | ||
| >500 | 2.914(0.978, 8.685) | 0.0549 | |||
| Platelets | |||||
| <150 | Reference | 0.584(0.174, 1.957) | 0.3833 | ||
| 150+ | 0.443(0.163, 1.206) | 0.1112 | |||
| MCV | |||||
| <84 | Reference | 3.606(0.756, 13.426) | 0.075 | ||
| 84+ | 2.250(0.879, 14.801) | 0.1785 | |||
Table 5: Binary logistic analysis for factors associated with maternal outcome haematological among women with preeclampsia (N=100)
Figure 1: Prevalence of maternal outcome (n=100)
Discussion
Patterns of hematological indices in women with preeclampsia
In this study, about (47%) of the respondents had low Platelets count during full blood count, this is a common complication in preeclampsia. This is due to increased consumption of platelets, reduced life span of the platelets and increased aggregation at placenta site due to increased level of Thromboxane A2 (Sultana R, et al., 2012), this is supported by a study done in Ethiopia which say that during the study there were reduction of platelets in women with preeclampsia (Freitas LG, et al., 2013). This is different from the study done in india which says that there is no platelets changes in preeclampsia, if it occur it will be mild and is due to the gestational cause of platelets consumption (Thalor N, et al., 2018). In this study there were(65%) of the respondents with high Packed Cells Volume, another study done in Brazil which says that there is low Platelets in preeclampsia (Freitas LG, et al., 2013), this is due to contracted volume caused by the fluid moving into the interstitial space following damage to the endothelium by the antiangiogenic factors, this is the same with the study done in Taibah university Edina Saudi Arabia which says that there is a raise of Packed cells volume during pregnant in preeclampsia and severe preeclampsia (Elgari MM, et al., 2019), this also is in consistence with another study which says that there is high Hematocrit in Preeclampsia (Bodur H, et al., 2005). Among the respondents (43%) had normal Red Blood Cells, 44% had high RBC’s and 13% had low RBCs, this is due to microangiopathic hemolysis of the Red blood cells This correlate with the result of the study done in Saudi Arabia which says that there was low Hemoglobin level in a preeclampsia and severe preeclampsia pregnant women (Elgari MM, et al., 2019).
Maternal outcomes in women with preeclampsia
During this study, maternal outcomes were assessed for patterns of hematological indices in pregnant women with preeclampsia and severe preeclampsia and results showed that, among those participants (49%) had premature labour, (51%) blood loss more than 500 mls that means Postpartum hemorrhage, most of the respondents delivered by caesarean mode which were (58%) and about 2% had maternal death, there were a study which has been done in South Africa which say that the low hemoglobin level, low platelets and high packed cells volume are the causes of adverse maternal outcomes (Poonyane T, 2015). This is because various outcomes correlate with changes in hematological indices (Rosemary unambya).The other study have the same consistence with this study which says that there is bad maternal outcomes in preeclampsia following low platelets (Bodur H, et al., 2005).
Association between maternal outcomes by hematological indices and other predictors in women with preeclampsia
This study showed that many predictors were associated with bad maternal outcomes. In this study, maternal outcomes were significantly associated with gestation age (p-value of 0.001) and those who had gestation age below 37 weeks are more likely to develop bad maternal outcomes. Maternal outcomes were significantly associated with blood loss below 500 mls (p-value 0.0306), those women with blood loss below 500 mls are more likely to develop bad maternal outcomes.
In this study, maternal outcomes were not significantly associated with platelets (p-value 0.1062) but it showed that those women with platelets count below 150 was more likely to develop the bad maternal outcomes, this finding are similar to the findings obtained in a study done in Dhaka Medical college whereby low platelets can cause maternal mortality and morbidity (Sultana R, et al., 2012), another study done in India which says that maternal outcome were associated with low platelets counts (Chappell LC, et al., 2008). The Maternal outcomes were also not significantly associated with Hemoglobin level, but it showed that those women with hemoglobin level below 11 gm/dl was more likely to develop bad maternal outcomes compared to their counterparts of Hemoglobin level of 11 g/dl and above, this correlate with the results of the study in Beijing Chaoyang Hospital which says that the low Hemoglobin level can cause bad maternal out comes (Gao XJ, et al., 2017), there is another study done in Dhaka Hospital India which reported that the results of Hemoglobin during the study was 11.5 gm/dl and this resulted into bad maternal outcomes (Basak SK, et al., 2015). These studies do not correlate with my study. The maternal outcomes were also not significantly associated with Packed cell volume (pvalue-0.8793) but those women in the study who had high packed cell volume were more likely to develop bad maternal outcomes similar findings occurred in a study done in West Zone Beijing Choyang Hospital which says that the raised packed cell volume is a sign of bad obstetric outcome and predictor in a women with changes in Hematological indices in Preeclampsia and severe preeclampsia (Chappell LC, et al., 2008) other study which correlate with the above findings was done in Dhaka Hospital India where by the hematocrit level was 34 and this resulted into bad maternal outcomes (Basak SK, et al., 2015). The findings are also in consistence with the study done in Bangladesh which says that the maternal outcomes were associated with the high packed cell level (Basak SK, et al., 2015).
Conclusion
This study aimed to find the changes in hematological indices and their maternal outcomes .Based in these study findings, it is clear that patterns in hematological indices in preeclampsia and severe preeclampsia are important parameters to investigate, this will help to improve care of the women with preeclampsia and severe preeclampsia and result into good obstetric outcomes since the abnormalities in hematological indices are responsible for bad obstetric outcomes, Cells blood count investigation is very important in women with Preeclampsia for better care of the women. Further Researches have to be conducted on hematological indices in women with preeclampsia.
Strength of the study
The present study shows a comprehensive observation of hematological indices among preeclampsia mothers and the maternal outcomes.
Moreover, the study provides information on the fact that, this conditions is considered independent risk factors thus hematological indices check can help define the birth outcomes in among the women with preeclampsia and guide interventions to improve the fetal outcomes.
Limitation of the study
The main limitation of the present study was the lack of a long follow-up for neonatal development and the women who had preeclampsia, it was therefore not possible to observe the long-term effects of pre-eclampsia and to correlate these with the various hematological indices studied here.
References
- Bodur H, Tan GT, Ayd BV. Maternal and perinatal outcome in pregnancies complicated with hypertensive disorder of pregnancyâ?¯: A seven year experience of a tertiary care center. 2005; 43-49.
- Maembe LE. Management of preeclampsia/eclampsia in dar es salaam public health facilities: Availability of supplies and knowledge of healthcare workers. 2012.
- Mahande MJ, Daltveit AK, Mmbaga BT, Masenga G, Obure J, Manongi R, et al. Recurrence of preeclampsia in Northern Tanzania: A registry-based cohort study. PLoS ONE. 2013; 8(11). e79116.
- Tomimatsu T, Mimura K, Endo M, Kumasawa K, Kimura T. Pathophysiology of preeclampsia: An angiogenic imbalance and long-lasting systemic vascular dysfunction. Hypertens Res. 2017; 40(4): 305-310.
- Basak SK, Begum K, Rashid M, Yasmin N, Begum H. Haematocrit value in preeclampsia. Bangladesh J Obstet. 2015; 30(2); 80-85.
- Martanti LE, Octaviani DA, Ariyanti I, Prasko P. Hematology profile analysis and birth weight in preeclampsia. 2020; 202: 12010.
- Jhajharia N, Verma M. Hematological changes in pregnancy induced hypertension in their third trimester at Jhalawar Medical college, Jhalawar, India. Int J Reprod Contracept Obstet Gynecol. 2019; 8(9): 3497.
- Sultana R, Karim SMF, Atia F, Ferdousi S, Ahmed S. Platelet count in preeclampsia abstract. J Dhaka Natl Med Coll Hosp. 2012; 18(02): 24-26.
- Freitas LG, Alpoim PN, Komatsuzaki F, Carvalho G, Dusse LMS. Preeclampsiaâ?¯: Are platelet count and indices useful for its prognostic? Preeclampsiaâ?¯: Are platelet count and indices useful for its prognostic? Hematology. 2013; 18(6): 8454.
- Thalor N, Singh K, Pujani M, Chauhan V, Agarwal C. A correlation between platelet indices and preeclampsia. Hematol. 2018; 41(2): 129-133.
- Elgari MM, Khabour OF, Alhag SM. Correlations between changes in hematological indices of mothers with preeclampsia and umbilical cord blood of newborns. Clin Exp Hypertens. 2019; 41(1): 58-61.
- Poonyane T. Impact of severe preeclampsia on maternal and fetal outcomes in preterm deliveries. Doctoral Dissertation. 2015.
- Chappell LC, Enye S, Seed P, Briley AL, Poston L, Shennan AH. Adverse perinatal outcomes and risk factors for preeclampsia in women with chronic hypertension: A prospective study. Hypertension. 2008; 51(4): 1002-1009.
- Gao XJ, Ye CH, Zhao HR, Chen C. Preeclampsia related investigative parameters and its association with maternal outcome. Biomed Res J. 2017; 28(7): 2935-2940.
Author Info
Salum Suleimani Luyeko*, Athanase Lilungulu and Maria Angelica RweyemamuCitation: Luyeko SS: Haematological Indices and Obstetric Outcomes among Pregnant Women with Preeclampsia at Iringa Regional Tanzania
Received: 25-Jun-2021 Accepted: 09-Jul-2021 Published: 16-Jul-2021
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3