Research Article - (2023) Volume 14, Issue 2
Abstract
Objective: Back problems (dorsopathies) are one of the most common locomotor system conditions. Back problems are usually categorised as specific and non-specific back complaints. Specific causes for back problems are hardly ever identified, approximately 90% are non-specific. Back problems lead to pain and reduced functioning. Important symptoms of non-specific back problems are diffuse, nagging pain and reduced physical functioning when carrying out daily activities. The aim of this article is to discuss the results, as reported by the patients, of the current conservative therapeutic treatment of non-specific low back complaints with the use of an orthopaedic corset.
Materials and methods: Patient Reported Outcome Measurement (PROM) study of 677 patients on the effectiveness of wearing an orthopaedic corset in patients with chronic non-specific low back pain was done. Patients with low back pain using corset were asked to complete a questionnaire about the effectiveness of the brace after wearing it for 3 weeks. Primary outcome measure was mobility assessed using an ordinal scale with and without the use of the corset. Secondary outcome measures were pain symptoms and overall daily functioning.
Results: The results demonstrated a 67% improvement in overall daily functioning (positive improvement), and 59% of the respondents reported a reduction in pain. Mobility improved significantly; the group who were only able to walk at home was reduced by 67%, the group who were able to walk to the local shop increased by 72%, and the group who once again were able to go for long walks actually doubled.
Conclusion: The results of this PROM study show that the use of an orthopaedic corset seems to serve as an appropriate joint support, offers pain relief and freedom of movement, and should be considered as a useful non-surgical treatment method for patients with chronic non-specific low back pain.Keywords
Low back pain, Corset, Orthotic devices, Rehabilitation
Introduction
Back problems (dorsopathies) are one of the most common locomotor system conditions. In 2019, almost 600,000 new cases were reported in the Netherlands: 246,400 men and 352,600 women. In addition, over the period of 2011 to 2019, the number of people with symptoms due to degeneration of the intervertebral discs (osteoarthritis/spondylosis of the spinal column) increased by approximately 40% (Nek-en rugklachten, 2022). This is a collection of conditions with diverse or unknown causes. Back problems are usually categorised as specific and non-specific back complaints. Specific back problems are complaints with an attributable physical cause. Examples of this are a spinal disc herniation, osteoporosis, a fracture or a tumour (Pillastrini P, et al., 2012).
Specific causes for back problems are not identified in most cases. For example, of all cases of acute low back pain, approximately 95% are non-specific. Non-specific low back pain means no specific physical cause can be identified. A commonly used hypothesis is that non-specific low back pain is linked with overloading, for example, the intervertebral discs, joints, nerves, and muscles of the spinal column (Bons SC, et al., 2017).
Most people with back problems have non-specific pain (Koes BW and van Tulder MW, 2003). As yet, it is not possible to categorise non-specific back problems on the basis of the exact location of the pain and/or which type of tissue is affected, such as the muscles, tendons, or joints (Oliveira CB, et al., 2018). Although it is clear that back problems are often recurrent, international literature usually categorises the complaints by duration (Koes BW, et al., 2010; Koes BW, et al., 2001)-
• Acute back problems (duration less than 6 weeks)
• Sub-acute back problems (duration 6 to 12 weeks)
• Chronic back problems (duration more than 12 weeks)
The ICD-10 (International Statistical Classification of Diseases and Related Health Problems) makes the following distinctions-
• Ankylosing spondylitis (Bechterew’s disease)
• Other inflammatory spondylopathies
• Spondylosis (osteoarthritis of the spinal column)
• Other spondylopathies
• Conditions of the intervertebral discs (including spinal disc herniation)
• Other dorsopathies, not classified elsewhere
• Dorsalgia
Back problems lead to pain and reduced functioning (Buchbinder R, et al., 2018). Important symptoms of non-specific back problems are diffuse, nagging pain and reduced physical functioning (e.g. due to stiffness) when carrying out daily activities. The Global Burden of Disease study shows that of the 359 conditions studied, low back pain is the condition that leads to the most years lived with disability (Tichenor M and Sridhar D, 2019).
The progress of non-specific back complaints seems favourable in many cases. Approximately 50%-75% of patients recover (mostly) within 6 weeks. It is estimated that approximately 25%-50% of patients develop chronic complaints to a greater or lesser extent (duration of complaints ≥ 12 weeks). The chances of recovery are lower in these patients. Back problems recur more often and more severely in people who have suffered frequent or long-term back problems (Bons SC, et al., 2017; Downie A, et al., 2013).
IQ Healthcare, Radboud University Medical Centre was commissioned by the ministry of health (VWSS) to assess the quality of 16 guidelines for diagnosis and treatment of low back pain and lumbosacral radicular syndrome using the AGREE II tool, as well as to summarise and critically analyse these guidelines for commonalities and differences in recommendations (Brouwers MC, et al., 2010). The guidelines comprise 14 guidelines from the Netherlands, including the Dutch Society for Physiotherapy (KNGF) guidelines on low back pain (2013), the Dutch General Practitioners Association (NHG) standard for non-specific low back pain (2017), the Ketenzorgrichtlijn on low back problems (2010), the NVAB guideline on low back problems (2006), the Zorgstandaard Chronische Pijn (2017), the Behandelkader Pijnrevalidatie (2012), the Dutch Society for Anesthesiology (NVA) guideline on spinal column-related low back pain (2011), and the Dutch Orthopedic Association (NOV) guideline on instrumented spinal column surgery (2017).
Recommendations in first-line and multidisciplinary guidelines largely correspond in terms of diagnosis, risk assessment, and treatment policy. Many guidelines recommend diagnostic triage that distinguishes between non-specific low back pain, lumbosacral radicular syndrome, and specific low back pain. Bed rest is discouraged as a treatment. Recommended medication usually consists of analgesics. In contrast, reassurance, encouraging activity and resumption of work despite possible pain are recommended (Foster NE, et al., 2018).
Many guidelines propose a step-by-step approach (KNGF 2013, NHG 2017, KZ 2010, NVAB 2006, ZS 2017, BP 2013, NICE 2016, KCE 2017) whereby more or different care is recommended if pain and limitations persist. If there is no improvement or recovery, remedial therapy supervised by a physiotherapist or remedial therapist is recommended.
As the final recommended conservative treatment option, the guidelines recommend multidisciplinary treatment. Recommendations in the guidelines for second-line care are more diverse. In this, the perspective of the professional group using the guidelines plays a role, as well as the limited scientific substantiation for diagnostic and therapeutic actions. The NVA and NOV guidelines do emphasise that patients should have completed a conservative pathway prior to being eligible for second-line treatment.
If conservative treatment and even intensive pain rehabilitation offers patients insufficient relief or comfort, these patients have a legitimate care need that could possibly see them turn to pain relief and support from an orthopaedic corset. Incidentally, both the NVA guideline (2011) and the NOV guideline (2017) do not indicate which criteria can be used to determine conservative treatment was unsuccessful.
The recommendations of all 16 guidelines for treatment of low back pain in first-line and multidisciplinary guidelines were analysed, including on the use of corsets if conventional therapy did not yield the desired result. Not utilising corsets and lumbar support is not recommended in any of the Dutch guidelines.
Recommendations for aftercare were absent in almost all of the analysed guidelines. As self-management, positive health and a multidisciplinary biopsychosocial model are important concepts at present, a focus on aftercare should not be lacking: The advice given to the patient to take home and/or to work? The health of the patient is not just the care provider’s responsibility but also that of the patient. This does mean tools should be offered to quantify treatment expectations.
There is little scientific substantiation for the effect of corsets on the daily functioning of patients with low back pain. A Japanese study on the effect of wearing a corset over 6 months showed that the lower back pain was reduced, and no deterioration of muscle strength was found in the paravertebral back muscles (Sato N, et al., 2012).
The aim of this article is to discuss patient-reported outcomes on the use of a corset. This research shows that improvements in Activities of Daily Living (ADL), pain reduction and mobility as perceived by patients are certainly positively stimulated by wearing a corset.
Patients and patient organisations are increasingly engaged in improvements to the quality of care. In many cases, patients wish to play a larger part in their own care pathway and make decisions jointly with their care providers. In addition, patients are more often being considered as partners with respect to the care plan, and care professionals apply the customer experience as a starting point in their advice and actions. In order to arrive at reliable information on the quality and the outcomes of the care provided, it must be measured first. One method is to ask patients about the effect of the care/treatment by way of a patient-reported outcome measurement. Every party benefits from transparency in care-the patient, who receives better care, the care provider, who offers more efficient and effective care, and the healthcare insurer, who can validate the effectiveness of the care received.
Livit Orthopedie, a Dutch provider of orthopaedic and prosthetic services and products, started a study in 2017 on the effectiveness of corsets with the intention of contributing to insight for patients and care providers into the use of corsets.
Materials and Methods
In recent years, there has been an increased focus on placing patients at the center of health care research and evaluating clinical care in order to improve their experience and ensure that research is both robust and of maximum value for the use of care professionals. Patient-Reported Outcomes (PROs) provide reports from patients about their own health, quality of life, or functional status associated with the health care or treatment they have received (Nederland Z, 2021).
This study is limited to people with chronic lower back pain. Between October 2018 and December 2020, 1,782 patients who had been provided with corsets were asked about the effectiveness of the corset 3 weeks after receipt. In all cases, the corset was prescribed to the patients by a medical specialist (physician).
To evaluate the short-and longer-term effects, this research was split into a group of first-time users (short-term effect) and a group of repeat users of a corset to assess the longer-term effects. Repeat users were patients who wore the corset over a period of 3 years. The use was validated by a Certified Prosthetist/Orthotist (CPO). The questionnaires were sent by e-mail and were voluntary. All corsets braces were supplied by Livit Orthopedie.
The questionnaire contained 10 questions, each with a qualitative ordinal scale in terms of pain perception and daily functioning (deteriorated a lot to improve). Mobility was expressed in metres. Patients were required to indicate mobility with and without the corset. The primary outcome measure was mobility, assessed using an ordinal scale with and without the use of a corset. Secondary outcome measures were pain and general daily functioning. Age and gender were also recorded. Patients provided consent when submitting the questionnaire.
The following PROs were defined for this study on the effectiveness of a corset-
• How has your general daily functioning changed since the use of your corset?
• How has your pain symptoms changed since the use of your corset?
• Indicate how mobile you are with/without the corset
The primary outcome measure was mobility, assessed using an ordinal scale with and without the use of a corset. Secondary outcome measures were pain and general daily functioning.
With a population size of 8,000 patients per year who are given a corset, and a confidence level of 95%, an error margin of 4% was determined. This expresses the number of random sampling tests in the results of a questionnaire.
The results are presented in bar charts, frequency tables and percentage distribution of responses in order to analyse the outcome measures (Weldring T and Smith SM, 2013).
Technical information
An orthopaedic corset is a customised aid for parts of or the entire spinal column. A corset can have three different functions, defined by the choice of material and the structure of the corset. The corset can stabilise, correct or immobilise. Within these function groups; there is a distinction in the stiffness of the corset in the way materials are used. Taking this into consideration, the table below describes a type of corset for the different medical conditions listed. The aim of the corset is to ensure general daily activities are less painful or easier to carry out, with the patient’s care need as the key focus.
The orthopaedic corset can be supplied in various versions and materials. It may be that a standard corset is sufficient. If this is not the case, a corset can be made to measure.
Stepped care
The principle of stepped care is an important starting point in general and certainly as part of specialist medical rehabilitation care too. This principle is referred to by the Healthcare Institute Netherlands (ZINL) in the Algemene Beroepskader Revalidatiegeneeskunde van de Nederlandse Vereniging van Revalidatieartsen (VRA) (the general professional framework for rehabilitation medicine by the Dutch association of rehabilitation physicians) (VRA, 2016), the memorandum on Indicatiestelling Medisch Specialistische Revalidatie (Specialist Medical Rehabilitation Care Assessment) by the VRA (VRA, 2016), and the VRA position paper 2015 (VRA, 2015).
Stepped care is a step-by-step plan of increasing intensive types of care, whereby the aim is not to carry out every step but rather to achieve results with as few steps as possible. The stepped care principle means as gently as possible and as intensively as possible. As such, the medical specialist will recommend the most purposeful treatment possible in view of the nature and severity of the issues (Silva DD, et al., 2020).
The stepped care principle works on the premise that the treatment offered is always the most purposeful. This involves an effective treatment that is the least demanding and the cheapest and that suits the nature and severity of the issues. A more intensive intervention is sought only when less intensive intervention yields insufficient results (VRA, 2016).
It is not until treatment, by way of a less complex solution (for example a ready-made corset), has yielded insufficient results or will not yield sufficient results that will it be appropriate for the patient to receive treatment using a customised solution prescribed by a medical specialist. All corsets in this study complied with the requirements for stepped care.
Results
The response rate of this outcome study was 38%; 677 of the 1782 patients completed the questionnaire. All responses were suitable for use. The response rates of online questionnaires varied widely, depending on target group and the nature of the study. The average response rate for e-mail questionnaires fluctuated between 25% and 33% (QuestionPro, 2021).
Table 1shows the demographic data of the research population. Of the respondents, 39% were between 30 and 70 years of age, and 61% were 70 years of age or over. The majority of the respondents in this study (63%) were women.
| N | Total | Female | Male |
|---|---|---|---|
| 677 | 428 | 249 | |
| % | - | 63% | 37% |
| Age (in years) | |||
| <30 | 1% | 0% | 1% |
| 30-60 | 16% | 13% | 17% |
| 60-70 | 23% | 28% | 20% |
| 70-80 | 37% | 43% | 34% |
| >80 | 24% | 16% | 29% |
| Average age (in years) | 72.1% | 72.7% | 71% |
| New patients | 67% | - | - |
| Repeated users | 33% | - | - |
| Co-infection | 32% | - | - |
| Custom made | 68% | - | - |
Table 1: Demographic information of the research population
Patients have been diagnosed with chronic specific low back pain by a medical physician. Patients experienced hardly any improvement in the complaints and experienced increasingly functional limitations, frequent treatments have been without effect, avoidance behaviour occurred and social interaction becomes limited.
The responses are presented below-
How has your general functioning changed since the use of your corset?
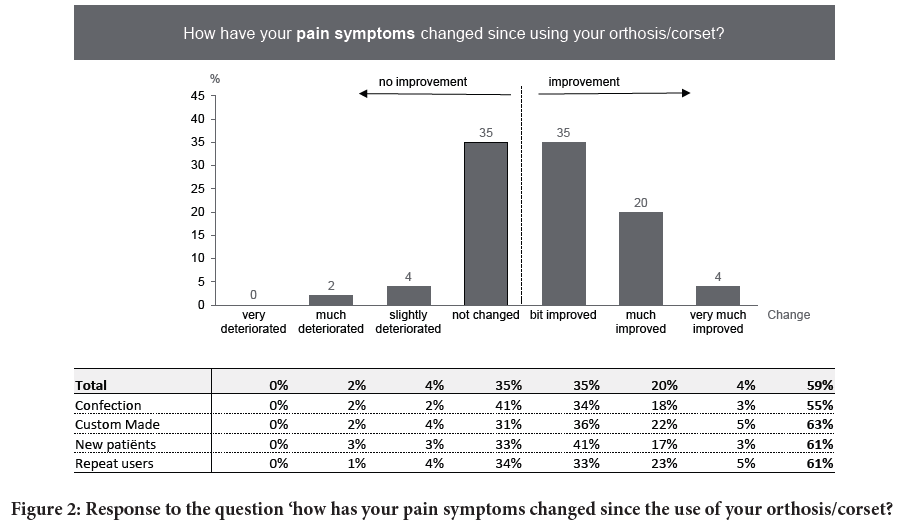
Of the respondents, 67% indicated that their general daily functioning improved with the use of an orthopaedic corset; 29% indicated it had much improved and 5% even indicated it had improved by a lot (Figure 1).
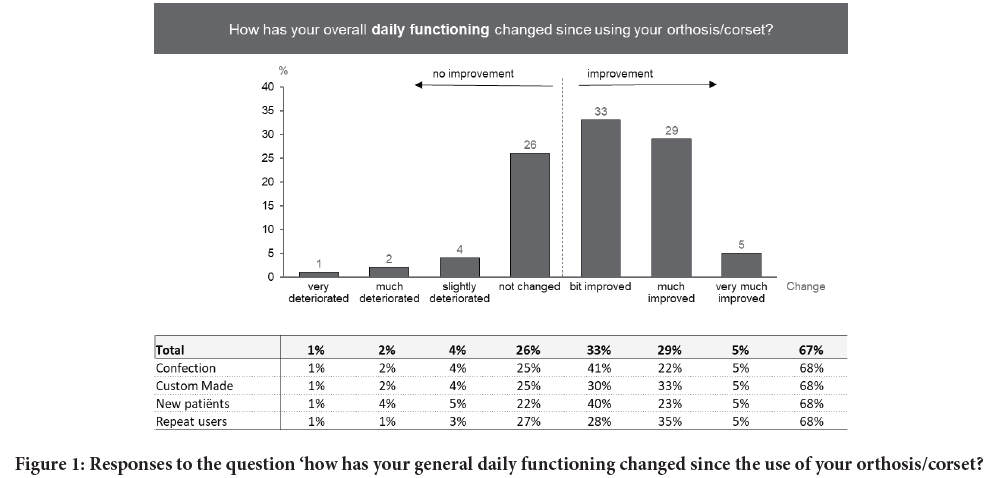
Figure 1: Responses to the question ‘how has your general daily functioning changed since the use of your orthosis/corset?
There is a slight difference between the perceived improvement of patients with a ready-made corset and those with a customised corset; the difference occurred in those patients who indicated that the functioning improved a little and those who indicated it improved a lot. Of the patients with a customised corset, 33% indicated that with use, functioning improved a lot; the comparable percentage was 22% for the group with a ready-made corset. Of the group that indicated functioning had improved a little, 41% had ready-made corsets and 30% had customised corsets.
For patients who started using a corset for the first time or those who were given a repeat aid, the perceived positive effect was virtually equal at 68%. However, the perceived effect in patients with a repeat aid was higher, as a larger number indicated that functioning improved by a lot (35% versus 23%).
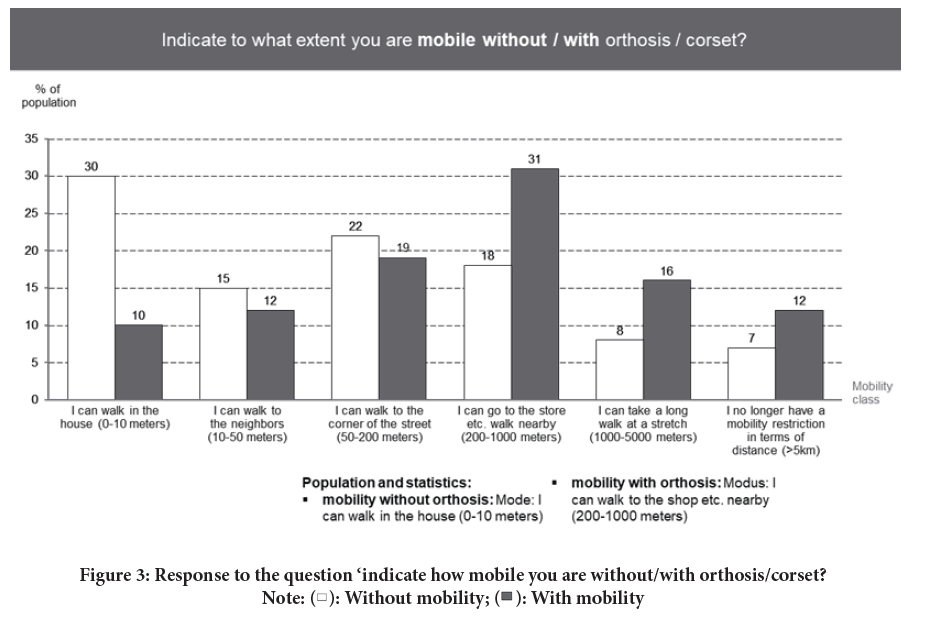
How has your pain symptoms changed since the use of your corset?
The study shows that the pain was reduced and the strain on the back lessened. Figure 2 is a graphic representation showing that the group with a corset had a 59% improvement in pain symptoms. Within this group, virtually no difference in pain reduction was detected between patients who were new to wearing a corset and those who were using a repeat aid. There was an 8% difference between patients with a ready-made corset (55%) and those with a customised corset (63%) who indicated their pain was reduced.
Figure 2: Response to the question ‘how has your pain symptoms changed since the use of your orthosis/corset?
Indicate how mobile you are with and without your corset
Mobility improved significantly: The group who were able to walk only at home was reduced by 67%, the group who were able to walk to the local shop increased by 72%, and the group who were once again able to go for a long walk actually doubled (Figure 3). With this, the mode shifted across three classes, from ‘I am only able to walk around my home’ (30%) to ‘I am able to walk to the local shop’ (31%).
Figure 3: Response to the question ‘indicate how mobile you are without/with orthosis/corset? Note:  : Without mobility;
: Without mobility;  : With mobility
: With mobility
Tables 2 and 3 show the perceived mobility with and without a corset in patients with a ready-made or customised corset and for a first or repeat aid. The perceived mobility improvement for patients with a customised corset was higher than with a ready-made corset. In the higher mobility classes, the changes observed were actually twice as high for those with a customised corset (108%) as they were for those with a ready-made corset (43%).
| Mobility class | I can walk in the house (0-10 meters) | I can walk to neighbours (10-50 meters) | I can walk to the corner of the street (50-200 meters) | I can go to the store etc. Walk nearby (200-1000 meters) | I can take a long walk at a stretch (1000-5000 meters) | I no longer have a mobility restriction in terms of distance (>5 Km) |
|---|---|---|---|---|---|---|
| Total | ||||||
| Mobility without corset | 30% | 15% | 22% | 18% | 8% | 7% |
| Mobility with corset | 10% | 12% | 19% | 31% | 16% | 12% |
| Co-infection | ||||||
| Mobility without corset | 18% | 18% | 25% | 18% | 11% | 10% |
| Mobility with corset | 10% | 9% | 16% | 35% | 19% | 11% |
| Custom made | ||||||
| Mobility without corset | 36% | 14% | 21% | 18% | 7% | 6% |
| Mobility with corset | 10% | 13% | 20% | 29% | 15% | 12% |
| New patient | ||||||
| Mobility without corset | 20% | 17% | 26% | 20% | 10% | 7% |
| Mobility with corset | 11% | 12% | 20% | 32% | 19% | 6% |
| Repeat user | ||||||
| Mobility without corset | 37% | 14% | 19% | 17% | 7% | 7% |
| Mobility with corset | 9% | 12% | 18% | 30% | 14% | 16% |
Table 2: Response to the questions ‘have you noticed an improvement’ specified into type of aid and medical indication
| Low mobility classes | Mobility without corset | Mobility with corset | Change (%) | ||||
|---|---|---|---|---|---|---|---|
| 0-10 meters | 10-50 meters | Total | 0-10 meters | 10-50 meters | Total | ||
| Total | 30% | 15% | 45% | 10% | 12% | 22% | 51% |
| Co-infection | 18% | 18% | 36% | 10% | 9% | 19% | 47% |
| Custom made | 16% | 14% | 50% | 10% | 13% | 23% | 54% |
| New patients | 20% | 17% | 37% | 11% | 12% | 23% | 38% |
| Repeat users | 37% | 14% | 51% | 17% | 7% | 24% | 53% |
| High mobility classes | |||||||
| Total | 8% | 7% | 15% | 16% | 12% | 28% | 87% |
| Co-infection | 11% | 10% | 21% | 19% | 11% | 30% | 43% |
| Custom made | 7% | 6% | 13% | 15% | 12% | 27% | 108% |
| New patients | 10% | 7% | 17% | 19% | 6% | 25% | 47% |
| Repeat users | 7% | 7% | 14% | 14% | 16% | 30% | 114% |
Table 3: Mobility improvement for low and high mobility classes (combined)
Patients with a repeat aid experience significantly improved mobility gains compared to patients who started wearing the corset for the first time. The mode in the patient group with a first aid improved by one mobility class when wearing a corset as opposed to three mobility classes for the patient group with a repeat aid. The change in the group of higher mobility classes was also twice as big (Table 3).
Discussion
Analysis of guidelines for low back pain largely correspond in terms of recommendation to first-line and multidisciplinary guidelines on diagnosis, risk assessment, and treatment policy.
Many guidelines recommend a diagnostic triage, and bed rest is discouraged as a treatment. Recommendations include encouraging activity and resumption of work despite possible pain. Mobility is always more beneficial for recovery than trying to avoid movement that causes back stiffness and only serves to increase the pain. This study supports the use of a corset as an effective alternative treatment therapy for pain reduction when other therapy has not yielded the desired results. The effect on the reduced pain perception by patients was high at 59% and directly contributed to the regained daily functionality that was reported by 67% of patients.
The study by IQ Healthcare recommends focusing future care policy on a strong first line and collaboration between the various disciplines (Brouwers MC, et al., 2010). It is recommended that the outcomes of the effectiveness of the various conservative treatment methods should be included in the new multidisciplinary guideline. Insights into the effectiveness of treatment methods of different disciplines should render the care process for patients more effective.
Patients with a repeat aid experience had significantly improved mobility gains compared to patients who started wearing the corset for the first time. The mode in the patient group with a first aid improved one mobility class when wearing a corset as opposed to three mobility classes for the patient group with a repeat aid. This demonstrates that wearing a corset in the long term yields a perceived positive effect and as such, proves to be an effective therapy. Follow-up research into the duration of corset use could provide additional insight into these findings. Low back pain often has a degenerative course. As far as we are aware, very limited research has been done into the use of a corset in the long term.
A difference was identified between the use of a customised corset and a ready-made corset. The perceived mobility improvement for patients with a customised corset was higher than with a ready-made corset. In the higher mobility classes, the changes observed were actually twice as high for those with a customised corset (greater than 108%) as they were for those with a ready-made corset (more than 43%). This challenges care professionals to take a closer look at the stepped care principle and to realise that the aim of this principle is not to follow every step but rather to achieve results with as few steps as possible. The results of this study give rise to the hypothesis that health care professionals often follow the entire step-by-step plan. The default prescription is more often a ready-made corset, followed by a customised corset if the intended goal has not been reached, and there is a reluctance to shorten the step-by-step plan and move to a customised corset straight away. It would be interesting to carry out follow-up research into patients with ready-made corsets who experience fewer effects to refine the diagnostic process and shorten the stepped care process. A limitation of this study is that no information was available on deformities of the lower back. These could have an impact on the effect of the corset.
Unlike common opinion in practice, research shows that wearing a corset brace does not have a negative effect on muscle strength, muscle endurance, and muscle and tendon stiffness (Foster NE, et al., 2018; Sato N, et al., 2012). This study supports this finding and shows that the use of an orthopaedic corset can clearly yield improved mobility. The group who are able to walk only at home was reduced by 67%, the group who were able to walk to the local shop increased by 72%, and the group who were once again able to go for a long walk actually doubled. The improvement of mobility is the objective of all guidelines for low back pain (Brouwers MC, et al., 2010), and the use of an orthopaedic corset is a proven effective aid in this respect.
Conclusion
The results of this large-scale PROM study on the effectiveness of wearing an orthopaedic corset shows that its use contributes to the reduction of pain and therefore improvements in general daily functioning and mobility. Reduced complaints mean that patients can move more easily with less pain and improve their quality of life.
This study shows that the use of an orthopaedic corset seems to serve as a suitable support, reducing complaints and offering freedom of movement. We hope this study contributes to the insight into the expected effect of an orthopaedic corset for low back pain that can be used by professionals in the management of patients’ expectations in daily practice.
References
- Volksgezondheid en Zorg Info. Nek-en rugklachten. 2022.
- Pillastrini P, Gardenghi I, Bonetti F, Capra F, Guccione A, Mugnai R, et al. An updated overview of clinical guidelines for chronic low back pain management in primary care. Jt Bone Spin. 2012; 79(2): 176-185.
[Crossref] [Google Scholar] [Pubmed]
- Bons SC, Borg MA, van den Donk M, Koes BW. NHG-standaard Aspecifieke lagerugpi n (M54). 2017.
- Koes BW, van Tulder MW. Evidence-based handelen bij lage rugpijn: Epidemiologie, preventie, diagnostiek, beh. en richtlijnen. Bohn Stafleu van Loghum; 2003.
- Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CW, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur Spine J. 2018; 27(11): 2791-2803.
[Crossref] [Google Scholar] [Pubmed]
- Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010; 19(12): 2075-2094.
[Crossref] [Google Scholar] [Pubmed]
- Koes BW, van Tulder MW, Ostelo R, Burton AK, Waddell G. Clinical guidelines for the management of low back pain in primary care: An international comparison. Spine. 2001; 26(22): 2504-2513.
[Crossref] [Google Scholar] [Pubmed]
- Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: A call for action. The Lancet. 2018; 391(10137): 2384-2388.
[Crossref] [Google Scholar] [Pubmed]
- Tichenor M, Sridhar D. Metric partnerships: Global burden of disease estimates within the world bank, the world health organization and the institute for health metrics and evaluation. Wellcome Open Res. 2019; 4.
[Crossref] [Google Scholar] [Pubmed]
- Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RW, de Vet HC, et al. Red flags to screen for malignancy and fracture in patients with low back pain: Systematic review. Bmj. 2013; 347.
[Crossref] [Google Scholar] [Pubmed]
- Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010; 182(18): E839-42.
[Crossref] [Google Scholar] [Pubmed]
- Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. The Lancet. 2018; 391(10137): 2368-2383.
[Crossref] [Google Scholar] [Pubmed]
- Sato N, Sekiguchi M, Kikuchi S, Shishido H, Sato K, Konno S. Effects of long-term corset wearing on chronic low back pain. Fukushima J Med Sci. 2012; 58(1): 60-65.
[Crossref] [Google Scholar] [Pubmed]
- Nederland Z. PROM-toolbox: PROM-wijzer en PROM-cyclus. 2021.
- Weldring T, Smith SM. Article commentary: Patient-Reported Outcomes (PROS) and Patient-Reported Outcome Measures (PROMs). Health serv insights. 2013: 6: 61-68.
[Crossref] [Google Scholar] [Pubmed]
- Algemene beroepskader revalidatiegeneeskunde. Nederlandse Vereniging van Revalidatieartsen (VRA). 2016.
- Position paper revalidatiegeneeskunde. Nederlandse Vereniging van Revalidatieartsen (VRA). 2015.
- Indicatiestelling medisch specialistische revalidatie. Nederlandse Vereniging van Revalidatieartsen (VRA). 2016.
- Silva DD, Pazzinatto MF, Crossley KM, Azevedo FM, Barton CJ. Novel stepped care approach to provide education and exercise therapy for patellofemoral pain: Feasibility study. J med Internet res. 2020; 22(7): e18584.
[Crossref] [Google Scholar] [Pubmed]
- Survey response rate: What it is and how to make it better. QuestionPro. 2021.
Author Info
Tim Dries1, Jan Willem van Der Windt2*, Wouter Akkerman2, Leen Nugteren3, Marco Toor4 and Bram Hentenaar52Livit Orthopedie, Amsterdam, Netherlands
3Livit Orthoepdie, Rotterdam, Netherlands
4Livit Orthopedie, Den Haag, Netherlands
5Department of Orthopedics, Diakonessenhuis Hospital, Utrecht, Netherlands
Citation: Dries T: Improved Mobility and Reduced Pain When Wearing a Corset for Patients with Chronic Low Back Pain
Received: 20-Jan-2023 Accepted: 03-Feb-2023 Published: 10-Feb-2023, DOI: 10.31858/0975-8453.14.2.98-104
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3