Case Series - (2023) Volume 14, Issue 5
Abstract
Background: Pilon fractures remain among the most frequent articular fractures, often secondary to a high-energy trauma, associated in the majority of cases with other bone lesions (fracture of the external malleolus and the dome of the talus). Thus, the soft tissue lining (thin and fragile) surrounding the distal leg may be open in open fractures or may be the site of suffering. the extent of which may vary in the case of a closed fracture, constituting in both cases a factor that will condition the choice of treatment, which must in all cases respect the state of the skin and not aggravate suffering that has already occurred.
Materials and methods: We present in this work our experience with a series of 57 cases admitted between 2013 and 2023 in our trauma department for the management of a pilon fracture, in which different therapeutic attitudes were adopted (minimally osteosynthesis, internal plate osteosynthesis, external osteosynthesis, orthopedic treatment). This period of 10 years allowed us to have a medium and long-term follow-up of our patients recorded on our own computerized medical record system.
Results: This study allowed us to open our minds to other surgical techniques, in particular minimal osteosynthesis for the management of pilon fractures. Indeed, this technique applied in 45.6% of our patients, allowed us to obtain very good results (84.5% of the fractures were consolidated after an average of 4 months). In terms of the quality of the bone reduction and the restoration of the articular surface, as well as in terms of function and complications (0% of material infection, 0% of skin necrosis and 0% of septic pseudarthrosis).
Conclusion: The condition of the skin opposite the tibial pilon, whether open or in pain, is an imperative condition for the choice of therapeutic method, which gives considerable value and place to minimally invasive osteosynthesis, especially when it allows intraoperative good bone reduction and good reconstruction of the articular surface.
Keywords
Tibial pilon, Fracture, Minimally invasive, Osteosynthesis
Introduction
Tibial pilon fractures are fractures in which the line is located in the metaphyseal and epiphyseal region of the lower end of the tibia. The degree of complexity of the fracture, the involvement of the articular surface and the condition of the skin opposite determine the degree of complexity of management of this type of fracture, as well as the prognosis of these fractures (Plaweski S, et al., 1999). Pilon fractures are due in the majority of cases to a high-energy trauma (road accident remains the first etiology in Morocco).
The mechanism essentially associates an axial compression force with accessory forces (dorsal or plantar hyperflexion, adduction or forced abduction); all of which result in depression at the point of impact and associated lesions (fracture of the external malleolus, the talus, skin lesions, etc.).
Pilon fractures are among the therapeutic emergencies that must be managed as soon as possible before the aggravation of skin damage that is characterized by evolutivity even in case of immobilization of the fracture (Plaweski S, et al., 1999). Therefore, taking into account the different factors (the skin condition of the distal quarter of the leg, the complexity of the fracture and the associated lesions), does minimally closed osteosynthesis solve the problem by allowing both a satisfactory reduction and stabilization of the fracture without opening up or aggravating an already existing skin condition.
Case Representation
In this work, we report the experience of the trauma and orthopedics department at the Mohammed VI University Hospital in Oujda, with a series of 57 patients admitted to the department for management of a tibial pilon fracture. 26 cases were treated with minimal osteosynthesis (pinning and/or percutaneous screwing), protected by an external fixator or a plaster cast. Moreover, 18 cases were treated with internal plate osteosynthesis, while 8 cases were treated with an isolated external fixator and five cases with orthopedic therapy.
All patients had a complete clinical examination with a standard radiograph of the ankle in front and side view along with a radiograph of the homolateral knee in front and side view. Thus, 70% of the cases had a scanner of the ankle with three-dimensional reconstruction. For therapeutic management, all patients were treated surgically and were operated with spinal anesthesia. For the 26 cases treated by minimal osteosynthesis, they underwent reduction under fluoroscopic control by external maneuvers (traction in the axis associated with rotational movements). The reduction obtained was maintained by percutaneous screwing (associated in 60% of the cases with pinning on demand). This minimal osteosynthesis was protected by an external fixator in 30% of the cases, and by a posterior plaster splint in 70% of the cases. For the 18 patients treated with internal osteosynthesis, the focus was approached anterointernal with open fracture reduction and stabilization of the reduction with a trefoil plate. For the eight patients treated with external fixators, a full-frame Hofmann fixator was used, positioned between tibia and calcaneus. A standard postoperative radiograph of the ankle in the front and side view checked the fixation.
Results
A minimum follow-up of 1 year for all cases was obtained, based on our own computerized medical record system. 57 patients were evaluated after a mean period of 73 months (15 to 132 months). In terms of gender, 74% of the patients were male and 26% were female. 80% of the patients were admitted as a result of road accidents, 90% of which were motorcycle accidents.
In our series, 74% of the fractures were closed fractures, for which the degree of skin damage was assessed by the Tscherne classification (59.5%: Stage 0, 33.3%: Stage 1 and 7.2%: Stage 2). Similarly 26% of the cases were having a skin opening, for which the degree of damage was assessed by the Cauchoix and Duparc classification and the Gustilo classification (33.3%: Stage 3, 53.3%: Stage 2 and 13.4%: Stage 1).
For the radiological assessment, all patients had a standard radiograph of the ankle in front and side view with front and side view of the homolateral knee. In our patients, 74% of the tibial pilon fractures were associated with a fracture on the lateral malleolus. Different types of fractures were classi- fied according to the AO classification (Figure 1).
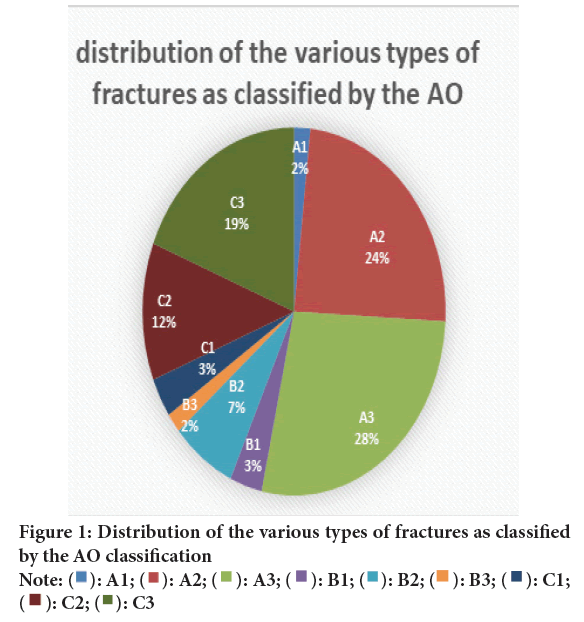
Figure 1: Distribution of the various types of fractures as classified
by the AO classification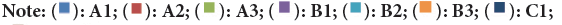
In the series of 26 cases treated with minimally invasive osteosynthesis, anatomical reduction of the fracture site and the tibiotalar articular surface was achieved in 50% of the cases while perfect reduction was not achieved in 41% of the cases but the set-up allowed contact between the edges on either side of the fracture site. More than 70% of reduction was accepted, with reconstruction of a correct tibiotalar articular surface (Figures 2 and 3). Thus, in this series of patients treated by minimal osteosynthesis, 84% had consolidation of the pilon after an average of 4 months after the operation (Figure 4). Thus, there were no cases of material infection or pseudarthrosis of septic origin, nor of skin necrosis (Figure 5).
Figure 2: (A) Initial view; (B) With initial radiographs in frontal; (C) Lateral view; (D) Postoperative clinical appearance; (E) Postoperative radiographic control in frontal view; (F) Lateral view
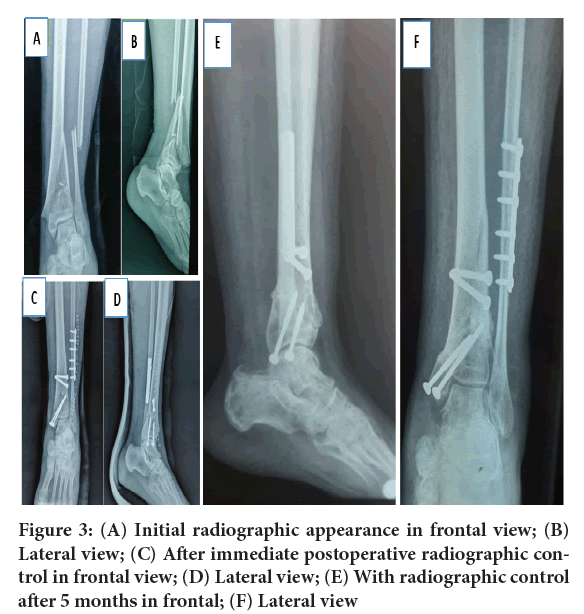
Figure 3: (A) Initial radiographic appearance in frontal view; (B) Lateral view; (C) After immediate postoperative radiographic control in frontal view; (D) Lateral view; (E) With radiographic control after 5 months in frontal; (F) Lateral view
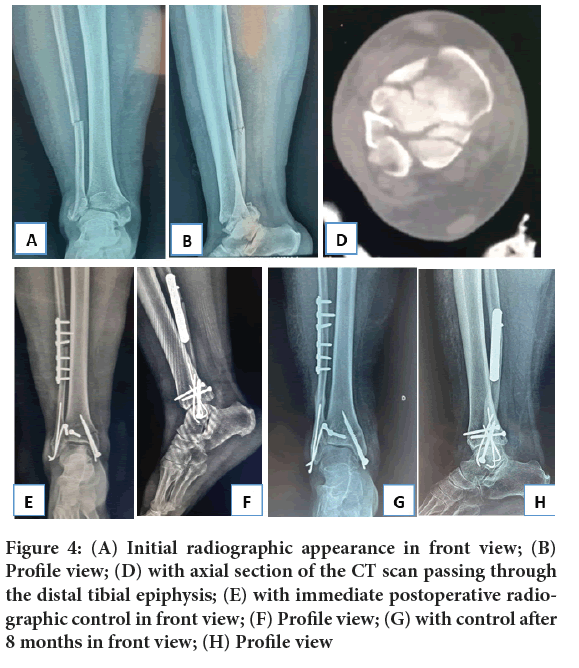
Figure 4: (A) Initial radiographic appearance in front view; (B) Profile view; (D) with axial section of the CT scan passing through the distal tibial epiphysis; (E) with immediate postoperative radiographic control in front view; (F) Profile view; (G) with control after 8 months in front view; (H) Profile view
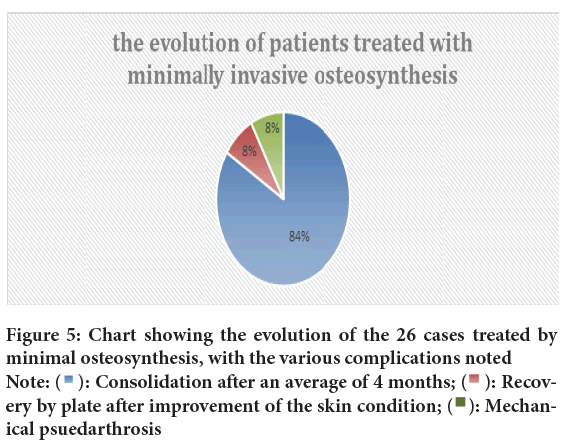
Figure 5: Chart showing the evolution of the 26 cases treated by
minimal osteosynthesis, with the various complications noted  ery
ery
by plate after improvement of the skin condition;
For the evolution of 18 cases treated by internal plate osteosynthesis, 55.5% had consolidation. After an average duration of 4 months (Figure 6), we had complications among which 4 cases were sepsis on material including 3 cases of septic pseudarthrosis and these 3 cases of septic pseudarthrosis benefited from a two-stage management according to the technique described by Masquelet (induced membrane technique). Figures 7-9, show the evolution of a case of septic pseudarthrosis that was managed according to the Masquelet technique.
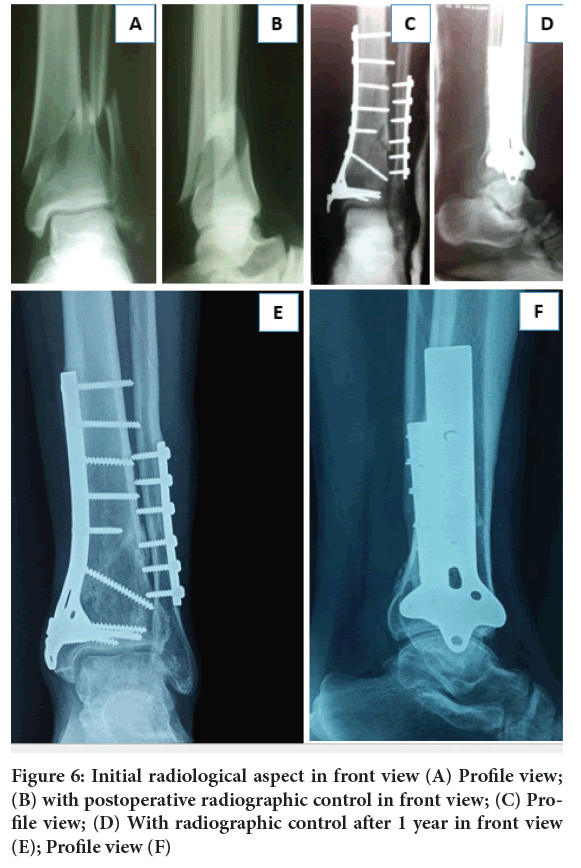
Figure 6: Initial radiological aspect in front view (A) Profile view; (B) with postoperative radiographic control in front view; (C) Pro- file view; (D) With radiographic control after 1 year in front view (E); Profile view (F)
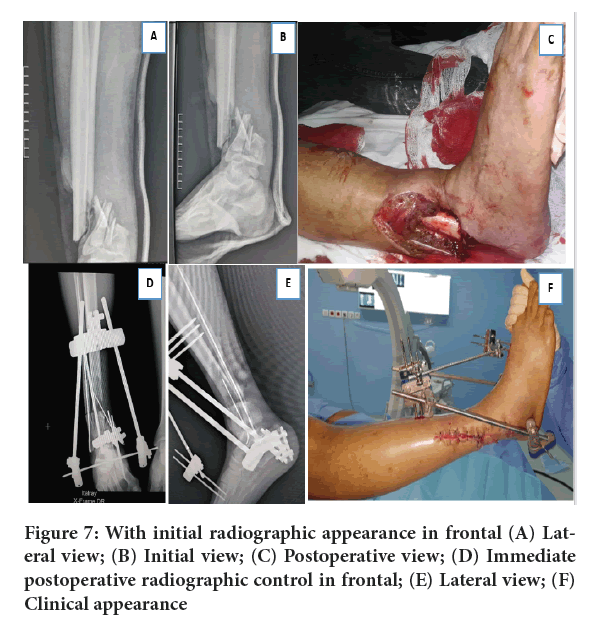
Figure 7: With initial radiographic appearance in frontal (A) Lateral view; (B) Initial view; (C) Postoperative view; (D) Immediate postoperative radiographic control in frontal; (E) Lateral view; (F) Clinical appearance
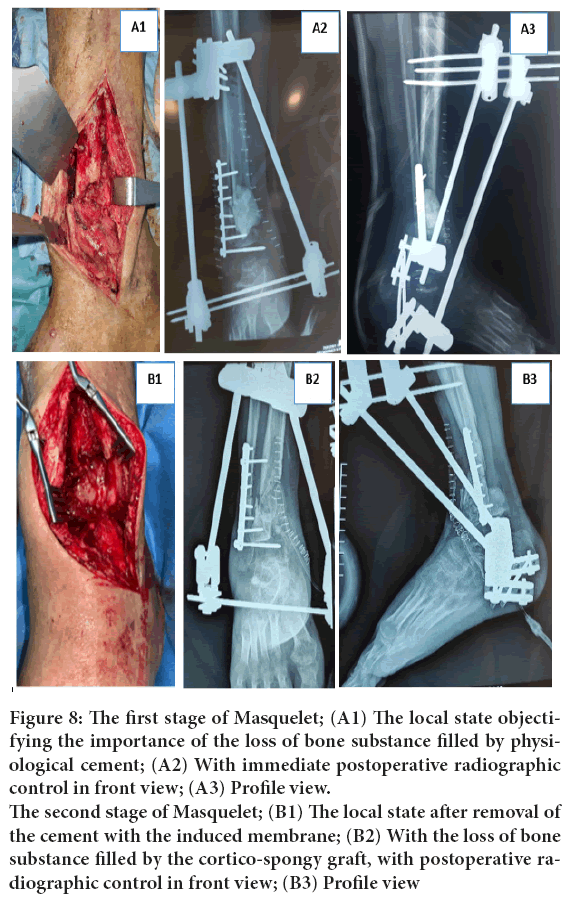
Figure 8: The first stage of Masquelet; (A1) The local state objectifying
the importance of the loss of bone substance filled by physiological
cement; (A2) With immediate postoperative radiographic
control in front view; (A3) Profile view. The second stage of Masquelet; (B1) The local state after removal of
the cement with the induced membrane; (B2) With the loss of bone
substance filled by the cortico-spongy graft, with postoperative radiographic
control in front view; (B3) Profile view
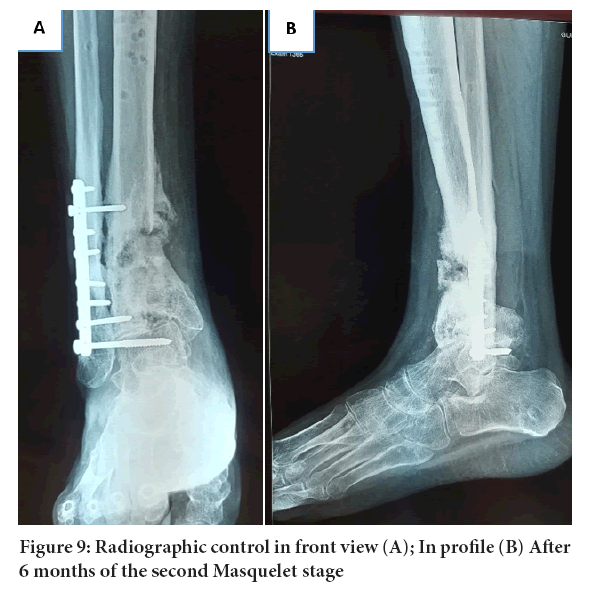
Figure 9: Radiographic control in front view (A); In profile (B) After 6 months of the second Masquelet stage
In the series of eight patients treated with a definitive external fixator, bone consolidation was achieved after an average of 4 months (Figure 10). Thus, five cases with non-displaced tibial pilon fractures were treated with orthopedic immobilization using a circular plaster cast for a period of 6 weeks (knee release after 3 weeks). The functional outcome of the four series of patients included in this study was evaluated by the AOFAS (the American Orthopedics Foot and Ankle Score) (Figures 11 and 12).
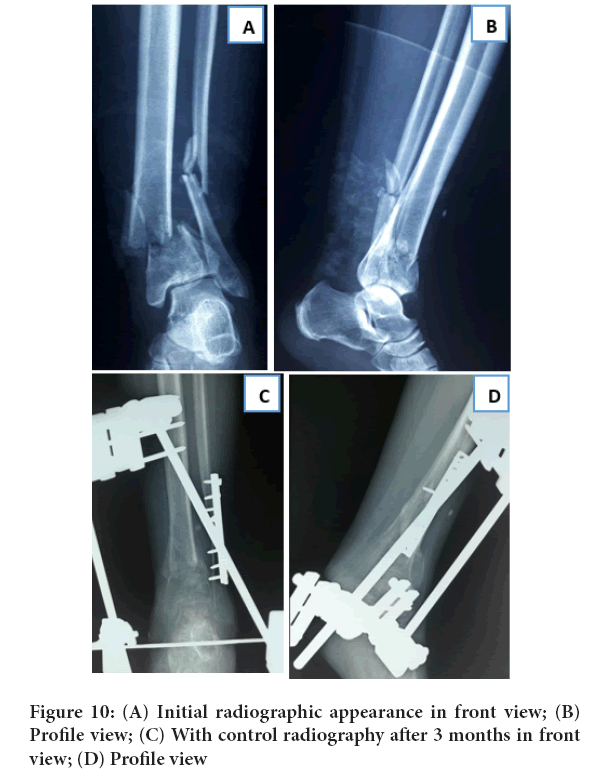
Figure 10: (A) Initial radiographic appearance in front view; (B) Profile view; (C) With control radiography after 3 months in front view; (D) Profile view
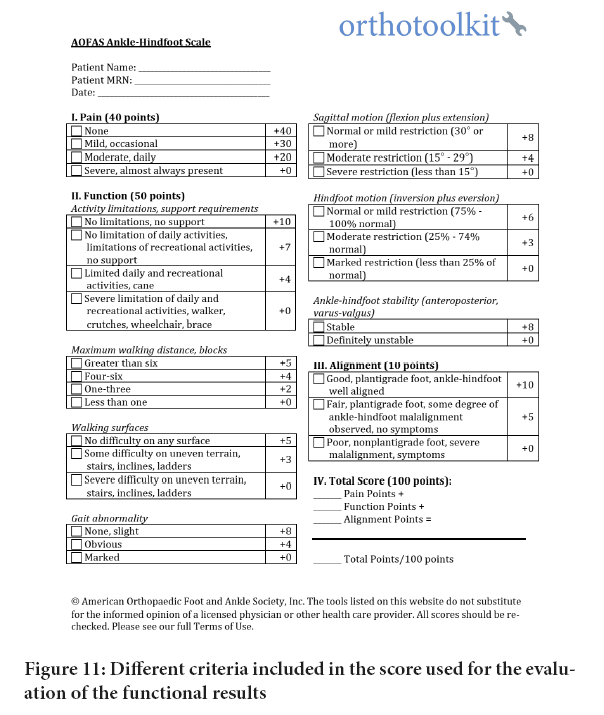
Figure 11: Different criteria included in the score used for the evaluation of the functional results
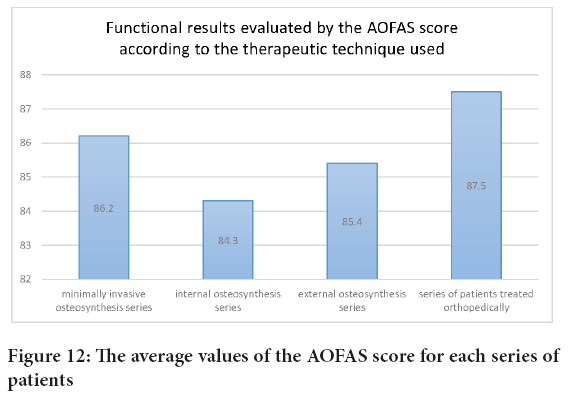
Figure 12: The average values of the AOFAS score for each series of patients
Discussion
Despite the progress that has revolutionized trauma and orthopedic surgery (in terms of diagnostic, therapeutic, physical therapy, and postoperative rehabilitation, which will determine the outcome of the treatment), pilon fractures are still the most difficult joint fractures to treat. This diffi- culty is linked not only to the epiphyseal location of this type of fracture, with all the problems encountered in reconstructing the articular surface, which in most cases evolves into osteoarthritis but also to the soft tissue representing the envelope of the distal leg, which is thin and fragile. It generally suffers significantly in the majority of distal tibia fractures, and determines the therapeutic method, which must never aggravate this suffering (Plaweski S, et al., 1999). Thus, the degree of complexity of the fracture and the associated bony lesions (fracture of the lateral malleolus and the talus) guide the choice of the therapeutic attitude, which must ensure a normal axis and languor and eliminate all rotation disorders. All the factors involved in the management of pilon fractures constitute a challenge for the surgeon who must ensure a reduction with the most anatomical reconstruction possible for the tibiotalar articular surface without aggravating skin suffering. Moreover, for this, the surgeon will be obliged to initiate external fixation whenever possible with or without minimal osteosynthesis depending on the type of fracture. Osteosynthesis of the pilon is not an easy task from a technical point of view for the surgeon and it depends on the experience and habit of the surgeon, who must in all cases put before him or her all the possible therapeutic modalities, and must take into account all the factors involved in the choice of therapy, in particularly about the condition of the skin.
In this work, we reviewed the history of our service with these fractures, in front of which we adopted different surgical techniques (external fixation, internal osteosynthesis by plate, minimal osteosynthesis, orthopedic treatment), this review allowed us to evaluate and compare the results obtained for each technique. Indeed, this study has shown the importance of minimally invasive osteosynthesis of pilon fractures, especially complex fractures and fractures with significant skin damage. This has been proven to obtain excellent results in patients benefiting from this therapeutic attitude. In this series of 26 cases treated by minimal osteosynthesis (percutaneous screwing and/or percutaneous pinning protected by a plaster cast or external fixator), the technique respects the fragile skin envelope of the ankle, and the challenge of not aggravating skin damage (0% skin necrosis). Thus, the local skin condition of all patients evolved very favorably after an average of two weeks postoperatively, allowing open revision only in two cases with significant bone loss requiring a graft with stabilization by tibial pilon plate.
Thus in this series, there were only two cases of mechanical pseudarthrosis treated with minimal osteosynthesis, as opposed to three cases of septic pseudarthrosis treated with internal osteosynthesis. The rate of pseudarthrosis reported in the published series is variable. Bastias C, et al., 2014 did not note any pseudarthrosis when using internal osteosynthesis. On the other hand, Pugh KJ, et al., 1999 obtained a significantly higher number of pseudarthrosis in his patients treated with external fixators compared to those treated with internal osteosynthesis. Also, there were no cases of postoperative infection in the 26 patients treated with minimal osteosynthesis, compared with three cases of material infection treated with internal plate osteosynthesis. A study of a series of 36 patients with pilon fractures treated with combined internal and external fixation which revealed a rate of 8% of septic complications (Tornetta III P, et al., 1993; Salton HL, et al., 2007). Another series of 127 cases of tibial pilon fractures treated with external fixation with minimal fixation revealed a rate of 0%-4% of infectious complications (Kim HS, et al., 1997; Endres T, et al., 2004; Kapoor SK, et al., 2010; Bacon S, et al., 2008; Gaudinez RF, et al., 1996), and it still con- firms the advantage of the closed focus which always gives a lower rate of septic complication than the open focus.
From a functional standpoint, the best result was obtained with minimal osteosynthesis (mean AOFAS score 86.2) in our series, compared with other surgical techniques for the management of pilon fractures. These results are consistent with the results found in the literature. Encinas-Ullán CA, et al., 2013 found a mean AOFAS score of 84.9 points, Bastias C, et al., 2014 had a mean score of 89, and Kao KF, et al., 2000 also obtained a mean score of 87.3.
Conclusion
Overall, this study has allowed us to open our minds to other surgical techniques, in particularly minimal osteosynthesis for the management of tibial pilon fractures. Indeed, this technique deserves its place because it respects the soft tissues that are the site of suffering in almost all pilon fractures, and thus allows for one-step management without waiting for improvement in the skin condition. It is also the method of recovery in countries where there are no means to adopt an adequate therapeutic method.
The condition of the skin opposite the tibial pilon, whether open or in pain, is an imperative condition for the choice of therapeutic method, which gives considerable value and place to minimally invasive osteosynthesis, especially when it allows intraoperative good bone reduction and good reconstruction of the articular surface.
Author's Contributions
Adnane Lachkar, Hicham Yacoubi and Najib Abdeljaouad did the surgery. Samir Ben Salah, Ayman Benabdellah and Issa Ali Eyal Slman draft- ed the study protocol. Samir Ben Salah, and Ayman Benabdellah drafted the documents for the ethics vote. Samir Ben Salah designed the study, developed the questionnaire, treated the data, did the statistics, and then drafted the manuscript and figures. All authors read and approved the final manuscript.
Ethical Approval and Cosent to Participate
Ethical approval was not needed in view of the retrospective and observational type of our study based on the analysis of the medical data of the patients treated in our trauma department as well as their follow-up thanks to our computerized system of archiving of the medical files. For this reason, consent of all the patients included in the study to use their medical data for the purpose of scientific research is sufficient.
Cosent for Publication
A written consent signed by all patients was obtained authorizing the use of their medical data in the scientific research and for publication on open access.
Availability of Data and Materials
The collection of data necessary to accomplish this work is facilitated by our computerized system of archiving medical records and the evolution of patients and their final results. Due to the sensitivity of the raw data, all data are available from the first author on request.
References
- Plaweski S, Huboud-Peron A, Faure C, Merloz P. Fractures du pilon tibial. Encycl Méd Chir. 1999.
- Bastias C, Henríquez H, Pellegrini M, Rammelt S, Cuchacovich N, Lagos L, et al. Are locking plates better than non-locking plates for treating distal tibial fractures? Foot Ankle Surg. 2014; 20(2): 115-119.
[Crossref] [Google Scholar] [Pubmed]
- Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: A comparison of treatment methods. J Trauma. 1999; 47(5): 937.
[Crossref] [Google Scholar] [Pubmed]
- Tornetta III P, Weiner L, Bergman M, Watnik N, Steuer J, Kelley M, et al. Pilon fractures: Treatment with combined internal and external fixation. J Orthop Trauma. 1993; 7(6): 489-496.
[Crossref] [Google Scholar] [Pubmed]
- Salton HL, Rush S, Schuberth J. Tibial plafond fractures: Limited incision reduction with percutaneous fixation. J Foot Ankle Surg. 2007; 46(4): 261-269.
[Crossref] [Google Scholar] [Pubmed]
- Kim HS, Jahng JS, Kim SS, Chun CH, Han HJ. Treatment of tibial pilon fractures using ring fixators and arthroscopy. Clin Orthop Relat Res. 1997; 334: 244-250.
[Google Scholar] [Pubmed]
- Endres T, Grass R, Biewener A, Barthel S, Zwipp H. Advantages of minimally-invasive reposition, retention, and Ilizarov-(hybrid) fixation for pilon-tibial-fractures fractures with particular emphasis on C2/C3 fractures. Unfallchirurg. 2004; 107(4): 273-284.
[Crossref] [Google Scholar] [Pubmed]
- Kapoor SK, Kataria H, Patra SR, Boruah T. Capsuloligamentotaxis and definitive fixation by an ankle-spanning Ilizarov fixator in high-energy pilon fractures. J Bone Joint Surg Br. 2010; 92(8): 1100-1106.
[Crossref] [Google Scholar] [Pubmed]
- Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, et al. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: Open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008; 39(2): 196-202.
[Crossref] [Google Scholar] [Pubmed]
- Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation in tibial plafond fractures. Clin Orthop Relat Res. 1996; 329: 223-232.
[Crossref] [Google Scholar] [Pubmed]
- Encinas-Ullán CA, Fernandez-Fernandez R, Rubio-Suárez JC, Gil-Garay E. Medial versus lateral plating in distal tibial fractures: A prospective study of 40 fractures. Rev Esp Cir Ortop Traumatol. 2013; 57(2): 117-122.
[Crossref] [Google Scholar] [Pubmed]
- Kao KF, Huang PJ, Chen YW, Cheng YM, Lin SY, Ko SH. Postero-medio-anterior approach of the ankle for the pilon fracture. Injury. 2000; 31(2): 71-74.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Samir Ben Salah1,2*, Ayman Benabdellah1,2, Issa Ali Eyal Slman1,2, Adnane Lachkar1,2, Hicham Yacoubi1,2 and Najib Abdeljaouad1,22Orthopedic Trauma Department, Mohammed Ist University, Oujda, Morocco
Received: 27-Apr-2023 Accepted: 22-May-2023 Published: 29-May-2023, DOI: 10.31858/0975-8453.14.5.343-348
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






