Case Study - (2024) Volume 15, Issue 7
Abstract
Marshall syndrome or PFAPA syndrome, is a rare autoimmune disorder that is mainly found in preschool- aged children. However, medical observations show that a similar clinical picture can develop in adults, more often at the age of 20-50 years. The authors report the case series of adult patients admitted to the clinic of Ear, Throat and Nose (ENT) diseases of the PMGMU named after IM Sechenov. The particular significance of this study lies in the increasing the awareness of otolaryngologists and therapists about the Marshall’s syndrome to improve the quality of its diagnosis and treatment. There are only isolated clinical cases of adult patients with Marshall syndrome in the literature. However, despite the rare occurrence of this pathology and the difficulties in diagnosis, it is necessary to increase awareness among both healthcare professionals and patients about this clinical syndrome in order to improve the quality of its diagnosis and treatment.
Keywords
Marshall syndrome, PFAPA syndrome, Periodic fever, Autoimmune disorder, Tonsillectomy
Introduction
Marshall’s syndrome or PFAPA syndrome (Periodic Fever, Aphthous stomatitis, Pharingitis, cervical Adenitis) was first described in 1987 by GS Marshall and his colleagues (Marshall GS,et al.,, 1987). In this observation, 12 clinical cases of a previously unknown periodic fever syndrome in children were described. Subsequently, this pathology was detailed by HM Feder and was named FAPA syndrome (Fever, Aphthous stomatitis, Pharyngitis, cervical Adenitis), and later the term was changed to PFAPA-with the addition of the letter P (Periodic), indicating the periodic nature of the disease (Feder HM, 1989; Marshall GS, 1989).
Prevalence of Marshall’s syndrome in the pediatric population is currently estimated at 2-3 children per 10,000 (Maidannik VG, 2013). There is very little information on the prevalence of this syndrome in the adult population, with only isolated clinical observations and small patient groups found in the literature (Rigante D,et al.,, 2017). For example, Padeh SMD,et al.,, 2008, described a group of 15 adults with clinical manifestations of the syndrome. The average age of the patients was 20.9 years, with episodes recurring every 4-6 weeks, and complete resolution of symptoms between clinical manifestations. This data shows that Marshall’s syndrome is a current issue not only in pediatrics.
Fever in children with PFAPA syndrome typically presents between the age of 2-5 years old (more commonly around three and a half years old), although it can occur earlier. Episodes of the syndrome (attacks) in most patients last for 5-7 years and spontaneously resolve by the age of ten, in some cases in the teenage years (Maidannik VG, 2013). A complete set of PFAPA syndrome symptoms is observed in less than half of cases. The most commonly occurring manifestations (70%-90%) are pharyngitis or tonsillitis and cervical lymphadenitis. Following the fever episode, there is а rapid regression of lymphadenopathy (Babachenko IV,et al.,, 2020). A distinctive feature of Marshall’s syndrome is the clear cyclical nature of the attacks, with intervals between them ranging from 2-7 weeks and potentially lengthening over time. Spontaneous resolution of the febrile state typically occurs within 3-6 days from the onset of fever (Batu ED, 2019).
Literature indicates that the duration of fever episodes is significantly longer in adult patients compared to the pediatric population, which in some clinical cases may complicate diagnosis (Rigante D,et al.,, 2017; Sicignano LL,et al.,, 2021). There are also reports of joint symptoms, myalgia, headache, and fatigue being more commonly observed in adults (Rigante D,et al.,, 2017).
Marshall syndrome is currently considered as a heterogeneous hereditary disease, but a specific causal mutant gene has not been identified. However, genetic predisposition loci to PFAPA syndrome have been identified, suggesting an association with Behcet’s disease and recurrent aphthous ulcers (Manthiram K, 2023). This complicates genetic diagnostics and distinguishes the described pathology from known diseases associated with mutations in specific loci, such as MEFV in familial Mediterranean fever or Nucleotide-binding domain, Leucine-Rich-containing family, Pyrin domain-containing-3 (NLRP3) in Cryopyrin Associated Periodic Syndrome (CAPS) (Maidannik VG, 2013).
The main link in the pathogenesis of PFAPA syndrome is hyperactivation of innate (antigen-independent) immunity and hyper production of acute-phase proteins such as, C-Reactive Protein (CRP) (Purrahman D,et al.,, 2022).
The main mediator of inflammation is Interleukin-1 (IL-1) which is produced without direct involvement of microbes or viruses in protein complexes formed in neutrophils and macrophages-inflammasomes (Babachenko IV, 2020). Patients with this background show a characteristic picture of blood during acute inflammation, leukocytosis, neutrophilia, and high Erythrocyte Sedimentation Rate (ESR).
In 2008, diagnostic inclusion criteria for PFAPA in adults were proposed to be as follows (Cantarini L,et al.,, 2017)-
• Onset of the disease at age 16 and older.
• Recurrent fever accompanied by erythematous pharyngitis and/or cervical lymphadenitis.
• Elevated markers of inflammation during episodes.
• Intervals between disease flares without any symptoms.
Exclusion criteria included infections, autoimmune and neoplastic diseases, monogenic and feverish polygenic autoinflammatory diseases. A throat swab during fever should not show signs of infection, and antibacterial therapy in such patients is ineffective.
The goal of treatment is to alleviate symptoms and increase the intervals between periods of exacerbation of Marshall syndrome;for this purpose, the following are used: Glucocorticosteroids (prednisolone at a dose of 50-60 mg/day) according to research data were prescribed to 33 patients out of 36, average age 33.3 ± 9.5 years, while a complete response to therapy was noted in 28 patients, a partial response in 4, and in one clinical case there was no effect of treatment (Cantarini L,et al.,, 2012).
In cases of glucocorticoid resistance, tonsillectomy or adenotonsillectomy may be performed, which in most cases helps prevent new attacks (Amarilyo G,et al.,, 2020).
It is noted that the effect of tonsillectomy may be temporary, and episodes of fever may occur several years after tonsillectomy and a period of absence of Marshall syndrome manifestations (Cantarini L,et al.,, 2012; Colotto M,et al.,, 2011; Rydenman K,et al.,, 2023). Temporary, but sufficiently long- term well-being after surgical treatment may be associated with the removal of lymphoid tissue, the activity of which is the cause of immune dysregulation in PFAPA syndrome (Rydenman K,et al.,, 2023). The recurrence of fever episodes may occur due to compensatory hypertrophy of other lymphoid structures in the throat (Cantarini L,et al.,, 2012).
In cases of persistent febrile attacks, the use of an IL-1 antagonist (the main mediator of inflammation)-Anakinra (Kineret), may be considered (Maidannik VG, 2013). We present a series of clinical cases of patients with Marshall syndrome.
Case Presentation
Clinical case 1
Patient A, who was 29 years old male, visited the Ear, Nose and Throat (ENT) clinic of Sechenov University with complaints of severe sore throat, increased body temperature to 39.3°C, and pain in the submandibular lymph nodes. Upon examination, general condition was found to be satisfactory with Body Mass Index (BMI) of 25.4 kg/m2 and body temperature 39°C. From anamnesis, it was found that he has been ill for 2 days, uses gargling with a local antiseptic-chlorhexidine, started taking systemic antibiotic therapy with levofloxacin 500 mg once a day from the first day, as well as antipyretics. No significant improvement is noted during the treatment.
During mesopharyngoscopy, soft palate symmetric, uvula along the midline, stasis hyperemia and swelling of the palatal arches were noted, palatine tonsils grade 1, hyperemic, swollen, and covered with white-yellow plaque. Regional submandibular lymph nodes are palpable, moderately painful, soft-elastic consistency, up to 1.5 cm. Other ENT-organs are normal. Heart rate, respiratory rate, blood pressure normal (Figures 1A and 1B).
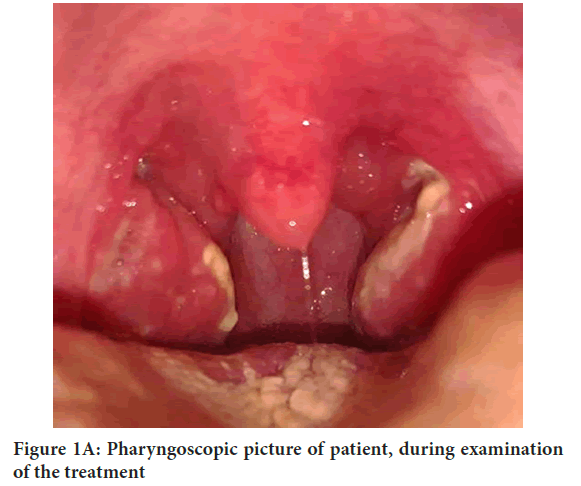
Figure 1A: Pharyngoscopic picture of patient, during examination of the treatment
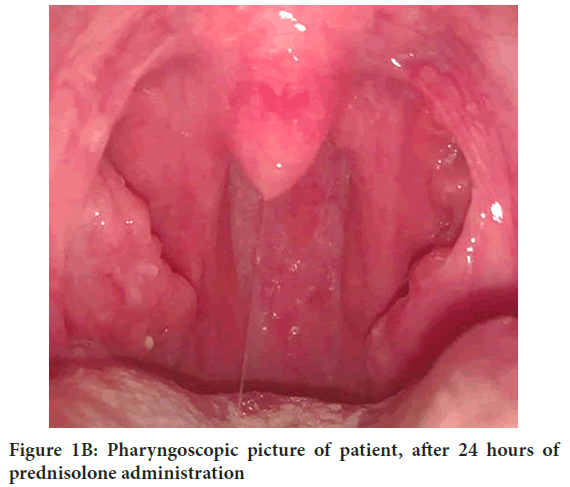
Figure 1B: Pharyngoscopic picture of patient, after 24 hours of prednisolone administration
The patient underwent a strep test, the result was negative. Complete blood count, absolute and relative neutrophilia (82%, reference values 48%-78%, 8.18 thous/mcl, reference values 1.78-5.38 thous/mcl), absolute and relative lymphocytopenia (8%, reference values 48%-78%, 0.8. thous/mcl, reference values 1.32-3.57 thous/mcl), increase in band neutrophils (27% reference values 1%-6%), other parameters of the complete blood count within normal limits. ESR by Westergren 6 mm/hr, elevated C-reactive protein 30.8 mg/l (reference values<5.0). Bacteriological examination of the surface of the palatine tonsils, result after 7 days-Streptococcus constellatus 104 CFU/smear (conditionally pathogenic microflora).
According to the patient, a similar condition with fever above 38.5°C, tonsil plaques, and throat pain has recurred 5 times over the past 4 months, once a month. Upon examination by an ENT specialist and therapist at the place of residence, a diagnosis of bacterial tonsillopharyngitis was established, for which repeated courses of systemic antibiotic therapy were carried out where amoxicillin/clavulanic acid, cefuroxime, azithromycin, levofloxacin and lincosamides was administered for 7-10 days. While taking antibiotics, there was no significant relief; the patient symptomatically used Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) to relieve fever and topical anti-inflammatory and antiseptic agents. Biochemical blood analysis showed an increase in CRP. This condition lasted for 4-7 days. There was no abdominal pain, chest pain, joint pain, appetite and stools were normal. Between episodes of illness, the patient feels well he was noted to have several episodes of stomatitis not related to angina. A similar series of “tonsillitis” was observed 3 years ago. The patient denies chronic illnesses, and there is no family history of periodic syndromes.
Considering the clinical picture of an acute illness with a focus of inflammation on the palatine tonsils, regional lymphadenitis, high fever, as well as the cyclical nature of exacerbations and the lack of a radical effect from systemic antibacterial therapy, we diagnosed the patient with Marshall syndrome. The patient was prescribed prednisolone 60 mg (12 tablets), omeprazole 40 mg once with a pronounced positive effect. Within 12 hours, the body temperature dropped to 36.7°C, throat pain significantly decreased, and complete normalization of the condition was observed within 24 hours. Subsequently, two more episodes were noted, occurring at intervals of 4 and 6 weeks, which were also successfully treated with a single dose of 60 mg prednisolone. Currently, there have been no episodes for 2 years.
Clinical case 2
Patient B, 25 years old, presented to the ear, nose, and throat clinic with complaints of frequent tonsillitis since the age of 16, occurring every month, accompanied by a high fever of 39°C-40°C and lasting 5-8 days.
Anamnesis of life denoted that he grew and developed normally, denies concomitant diseases, and has no history of allergies. According to the patient’s history, his father suffered from chronic tonsillitis since childhood; his tonsils were removed at the age of 14, with “insufficient effect.” The patient was unable to explain what the insufficient effect was. History of the disease, denoted that from the first episode of the symptoms described above, the patient was observed by therapists and otolaryngologists in various medical institutions, blood tests (complete blood count, CRP, Antistreptolysin O antibody (ASLO)) have been performed multiple times, strep tests were always negative, repeated throat swab culture tests did not reveal any pathogens or high levels of opportunistic bacteria. During acute episodes, there was a slight increase in CRP and accelerated ESR, sometimes leukocytosis (11 × 109/l, reference values 4-9 × 109/l), neutrophilia (89%, reference values 48%-78%) with a left shift. All other blood parameters were within normal limits. Each situation was considered as tonsillitis (acute streptococcal tonsillopharyngitis), and the patient almost monthly took systemic antibacterial drugs (multiple courses of penicillin’s, third-generation cephalosporins, macrolides, fluoroquinolones) for an average of 5 days, local antiseptics, bacteriophages-without significant improvement. Between episodes of illness, the patient felt healthy, and laboratory parameters also returned to normal.
One year ago (in June 2021), the patient underwent bilateral tonsillectomy, after which the described episodes of illness did not recur for six months. Recurrences occurring seven months later were considered by medical professionals as lingual tonsillitis, for which appropriate treatment was administered each time (local antiseptics, bacteriophages, systemic antibacterial therapy). The patient presented to the clinic after another episode of “tonsillitis”.
On examination, the general condition is satisfactory, BMI 25 kg/m2 and body temperature 36°C. During mesopharyngoscopy and fiberoscopy showed symmetrical soft palate, scarred tonsillar fossae but clean and absence of uvula (removed during a previous operation) (Figures 2 and 3).
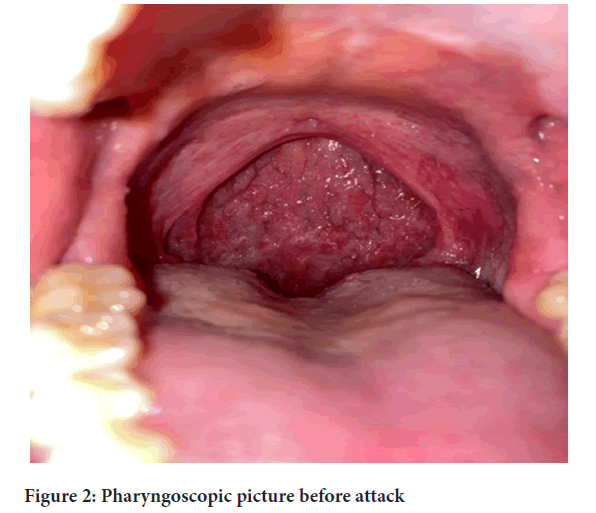
Figure 2: Pharyngoscopic picture before attack
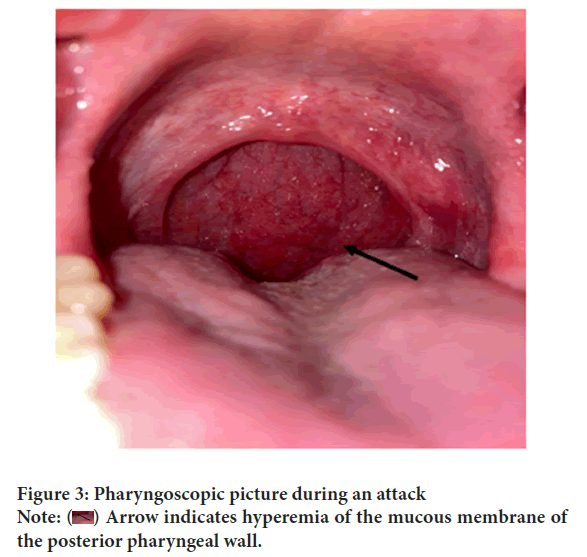
Figure 3: Pharyngoscopic picture during an attack
Note: ( ) Arrow indicates hyperemia of the mucous membrane of
the posterior pharyngeal wall.
) Arrow indicates hyperemia of the mucous membrane of
the posterior pharyngeal wall.
The mucous membrane of the posterior pharyngeal wall is pink and moist, tongue is not coated. Slight hyperplasia of the lymphoid tissue granules of the posterior pharyngeal wall, lingual tonsil is unchanged. Regional lymph nodes are slightly enlarged with painless palpation without adhering to the skin. Other ENT organs are unremarkable.
Among the comorbidities, Gastroesophageal Reflux Disease (GERD) was diagnosed by the gastroenterologist. Symptomatically receiving omeprazole 20 mg. Considering the characteristic periodicity of the disease, ineffectiveness of antibacterial therapy, elevation of inflammatory markers only during attacks, absence of any symptoms in the interictal period, negative throat cultures, temporary effect of tonsillectomy, Marshall syndrome was suspected by us. The patient was observed for 2 weeks, after the next episode of the disease developed, prednisolone 50 mg (10 tablets) was prescribed orally once at the peak of fever. The prescribed treatment relieved the attack within a few hours. Subsequently, the patient was referred to a rheumatologist for observation. It was recommended to exclude monogenic autoinflammatory diseases Familial Mediterranean Fever-Hyperimmunoglobulin D Syndrome-Twin Reversed Arterial Perfusion Syndrome (FMF-HIDS-TRAPS), perform a molecular genetic study to identify mutations in the Tumor Necrosis Factor Receptor Associated Periodic Syndrome 1A (TNFRSF1A), Mevalonate Kinase (MVK) and NLRP3 genes, continue treatment of attacks with glucocorticosteroids. No mutations in these genes were found in the test results. More than a year has passed since the diagnosis was established (confirmed by a rheumatologist as Marshall syndrome). Immediately after starting therapy, the attacks increased in frequency (every 3 weeks, but are relieved after taking the medication for a day), currently becoming less frequent after adjusting the prednisolone dose (60 mg orally) and relieved after taking the corticosteroids for a day and we continued to monitor the patient.
Results and Discussion
Inflammatory processes in the structures of Waldeyer’s tonsillar ring are a common problem in both pediatric and adult ENT practice. Acute streptococcal pharyngitis presents with a characteristic clinical picture-pronounced intoxication, fever, significant throat pain, and lymphadenopathy. Acute bacterial tonsillopharyngitis requires mandatory systemic antibiotic therapy. However, in cases of frequently recurrent tonsillopharyngitis and in adult patients, differential diagnosis with rare autoimmune diseases is necessary for the adequate treatment of such patients. The pathogenesis of Marshall’s syndrome is still unknown.
However, the effectiveness of corticosteroids suggests that the cellular reactions related to this condition are non-infectious in nature. Inflammation arises from the activation of the innate immune system, but patients with PFAPA also have dysfunction of T-cells, and both adults and children with this condition have an immature immune system (Rigante D,et al.,, 2017). The initial effectiveness of tonsillectomy may be due to the removal of active lymphatic tissue (for example, palatine tonsils) responsible for immune dysregulation. However, secondary deficiency may occur due to compensatory hypertrophy affecting other tonsils of the tonsillar ring (e.g., lingual tonsils in our case). Indeed, such foci can serve as reservoirs for infections and aberrant cytokine regulation, leading to clinical recurrence of the disease. In literature, there is very little information about the description of this syndrome in adults, and even rare articles about Marshall syndrome in adult patients are written by pediatricians (Padeh SMD,et al.,, 2008). It is essential to increase the awareness of otolaryngologists and therapists about the diagnostic criteria of this disease.
Conclusion
Marshall syndrome (PFAPA syndrome) is the most common hereditary periodic fever syndrome in pediatrics and is also found in the adult population. This clinical case describes the manifestations and diagnostic criteria of Marshall syndrome in an adult patient. Despite the rarity of this pathology and the difficulty in diagnosis, it is necessary to increase awareness among both healthcare providers and patients about this clinical syndrome to improve the quality of its diagnosis and treatment.
Author Contributions
Karapetyan LS developed the concept, design, key goals and tasks and was also involved in the preparation and editing of the text. Grigoryan IZ prepared the text, analysed and interpreted the data. Starostina SV and Svistushkin VM approved the final version of the article. Svistushkin MV, Sinkov EV, Sobolev VP and Shadyev TK prepared and presented the illustrations of the study.
Consent for Publication
Informed consent for publication of data was obtained from the patients.
References
- Marshall GS, Edwards KM, Butler J, Lawton AR. Syndrome of periodic fever, pharyngitis and aphthous stomatitis. J Pediatr. 1987; 110(1): 43-46.
[Crossref] [Google Scholar] [Pubmed]
- Feder HM. Periodic fever associated with aphthous stomatitis, pharyngitis and cervical adenitis. Pediart Infect Dis J. 1989; 8: 1867. [Google Scholar]
[Pubmed ]
- Marshall GS. PFAPA syndrome. Pediatr Infect Dis J. 1989; 8: 658-659.
[Crossref] [Google Scholar] [Pubmed]
- Maidannik VG. Modern aspects of periodic fever with aphthous stomatitis, pharyngitis and cervical adenitis (Marshall’s syndrome) in children. INJPediatrObstet Gynecol. 2013; 3(3): 63-66.
- Rigante D , Vitale A, Natale MF, Lopalco G, Andreozzi L, Frediani B, et al. A comprehensive comparison between pediatric and adult patients with Periodic Fever, Aphthous stomatitis, Pharyngitis, and cervical Adenopathy (PFAPA) syndrome.Clin Rheumatol. 2017; 36(2): 463-468.
[Crossref] [Google Scholar] [Pubmed]
- Padeh SMD, Stoffman N, Berkun Y. Periodic Fever accompanied by Aphthous stomatitis, Pharyngitis and cervical Adenitis syndrome (PFAPA syndrome) in adults. Isr Med Assoc J. 2008; 10: 358-360.
[Google Scholar] [Pubmed]
- Babachenko IV , Tian NS, Ivanova MA, Sharipova EV, Belikova TL. Marshall’s syndrome in the practice of infection disease doctor and pediatrician (сlinical case). J Infectology. 2020;12(4):114-9
- Batu ED. Periodic Fever, Aphthous stomatitis, Pharyngitis, and cervical Adenitis (PFAPA) syndrome: Main features and an algorithm for clinical practice. Rheumatol Int. 2019; 39(6): 957-970.
[Crossref] [Google Scholar] [Pubmed]
- Sicignano LL, Rigante D, Moccaldi B, Massaro MG, DelliNoci S, Patisso I, et al. Children and adults with PFAPA syndrome: Similarities and divergences in a real-life clinical setting. Adv Ther. 2021; 38(2): 1078-1093.
[Crossref] [Google Scholar] [Pubmed]
- Manthiram K. What is PFAPA syndrome? Genetic clues about the pathogenesis. Curr Opin Rheumatol. 2023; 35(6): 423-428.
[Crossref] [Google Scholar] [Pubmed]
- Purrahman D, Poniatowski ŁA, Wojdasiewicz P, Fathi MR, Yousefi H, Lak E, et al. The role of inflammatory mediators in the pathogenesis of Periodic Fever, Aphthous stomatitis, Pharyngitis and cervical Adenitis (PFAPA) syndrome. Mol Biol Rep. 2022; 49(8): 8061-8069.
[Crossref] [Google Scholar] [Pubmed]
- Cantarini L, Vitale A, Sicignano LL, Emmi G, Verrecchia E, Patisso I,et al. Diagnostic criteria for adult-onset Periodic Fever, Aphthous stomatitis, Pharyngitis, and cervical Adenitis (PFAPA) syndrome. Front Immunol. 2017; 8: 1018.
[Crossref] [Google Scholar] [Pubmed]
- Cantarini L, Vitale A, Bartolomei B, Galeazzi M, Rigante D. Diagnosis of PFAPA syndrome applied to a cohort of 17 adults with unexplained recurrent fevers. Clin Exp Rheumatol. 2012; 30(2): 269-271.
[Google Scholar] [Pubmed]
- Amarilyo G, Rothman D, Manthiram K, Edwards KM, Li SC, Marshall GS, et al. Consensus treatment plans for Periodic Fever, Aphthous stomatitis, Pharyngitis and Adenitis syndrome (PFAPA): A framework to evaluate treatment responses from the Childhood Arthritis and Rheumatology Research Alliance (CARRA) PFAPA work group. PediatrRheumatol Online J. 2020;18(1):1-7.
[Crossref] [Google Scholar] [Pubmed]
- Colotto M, Maranghi M, Durante C, Rossetti M, Renzi A, Anatra MG, et al. PFAPA syndrome in a young adult with a history of tonsillectomy. Intern Med. 2011; 50(3): 223-225.
[Crossref] [Google Scholar] [Pubmed]
- Rydenman K, Sparud-Lundin C, Karlsson-Bengtsson A, Berg S, Fasth A, Wekell P. Tonsillectomy reduces the family impact of Periodic Fever, Aphthous stomatitis, Pharyngitis and cervical Adenitis (PFAPA) syndrome and improves health-related quality of life in affected children. Orphanet J Rare Dis. 2023; 18(1): 153.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Karapetyan LS*, Svistushkin VM, Starostina SV, Svistushkin MV, Grigoryan IZ, Sinkov EV, Sobolev VP and Shadyev TKCitation: Karapetyan LS: Marshall Syndrome in Adults, Myth or Reality
Received: 03-Jul-2024 Accepted: 17-Jul-2024 Published: 24-Jul-2024, DOI: 10.31858/0975-8453.15.7.221-224
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






