Research Article - (2023) Volume 14, Issue 2
Abstract
Introduction: We aimed to explore the medium-long term impacts of anti-retroviral treatment of hypertension in a sample of HIV-positive in Malawi. This was a retrospective study carried out at Disease Relief with Excellent and Advanced Means (DREAM) health Centre in Blantyre/Malawi on enrolled and followed up patients from 2005 to 2019.
Methodology: Information about age, gender, blood pressure, ART regimen, BMI, CD4 count, viral load, biochemistry, hemoglobin, marital status, education, survival and period on anti-retroviral drugs were retrieved from data base from 01/01/2006 to 31/12/2015. In total, we enrolled (alive and on HAART) 1350 patients >18 years (Mean age: 43.4 and the SD was ± 10.7 with 1031 (65.9%) females and 534 (34.1%) males who were taking (or have taken) ARVs for more than 6 months at the date of enrolment. Patients were not affected by hypertension or potentially related diseases like renal failure at the beginning of ART. The mean observation time from the HAART initiation was 77 months per person (SD ± 40).
Results: The sample was made up by two groups of patients, 675 who developed hypertension and 675 who did not, with similar age and gender composition. Among patients with hypertension, 30/675 (4.4%) developed severe hypertension, 154 developed moderate hypertension (22.8%) and 491 developed mild hypertension (72.8%). Hypertension stages were not associated to statistic significant differences of age and/or gender (p=0.422, p=0.281 respectively). At baseline, patients who developed hypertension showed higher hemoglobin, higher CD4 count and lower VL (p<0.001). Patients on AZT-based regimen and TDF-based regimen were at high risk to develop hypertension while PI-based regimen was protective to hypertension (p<0.001). In a multivariate analysis, factors independently associated to hypertension were higher CD4 count and body mass index at the visit date, while baseline viral load and PI-Including regimes were protective factors. Education level was inversely associated with risk of hypertension, while being married was associated of risk of hypertension (p<0.001). Mortality rate among hypertensive patients was 1.6% for those treated for hypertension against the 3.6% for those not treated.
Conclusion: This study shows a protective action of PI-including regimens compared with AZT based regimen that is associated to an increased risk of hypertension. Factors related to a better general health status are associated to a higher risk of hypertension as well as lower education, older age and male gender. Treatment should be started as soon as hypertension stages 2-3 are reached and controlled by behavioral factors is no longer effective.
Keywords
ART regimen, Hypertension, Antiretroviral therapy, Blood pressure
Abbreviations
ABC: Abacavir; ACS: Acute Coronary Syndrome; AMID: Acute Myocardite Infarction; ART: Anti-Retroviral Therapy; ARV: Antiretroviral; AZT: Zudovudine; AZV: Atazanavir; BMI: Body Mass Index; BP: Blood Pressure; CVD: Cardiovascular Disease; DAD: Data Collection for Adverse Events for Anti-HIV Drugs; DBP: Diastolic Blood Pressure; D4T: Stavudine; DREAM: Disease Relief with Excellent and Advanced Means; HAART: Highly Active Antiretroviral Therapy; HB: Hemoglobin; HIV: Human Immunodeficiency Virus; F: Female; LPV/r: Lopinavir/ritonavir; M: Male; NCD: Non Communicable Disease; NRTI: Nucleoside Reverse Transcriptase; NNRTI: Non-Nucleoside Reverse Transcriptase; PLWH: People Living with HIV; RAAS: Renin-Angiotensin-Aldosterone System; SBP: Systolic Blood Pressure; SSA: Sub-Saharan Africa; 3TC: Lamivudine; TDF: Tenofovir; VL: Viral Load; WHO: World Health Organization
Introduction
It is estimated that 37 million people are living with the HIV. From year 2000, HIV positive clients who have access to Highly Active Antiretroviral Therapy (HAART) has been increased from 700,000 to over 16 million (WHO, 2017; WHO, 2015). The use of Antiretroviral Therapy (ART) has decreased mortality related to Human Immunodeficiency Virus (HIV) from around 2 million deaths in 2005 to 1 million in 2016 (WHO, 2017; WHO, 2015). Despite the decrease of mortality related to HIV, the mortality related to cardiovascular disease has been doubled in people living with HIV (Feinstein MJ, et al., 2016). In fact, together with the prolonged lives of people living with HIV on HAART, also emerged some concerns-among the others lifestyle changes, aging and the toxic effects of ART, risk factors for Cardiovascular Disease (CVD) (Triant VA, et al., 2007). It is estimated that people living with HIV (PLWH) on ART have a 10-year risk of developing CVD higher than 20% of people who are HIV positive but not yet on ART (Mutimura E, et al., 2008).
The main risk factor for mortality worldwide is hypertension and it is a growing concern in adults with HIV-infection (Gazzaruso C, et al., 2003). Africa was found to have highest prevalence of hypertension among the World Health Organization (WHO) region (46% for both genders). The African Americans and the black Africans has got higher risk of developing hypertension than other population, probably due to lack of awareness, early treatment and prevention methods of hypertension. However, higher hypertension incidence rates for blacks compared to white people have been mentioned in many studies. Bogalusa HEART study showed that black people had higher hypertension risk compare to white after 15 years of follow up (Kaul S, et al., 1991). In 2030, the expected deaths caused by CVD will double to 2.4 million in 2030 relative to an estimated reports from 2000 (WHO, 2013). In SSA, mortality due to CVD is estimated to be three times greater than in Western Europe (WHO, 2009).
An interesting meta-analysis published by Okechukwu S Ogah and colleagues, in recent advances in hypertension in sub-Saharan Africa took into consideration 38 publications from Sub-Saharan Africa (SSA) partly carried out in urban areas and partly in rural ones (Table 1). This paper reports a prevalence of hypertension among the general population at 44.9% in Malawi, which has been also confirmed by WHO, that report for Malawi a prevalence of hypertension of 43.4%.
| No | Country | Population 2010 | Men | Women | All |
|---|---|---|---|---|---|
| 1 | Niger | 15,111,953 | 52.5 | 42.8 | 47.8 |
| 3 | Ivory coast | 19,737,800 | 44.1 | 38.6 | 41.5 |
| 4 | Mozambique | 23,390,765 | 46.7 | 43.3 | 44.4 |
| 7 | Malawi | 14,900,841 | 45.6 | 41.4 | 43.4 |
| 9 | Zambia | 13,088,570 | 41.3 | 39 | 40.1 |
Table 1: Prevalence of hypertension in some selected African countries
The link between HIV infection and cardiovascular diseases
Adults with HIV and hypertension have a higher cardio vascular risk events and mortality compare to non HIV infected adults with hypertension. In a prospective cohort study of >80,000 people living with HIV and uninfected American veterans were followed for 6 years on average and this study found that the risk of acute myocardial infarction was a 2 fold in people living with HIV and hypertension when compared to hypertensive adults without HIV infection (WHO, 2017; WHO, 2015).
Cardiac abnormalities in HIV-positive persons were noted as early as 1989 (Himelman RB, et al., 1989; Hecht SR, et al., 1989) (pre-HAART era) and included dilated cardiomyopathy, endo-, myo-and peri-carditis, and pulmonary hypertension (Himelman RB, et al., 1989; Hecht SR, et al., 1989; Rerkpattanapipat P, et al., 2000).
One of the largest studies on Hypertension done in the world showed that patients infected with HIV had a higher prevalence of hypertension compare to closely HIV negative controls group, as reported by Dutch investigators in clinical infectious diseases. They noted that hypertension in HIV patients was also associated with abdominal obesity, body shape change related to stavudine which is an older HIV drugs no longer used in many countries (Medina-Torne S, et al., 2012).
However, Feinstein MJ, et al., 2016 found no difference in hypertension prevalence between those HIV infected and those HIV negative (32% vs. 29%, p=0.47).
Mechanisms underlie higher hypertension prevalence are not fully understood even if some indication have been given by several researchers. Dysangco A, et al., 2017 did not observed endothelial function abnormalities in HIV positive (+) patients receiving ARVs even if they showed an increase of inflammation and endothelial activation. HIV seems to be able to activate inflammation mechanisms associated to thrombotic and artherosclerotic disease (Becker AC, et al., 2010; Knudsen A, et al., 2013; Lo J, et al., 2010). This action is counteracted by ARVs, even if evidences exist that ARVs drugs, especially PI, are associated to an increase of Acute Miocardial Infarction (Friis-Møller N, et al., 2003; DAD study group, 2007; Cachay ER, 2023). Rasoulinejad and coll identified pulmonary Hypertension independently associated to HIV infection. Moreover, HIV infection can induce renal insufficiency which can cause a secondary hypertension (Bloomfield GS, et al., 2011; Mateen FJ, et al., 2013; Mutede BR, et al., 2015).
The relation between hypertension and ART
Both Human Immunodeficiency Virus (HIV) infection and Hypertension are long term health conditions and sometimes last without any symptoms at the beginning but all these conditions are manageable at the earlier stage (Hall AM, et al., 2011). As long as people living with HIV have a greater life expectancy on HAART, many HIV infected individuals will gain weight which is also a hypertension risk factor (Hall AM, et al., 2011). At the same time, weight gain can also be an ART side effect, due to some ARVs like PIs, efavirenz and tenofovir (Mateen FJ, et al., 2013).
Renal tubular toxicity have been found to be caused by tenofovir use in patients infected with HIV and this risk can be increased when there is already a pre-existing renal disease (Mutede BR, et al., 2015; Hall AM, et al., 2011; Mpondo BC, et al., 2014; Msango L, et al., 2011; Dolan SE, et al., 2005).
Insulin resistance can be caused by ARVs and cause into lipodistrophy/ weight gain. The Nucleoside Reverse Transcriptase Inhibitors (NRTIs), potentially induce changes in mitochondrial ability which can modify the sensitivity of insulin (Mutimura E, et al., 2008). Many changes of insulin sensitivity have been found in clinical trials on the use of PIs in people living with HIV (WHO, 2013).
PIs have been associated to increased cardiovascular risk, due to impaired glucose metabolism, dyslipdemia, obesity and hypertension in industrialized countries (Kearney PM, et al., 2005).
Hypertension and people living with HIV in Malawi
In Malawi, it is noticed an increased hypertension cases and most of the people living with HIV have also hypertension while many of them are not aware of their hypertension status, therefore are not treated (Matchaya GC, 2007; Msyamboza KP, et al., 2011).
The Malawi HTN prevalence varies from one group to another, in 2009, according to the WHO STEPS survey (by definition, STEP: State Tobacco Education Prevention).
According to the STEPS study, the hypertension prevalence was 35% among adults, which is lower than the result found by the WHO in 2011 which found 43.4% among adults; in a small HIV-infected cohort in Blantyre, it was found that 46% had high blood pressure (Amberbir A, et al., 2019) while a larger cohort found 24% of hypertensive patients (Ataklte F, et al., 2015). The contributing factors to this problem is lack of a strong hypertension program, non-screening national program for hypertension which lead to poor management of hypertensive patients in Malawi (WHO, 2012; Mitambo C, et al., 2017; Celermajer DS, 1997).
It is projected that hypertension will cause more deaths in African countries than infectious diseases in the next coming 20-30 years (WHO, 2012, Mitambo C, et al., 2017).
Materials and Methods
The study is made up by two different approaches both carried out at DREAM health Centre Blantyre/Malawi under the DREAM 2.0 program. The first part includes a case control study about the determinants of the onset of hypertension in patients receiving ART. Observation started from the censor date back to the HAART initiation (Initiation date). HAART initiation is taken from the DREAM software for the patients who started HAART at the DREAM program, while it has been taken by the health passport when the patients started HAART before coming to the DREAM center. Data have been recorded at the HAART initiation (or at the first contact with the DREAM program), at the change of ART regimen (Change date) in case the patient has been shifted to a second line regimen, and at the available visit closest to the censor date for the non-hypertensive patients or at the visit when the diagnosis of hypertension was done for hypertensive patients (Visit date). The ART regimen associated to the developing of hypertension was the one that was taken by the patients for at least 180 days before the diagnosis of hypertension.
Inclusion criteria
a) Patients older than 18 years
b) Patients who were not affected by hypertension or related disease at the time when they started Antiretrovirals (ARVs)
c) All patients who have been taking/have taken ARVs for more than 180 days
The study involved 1350 patients aged over 18 years (Mean age: 43.4 and the SD was ± 10.7 with 1031 (65.9%) females and 534 (34.1%) males who were matching inclusion criteria
The starting date for the retrospective analysis was the last visit before 07/06/2017 or when the hypertension diagnosis was done (visit date) (Tables 2 and 3).
| Gender | Frequency | % value |
|---|---|---|
| Female (F) | 1.031 | 65.9 |
| Male (M) | 534 | 34.1 |
| Total | 1.565 | 100 |
Table 2: Hypertension diagnosis according to gender
| Hypertension stages | Frequency | Percentage (%) |
|---|---|---|
| No hypertension | 675 | 50 |
| Stage 1-mild | 491 | 36.4 |
| Stage 2-moderate | 154 | 11.4 |
| Stage 3-severe | 30 | 2.2 |
| Total | 1350 | 100 |
Table 3: Stages of hypertension
The second part of the study was a retrospective observational cohort analysis carried out starting at the date of hypertension diagnosis and comparing survival of three groups of patients
a) Hypertensive patients treated for hypertension
b) Hypertensive patients not treated for hypertension
c) Non hypertensive patients
Hypertension was defined according the following criteria-
i. No hypertension was defined as normal blood pressure with Systolic Blood Pressure (SBP) lower than 140 mm Hg and Diastolic Blood Pressure (DBP) lower than 90 mm Hg.
ii. Stage 1-Mild hypertension was defined as 140<SBP ≤ 159 or 90 <DBP ≤ 99 mm Hg measured at least two times after resting not less than 15 minutes
iii. Stage 2-Moderate hypertension was defined as 160<SBP ≤ 179 or 100 <DBP ≤ 109 mm Hg
iv. Stage 3-Severe hypertension was defined as SBP ≥ 1780 and or DBP ≥ 110 mm Hg
Antiretroviral regimens
Use of PIs based regimen was defined as being prescribed any of the locally available PIs which include Lopinavir (LP), or Ritonavir (r) or Darunavir (DV) or Atazanavir (ATV) irrespective of the other two ARVs included in the administrated regimen.
Use of Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTI)-based regimen was defined as being prescribed of the locally available NNRTIs including Nevirapine (NVP) or Efavirenz (EFV). In this case the other ARV drugs included in the regimen have been specified and included separately in the analysis when it was reasonable.
Use of Nucloeside Reverse Transcriptase Inhibitors (NRTI)-based regimen was defined as being prescribed of the locally available NRTIs including Stavudine (d4T), Lamivudine (3TC), Abacavir (ABC), Tenofovir (TDF), Zidovudine (AZT) when they prescribed regimen did not include any other kind of ARVs.
BMI was defined and categorized according to standard international definitions-Body Mass Index (BMI) is a simple index of weight-for-height that is commonly used to classify underweight, overweight and obesity in adults. It is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). More than 25 kg was considered to be in category 1 and less than 25 was considered to be in category 0.
Hemoglobin was measured in gram per deciliter and categorized as 0=hemoglobin less than 10 g/dl and 1=hemoglobin over 10 g/dl.
Creatinine measurements in micromoles per liter were converted to milligrams per deciliter and dichotomized in two categories according to the threshold of 1.20.
Glomerular filtration rate was estimated using the abbreviated modified diet in renal disease equation formula of Cockcroft-Gault. Creatinine clearance (CrCl) (male)=((140-age) × weight in kg)/(serum creatinine × 72).
In the DREAM protocol blood samples were collected at Initiation date (before ART initiation) and the first viral load control and CD4 count at 6 months and then routine viral load control every year while. Routine biochemistry and FBC were controlled every 6 months (Table 4). Hemoglobin was measured in grams/deciliter and hemoglobin less than 10 g/dl was considered as group 0 (low hemoglobin) and HB more than 10 g/dl was considered as normal hemoglobin and was group 1.
| Hypertension | N | Mean | Standard deviation | Standard mean error | p-value | |
|---|---|---|---|---|---|---|
| Mean age | Non-hypertension | 675 | 43.2 | 10.97 | 0.42234 | p=0.281 |
| Hypertension | 675 | 42.57 | 10.3 | 0.39651 |
Table 4: Mean age according to hypertension
Viral Load (VL) was measured in copies/milliliter of blood with 40 copies/ ml as threshold.
CD4 count was measured in cell/ml of blood.
Descriptive analyses were performed to display the overall distribution of the cardiovascular, clinical and HIV-related risk factors for men and women. Continuous variables are displayed as mean and SD or as median and interquartile range. For our descriptive analyses, categorical variables are expressed as proportions. Categorical variables have been compared by the Pearson Chi-Square test, while continuous ones by t-test. Multivariate analysis has been performed to establish the inference of the different risk factors on the outcomes. All these analysis have been carried out using SPSS 25.0 statistical package. The analysis is designed to describe the relation between several risk factors for hypertension with the two end-points reported above.
Results
In total, we analyzed 1350 patients from January 2006 to December 2016, 675 of participants developed hypertension during this period and 675 did not representing 50% each group. The mean age was 43.2026 for the non-hypertensive patients and 42.5783 for hypertensive patient, p=0.281, the mean difference was not significant and the p-value shows that age is similar in the two groups (Table 5). Gender was equally distributed too, between the two samples. According to the baseline parameters, we noticed that the mean creatinine was high among non-hypertensive patients compare to hypertensive patients (0.99 vs. 0.74), also the mean HB was low among non-hypertensive patients compare to hypertensive patients (11.2 vs. 12.03) (Table 6).
| CD4 count at ART initiation | Death abandon | Total | p-value | |||
|---|---|---|---|---|---|---|
| No | With | |||||
| CD4 | <350 cells/ml | N | 657 | 233 | 890 | <0.001 |
| % in CD4 BL | 73.80% | 26.20% | 100.00% | |||
| >350 cells/ml | N | 407 | 49 | 456 | ||
| % in CD4 BL | 89.30% | 10.70% | 100.00% | |||
| Total | N | 1064 | 282 | 1346 | ||
| % in CD4 BL | 79.00% | 21.00% | 100.00% | |||
Table 5: Survival according to CD4 count at ART initiation
| Hypertension | CREAT BL | HEMO BL | BMI BL | VL BL | CD4 BL | |
|---|---|---|---|---|---|---|
| Non hypertension | Mean | 0.99 | 11.2 | 21.4392 | 97418.39 | 222.43 |
| N | 603 | 671 | 666 | 675 | 675 | |
| SD | 2.88 | 5.96 | 4.63046 | 141749.9 | 192.067 | |
| Hypertension | Mean | 0.7443 | 12 | 23.2317 | 19330.24 | 383.88 |
| N | 209 | 629 | 671 | 611 | 627 | |
| SD | 0.24251 | 2.07 | 4.46985 | 68813.34 | 220.688 | |
| Total | Mean | 0.9304 | 11.6 | 22.3388 | 60317.41 | 300.18 |
| N | 812 | 1300 | 1337 | 1286 | 1302 | |
| SD | 2.49045 | 4.53 | 4.63638 | 119619.4 | 221.491 | |
Note: CREAT BL: Creatinine baseline; HEMO BL: Hemoglobin baseline; BL: BMI baseline; VL BL: Viral load baseline; CD4 BL: CD4 count baseline
Table 6: Analysis of hypertension using baseline parameters
For the viral load, the mean was higher in non-hypertensive patients compare to hypertensive patients (97418 copies vs.19330), the mean of viral load for non-hypertensive patients was 5 times higher than hypertensive patients. For the CD4 count baseline, we noticed the mean for non-hypertensive patients was half of the mean for hypertensive patients (222.43 cells vs.418 cells) with total mean of 300 cells. Taking into consideration the BMI, again higher values correlate with the development of hypertension since non hypertensive patients had a mean of BMI=21.43, while the mean BMI for hypertensive patients was 23.15, meaning the hypertensive patients had about 1.8 point higher BMI compare to non-hypertensive patients.
From the table above, we noticed that the mean creatinine is very similar from hypertensive to non-hypertensive clients. (0.904 vs.0.899) this tells us that the health conditions of our clients have been improved by the ART treatment, high creatinine is related to kidney damage but ART treatment had improved the health conditions of these patients; this is why the mean create for hypertensive patients and non-hypertensive patients is very similar. We also found the mean hemoglobin is similar for non-hypertensive and hypertensive patients (12.36 vs.12.81) (Table 7).
| Hypertension | CREAT | HEMO | BMI | VL | CD4 | |
|---|---|---|---|---|---|---|
| Non hypertensive | Mean | 0.89 | 12.4 | 21.96 | 11856.77 | 436.3 |
| N | 473 | 672 | 661 | 675 | 675 | |
| SD | 0.33 | 2.09 | 4.52 | 59954.51 | 243.21 | |
| With hypertension | Mean | 0.9 | 12.8 | 23.68 | 3455.5 | 438.66 |
| N | 436 | 671 | 671 | 675 | 675 | |
| SD | 0.41 | 1.9 | 4.88 | 17857.86 | 204.61 | |
| Total | Mean | 0.9 | 12.6 | 22.83 | 7656.14 | 437.48 |
| N | 909 | 1343 | 1332 | 1350 | 1350 | |
| SD | 0.37 | 2.01 | 4.78 | 44417.69 | 224.66 | |
Note: CREAT: Creatinine; HEMO: Hemoglobin; BMI: Body Mass Index; VL: Viral Load
Table 7: Comparative analysis for development of hypertension
CD4 count: We found the follow up CD4 count mean was 436 cells for non-hypertensive patients vs. 438 cells/ml for hypertensive patients, this also shows that the follow up CD4 count is almost the same for non-hypertensive patients vs. hypertensive patients, the difference is very slim, while at the base line, the CD4 count for non-hypertensive patients was half of hypertensive patients, this is the good effect of the ART. After being on ART the immunologic conditions are improved.
Viral load follow up: We noticed also the reduction of the gap between non hypertensive and hypertensive, the difference is 8401. the mean VL follow up is 11856 copies/ml while the mean for the hypertensive patients is 3455 copies/ml. the difference at baseline between hypertension and non-hypertension was 78.088 copies/ml. This shows again the impact of the ART treatment. In our cohort, we found that 117/170 hypertensive patients had no education meaning did not go to school, representing 68.8% of the total number of patients who did not go to school. Being low educated was related to the presence of hypertension and statistically significant with p<0.001. Among the primary level patients, we noticed that 324/600 had no hypertension representing 54%, with p<0.001.
For secondary level patient, we also noticed that over half (51.7%) 0265/513 of them had non-hypertension with p<0.001 meaning that being at secondary level is not related to a risk of hypertension.
For the university level, we noticed that 40.3% had hypertension stage 1 (27/67). According to the marital status, in total we had 868/1350 (64.29%) married patients men and women followed by widow 231/1350 (17.11%); we found that among married patients the percentage of hypertensive ones was 54.5%, he highest reported across the whole marital categories (p<0.001). Being single, the hypertension rate was 33% (37/112), while for divorced or separated patients; the rate was closer for hypertension and non-hypertension (48.9% and 51.1% respectively, for those who were widow). The final results of the multivariable logistic regression are consistent in both cases. Education was inversely associated to risk of hypertension, with p=0.01, as well as gender (even if with marginally statistic significant value); age was not associated to risk of hypertension (p-value of 0.12). Viral load<1000 copies/ml, CD4 count>350 cells/ml, BMI>25 and HB>10 g/dl were strongly associated to the development of hypertension with p<0.001.
For type of regimen, when we consider PIs as reference point, we noticed that 3TC/TDF/EFV and ABC/3TC/NVP are not associated to a risk of hypertension, while regimens including NVP showed a very mild risk of hypertension compared with PI-based regimen; when comparing EFV based regimen and NVP regimen we noticed that regimen containing NVP has got an association to risk of hypertension than EFV based regimen. Years of HAART administration is also showed a protective effect on the risk of developing hypertension. The time on HAART was also associated to the development of hypertension (Tables 8 and 9).
| Multivariables | Significance | OR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Education | 0.01 | 0.77 | 0.634 | 0.944 |
| Age | 0.12 | 0.98 | 0.974 | 1.003 |
| Gender (Female vs. Male) | 0.04 | 0.71 | 0.513 | 0.992 |
| VL at HAART initiation (>1000 vs. <1000 c/ml) | <0.001 | 0.06 | 4.50% | 8.60% |
| CD4 at HAART initiation (>350 vs. <350 c/µL) | <0.001 | 2 | 1.448 | 2.763 |
| BMI at HAART initiation (>25 vs. >25) | <0.001 | 1.98 | 138.80% | 283.50% |
| Hb at HAART initiation (>10 vs. <10 gm/100 cc) | <0.001 | 2.02 | 1.444 | 2.838 |
| Regimen by months of administration until the visit date | ||||
| PI-based | 1 | |||
| TDF/3TC/EFV | 0.134 | 1.09 | 99.70% | 102.20% |
| d4T/3TC/NVP | 0.002 | 1.01 | 1.005 | 1.02 |
| AZT/3TC/NVP | 0.009 | 1.01 | 100.30% | 102.30% |
| ABC/3TC/NVP | 0.116 | 1.03 | 0.992 | 1.078 |
| TDF/3TC/NVP | 0.008 | 1.02 | 1.007 | 1.047 |
| Years of HAART administration | <0.001 | 1.1 | 1.04 | 1.17 |
Table 8: Multivariables logistic regression; dependent variable-hypertension (No and with)
| Characteristics | Significance | RR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Gender (Female vs. Male) | 0.07 | 0.8 | 0.63 | 1.02 |
| Age | 0 | 0.81 | 0.71 | 0.91 |
| PI-based | <0.001 | 1.00 | ||
| TDF/3TC/EFV | 0 | 17.69 | 1216.00% | 25.73 |
| d4T/3TC/NVP | 0 | 2.17 | 1.33 | 3.56 |
| AZT/3TC/NVP | 0 | 17.21 | 668.00% | 44.35 |
| ABC/3TC/NVP | 0 | 9.95 | 3.82 | 25.87 |
| TDF/3TC/NVP | 0.51 | 1.31 | 58.00% | 2.96 |
| No hypertension | <0.001 | 1.00 | ||
| Mild hypertension | 0 | 0.09 | 6.00% | 0.14 |
| Moderate hypertension | 0 | 0.09 | 0.05 | 0.18 |
| Severe hypertension | 0.13 | 0.45 | 16.00% | 1.26 |
| Hb at baseline (>10 gm/100 cc vs. <10) | 0 | 1.84 | 1.45 | 2.34 |
| BMI at baseline (>25 vs. <25) | 0 | 1.77 | 1.24 | 2.52 |
| VL at baseline (>1000 c/ml vs. <1000) | 0.12 | 0.79 | 0.58 | 1.06 |
| CD4 at Baseline (>350 c/μL vs. <350) | 0.59 | 1.09 | 0.8 | 1.48 |
Table 9: Survival according to hypertension, adjusted for age, gender, HAART, Length of HAART administration. Baseline BMI, Hb, Viral load and CD4 count at the first contact with the service
Hypertension and survival
Compared to PI based regimen, we noticed an increased mortality and abandon risk related to other regimen with p<0.001. TDF/3TC/EFV regimen showed an increased risk of 17.69 while D4T/3TC/NVP showed only an increased risk of 2.17. Considering hypertension status, we found that all patients showed less risk at the beginning because they all had similar condition (Table 10). For hemoglobin baseline, we noticed that patients with normal/high hemoglobin had 1.84 times mortality risk compare to those less than 10 gm/dl. For BMI baseline, we also noticed that patients with high BMI (BMI>25) had 1.77 times mortality risk compare to those with BMI<25. For CD4 count and VL baseline, there were not many differences. For CD4 count, we also notice the same scenario with the bad clinical condition, (CD4 count <350 cells/ml) was associated to death/abandon with p<0.001 while patients with CD4 count more than 350 cells/ml survived more in our cohort. We see more death in those without hypertension and these people are those when were very sick and had no time to stay longer on HAART, they died in short period because of severe illness, this is followed by the severe hypertensive patients, they also died because of some complications of hypertension. As already seen in some previous tables, we clearly notice in the above table that there is no difference of survival according to gender (p=0.32) while a marginal effect of age can be observed (p=0.05). For hypertension level, we found that death/abandon was related to the treatment of hypertension, since those treated had and RR of 3.35 vs. those not treated, adjusted for the level of hypertension. However severe hypertension showed a very high relative risk of death compared to the mild one (Figure 1).
| Education level | Hypertension | Total | CHI square | ||
|---|---|---|---|---|---|
| No | With | ||||
| No education | N | 53 | 117 | 170 | p<0.001 |
| % | 31.2% | 68.8% | 100% | ||
| Primary education | N | 324 | 276 | 600 | |
| % | 54% | 46% | 100% | ||
| Secondary education | N | 265 | 248 | 513 | |
| % | 51.7% | 48.3% | 100% | ||
| Tertiary/university education | N | 33 | 34 | 67 | |
| % | 49.3% | 50.7% | 100% | ||
| Total | N | 675 | 675 | 1350 | |
| % | 50% | 50% | 100% | ||
Table 10: Incidence of hypertension according to education level
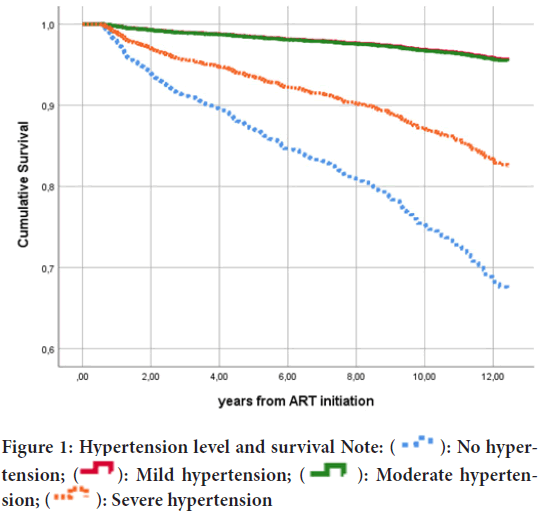
Figure 1: Hypertension level and survival Note:  : No hypertension;
: No hypertension;  : Mild hypertension;
: Mild hypertension;  : Moderate hypertension;
: Moderate hypertension;  : Severe hypertension
: Severe hypertension
The above graph shows the high mortality/abandon related to severe hypertension followed by moderate hypertension and though the difference between survival of mild and moderate hypertension is slim at the beginning, we note and gap after 9 years. We could clearly see that after 4 years of hypertension, the difference between those treated and those none treated for hypertension, patients without hypertension treatment have got low survival than those with treatment.
DISCUSSION
Impact of different ARV regimens on hypertension
Heart tissues and functions are affected by HIV as well as antiretroviral. Celermajer DS, 1997 demonstrated that endothelial malfunction is followed by clinical signs atherosclerosis. The Mechanism by what the HIV affect the endothelial function is not well explained. Nehal M and Muredach R, 2005 showed that cardiovascular risk can be increased by the atherogenic profile. The suspicion that the use of HAART increases the cardiovascular risk and its complication is still under dispute by some researchers based on the fact that atherosclerosis of the heart may take 10-15 years and the use of HAART 2-3 years cannot develop hypertension (Martin U, et al., 1999).
In this study, a very mild association between NVP-based regimen and development of hypertension, adjusted for demographic and social factor as well as for HIV infection related factors, has been observed.
Despite of very few studies investigating, the association between High blood pressure and non-nucleoside reverse transcriptase inhibitors, a prospective open-label clinical trial assessing some cardiometabolic manifestation when these patients were substituted to other new ARVs mainly rilpivirine, showed a mean systolic blood pressure reduced of 6.0 mmHg (95% CI-1.7 to -10.3; p=0.007) after 24 weeks of therapy (Rokx C, et al., 2015).
The regimen most frequently associated to the development of hypertension was the NNRTI-based regimen with nevirapine and NRTIs with tenofovir and lamivudine, 55.2% of patients on D4T developed hypertension and 56.4% on AZT developed hypertension, for PIs regimen we noticed a protective impact against hypertension, only 28.6% of patients on PIs developed hypertension this was statistically significant with p<0.001. However, it should be noted that all the regimens containing NNRTI showed a higher percentage of patients developing hypertension than the regimen containing PIs. Moreover, regimens containing nevirapine seem to be associated to the development of hypertension more frequently than the regimen containing efavirenz. After comparing only TDF/3TC/EFV with TDF/3TC/NVP we found a risk of developing hypertension in the patients receiving the nevirapine based regimen of 2.3 times higher than the ones receiving EFV (CI 95% 1.4-3.8, p<0.001).
Concerning the NRTIs, it is demonstrated that some may play a role of hypertension though the researchers have not yet come with an agreement on this point, it was found that combination of lamuvidine and tenofovir compared with lamivudine and zidovudine was related to an increased risk of hypertension in a cohort of 444 people living with HIV (p=0.046) (Crane HM, et al., 2006). Another study in prospective cohort of 527 HIV-infected and 517 HIV-uninfected adults showed that those on stavudine were independently associated with high blood pressure as well as the study of Carter M, 2016. In other way around, some studies found no association between nucleoside reverse transcriptase inhibitor use and high blood pressure (Peck RN, et al., 2014). We also see clearly the relation between the total time on HAART and the risk of developing hypertension with p<0.001 (Ngala RA and Fianko K, 2014).
We noticed that patients on PI based regimen had got less days on HAART than other regimens, because of the role played as second line treatment. This could be the reason for not seeing a clear relation between PI-regimens and development of hypertension.
Protease inhibitors mayplayarole ofhypertension in people living with HIV mainly in the physiopathology of RAAS (Renin-Angiotensin-Aldosterone System) activation, malfunction of endothelium. Lipodystrophy and dyslipidemia (Boccara F, et al., 2010), the activation of adipokine mediated inflammatory that create activation of adipose of RAAS was shown to be related to the combination of lopinavir/ritonavir (Fuchs VR, 1975).
BMI (Body Mass Index) at baseline: Good weight before starting HAART was a risk factor to develop hypertension in our cohort as shown in the Table 11. Among patients with hypertension, 184/312 representing 59%, had BMI over 25 at baseline while patients without hypertension. 52.7% had BMI<25, the p value is less than 0.001. Taking into consideration the BMI, again higher values correlate with the development of hypertension since non hypertensive patients had a mean of BMI=21.43, while the mean BMI for hypertensive patients was 23.15, hypertensive patients had about 1.8 times higher BMI compare to non-hypertensive patients. All this explains that most of our patients who developed hypertension during the period of the study came for the first time at the clinic in better health (Good BMI, good CD4 count, good HB, good creatinine) than the ones who did not develop hypertension. Our result is in correlation with the results found by Carter M, 2016 in her publication and found that HIV infection still increases the prevalence of high blood pressure prevalence after assessing for gender, age and ethnicity (p=0.002), other contributing factors were smoking BMI and physical exercise and alcohol consumption (p<0.001).
| Characteristics | Significance | RR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Gender (Female vs. Male) | 0.32 | 0.73 | 0.39 | 1.36 |
| Age | 0.05 | 1.51 | 1.00 | 2.28 |
| TDF/3TC/EFV | 1.00 | |||
| d4T/3TC/NVP | 0.55 | 1.24 | 0.61 | 2.55 |
| AZT/3TC/NVP | 0.46 | 0.68 | 0.24 | 1.91 |
| ABC/3TC/NVP | 0.21 | 3.84 | 0.48 | 3.75 |
| TDF/3TC/NVP | 0.41 | 1.54 | 0.55 | 4.36 |
| PI-based | 0.88 | 1.17 | 0.15 | 9.03 |
| Hypertension treatment (No vs. Yes) | 0.02 | 3.35 | 1.21 | 9.27 |
| Mild hypertension | 1.00 | |||
| Moderate hypertension | 0.21 | 1.61 | 0.76 | 3.42 |
| Severe hypertension | 0 | 7.72 | 2.61 | 22.79 |
| Hb at baseline (>10 gm/100 cc vs. <10) | 0.68 | 1.17 | 0.57 | 2.4 |
| BMI at baseline (>25 vs. <25) | 0.76 | 0.9 | 0.47 | 1.74 |
| VL at baseline (>1000 c/ml vs. <1000) | 0.24 | 1.54 | 0.75 | 3.14 |
| CD4 at Baseline (>350 c/µL vs. <350) | 0.46 | 1.26 | 0.68 | 2.34 |
Table 11: Survival according to hypertension level and hypertension treatment, adjusted for age, gender, HAART, length of HAART administration, baseline BMI, Hb, Viral load and CD4 count at the first contact with the service
Viral load baseline: Among patients who have viral load less<1000 copies/ml, 475/566 developed hypertension representing 83.9%. For patients who had viral load baseline over 1000 copies/ml, 584/784 did not develop hypertension representing 74.5%. p<0.001, meaning people with high viral load are at less risk to develop hypertension, and people with low viral load were those in good health and high viral load is a sign of advance HIV disease. For the viral load follow up, we noticed the same scenario, also the reduction of the gap between non hypertensive and hypertensive, the difference is 8.401, the mean VL follow up is 11.856 copies/ml while the mean for the hypertensive patients is 3.455 copies/ml.
CD4 count: A lot of studies concerning the relation between CD4 count level and hypertension in HIV positive patients have been carried out but no consensus have been found. In this study we analyzed CD4 count of patients before starting HAART and measured the CD4 count the time they developed hypertension. In total, 890 patients had CD4 count baseline<350 cells/ml and among this group 356 patients developed hypertension representing 40%; for those with CD4 count over 350 cell/ml, we had a total of 456 and among this group 69.1% developed hypertension with p<0.001. This means that, patients with CD4 count over 350 cells/ml are more likely to develop hypertension, again as mentioned already. Patients who started HAART with good health (good CD4 count, good BMI, good viral load) had an increase of risk to develop hypertension during the cascades of the HIV treatment. Our result is in line with the results found by Leite LH and Sampaio AB, 2011. Leite LH and Sampaio AB, 2011 found a significant relation between hypertension and high CD4 count in a cohort in Brazil and the advanced age and longest time on HAART. Peck RN, 2014 found similar results with hypertension related to age, alcohol use. BMI, microalbuminuria, low eGFR, and higher current CD4 T-cell count which were independently associated with hypertension. Another similar result was found by Dimala CA, et al., 2018 an association between high CD4 cell count and blood pressure and its variation with body mass index categories in HIV-infected patients.
Hemoglobin level: Hemoglobin level is also a sign of HIV disease level, when the hemoglobin level is low at baseline. In our study according to the baseline parameters, we noticed that the mean HB was low among non-hypertensive patients compare to hypertensive patients (11.2 vs.12.03); though the difference is slim but still more, we noticed that patients who started HAART with good HB had more chances to develop hypertension compare to those with low hemoglobin; we also noticed the same difference during the follow up when the mean hemoglobin is similar for non-hypertensive and hypertensive patients( 12.36 vs.12.81. Our result is in correlation with the result found by Atsma F, et al., 2012 found that mean Systolic blood pressure was increased together with Hemoglobin and increased SBP for men 1.3 mm Hg (95% CI 1.1-1.4 mm Hg) as well as HB level. For women, the increase was bit more than men with SBP increased by 1.8 mm Hg (95% CI 1.6-2.0 mm Hg) for each millimole per liter increase in Hb level. It is also shown that nitric acid is rummaged by free HB and this acid comes from the blood vessels through the endothelial cells, from there it goes into the muscles close to the vessels where by the blood pressure is controlled, so in case the HB is increased in free stage, this may be bind to Nitric oxide and increase blood pressure by vessel constriction (Cabrales P, et al., 2011). Finally, both Hb and blood pressure may be related to the renin-angiotensin-aldosterone system (Vázquez BY, 2012). Post-transplant erythrocytosis in kidney transplant recipients can be managed by angiotensin-converting enzyme inhibitor or angiotensin receptor blocker treatment (Klaassen RJ, et al., 1997) and angiotensin II may play a role in erythropoietin production (Freudenthaler SM, et al., 1999). The renin-angiotensin-aldosterone system play a role in motivating the sympathic nervous system, which will affect the erythropoietin production and this may cause anemia by autonomic neuropathy (Biaggioni I, et al., 1994).
Education level and hypertension: One of the factors we looked at was education level of our patients, this was a way to find out if well educated people have less salt intake than those less educated. While the explanation of hypertension inversely associated to education level remains unclear (Nehal M and Muredach R, 2005).
The incidence of hypertension according to the education level: In our cohort, we found that 117/170 hypertensive patients had no education (did not go to school), representing 68.8% of the total number of patients who did not go to school; p<0.001), while 34/67 among the university patients representing 50.7% had hypertension (no big difference). For intermediate education level, primary and secondary ones, we had 46% and 48.3% with p<0.001 as hypertension respectively, all these mean that most of the people who are educated know the way to prevent hypertension by controlling regularly their BP. by practicing exercise, by avoiding food which may increase the risk of hypertension.
When comparing the education level to hypertension levels, we found that for non-educated patients, stage 1 hypertension dominated with almost half of the patients 84/170 representing 49.45%, followed by pre-hypertensive patients with 53/170 representing 31.2%. Explaining that with the stage of hypertension, the stage 1 was 71.79% of the non-educated patients, (with p<0.001, statistically significant) (Table 9).
Among the primary level patients, we noticed that 324/600 had prehypertension representing 54%, with p<0.001. For secondary level patients, we also noticed that over half (51.7%) 0265/513 of them had prehypertension with p<0.001 meaning that being at secondary level is not related to a risk of hypertension. For the university level, we noticed that 40.3% had hypertension stage 1 (27/67).
Our result is comparable of the results found by Vargas CM, et al., 2005 in their cohort, they noticed that when people are educated less than 12 years. the blood pressure tend to be increased compare to those who are educated more than the same period of 12 years (Xiaojun C and Xuerui T, 2013) in china, in their study found that those less educated had higher systolic blood pressure in female concluding that low educated was related to high blood pressure in women. Another study was also conducted by Tedesco MA, et al., 2001. Also conversely, ISTAT found that 4/5 of their participants had low education level and most of their hypertensive people were men with p<0.001. A study done by Dyer AR, et al., 1976 of a cohort of 40,000 data clerks in USA, Chicago notices an inverse strong association between hypertension and education level without considering age, weight and heart.
Marital status and hypertension: In our cohort, we were also interested to see if there is an association between marital status and hypertension (Table 12). In total, 868/1350 (64.29%) were married patients men and women followed by widow 231/1350 (17.11%). We found that being married represented 54.5% of hypertension against 45.5% for non-hypertension with p<0.001. While being single, the hypertension rate was 33% (37/112). Single patients had less risk of developing hypertension; for divorced or separated patients. The rate was closer for hypertension and non-hypertension (48.9% and 51.1% respectively), for those who were widow. We noticed that over half had no hypertension 58% vs.42% (with p<0.001). This can be explained by the fact that people who are married live in an emotional stress conditions in Malawi and with the high rate of divorce in the country. Most of the people who are married live in difficult situations than those who are singles. Of course their social-economic situation is much better but this study did not find out for how long the patients have been married.
| Marital status | Hypertension | Total | p-value | ||
|---|---|---|---|---|---|
| No | With | ||||
| Divorced | N | 71 | 68 | 139 | 0.001 |
| % | 51.1% | 48.9% | 100% | ||
| Single | N | 75 | 37 | 112 | |
| % | 67% | 33% | 100% | ||
| Married | N | 395 | 473 | 868 | |
| % | 45.5% | 54.5% | 100% | ||
| Widow | N | 134 | 97 | 231 | |
| % | 58% | 42% | 100% | ||
| Total | N | 675 | 675 | 1350 | |
| % | 50% | 50% | 100% | ||
Table 12: Incidence of hypertension according to marital status
Schwandt HM, et al., 2010 found similar results; in their cohort they discovered that hypertension was not common in singles. Tuoyire DA and Ayetey H, 2019 found similar result in Ghanaian population. In their study they assessed socio demographic covariates and life style, their result showed higher risk of hypertension for those married (OR=2.14; 95% CI=1.30-3.53), partners living together and those married before women, all these results can be explained by the fact that married people have more stresses in their life, though which may be one of the causes of hypertension, but once again more investigations need to be done to find the real cause of hypertension in married people.
Survival
Mortality and hypertension: The graph below shows that the survival level is lower in patients without hypertension and most of this patients are those who were on stavudine and started HAART with very bad health conditions (p<0.001). Among hypertensive patients, we noticed a longer period of survival in patients with hypertension and treated with BP drugs compare to patients with hypertension without BP treatment (p<0.001) (Figure 2).
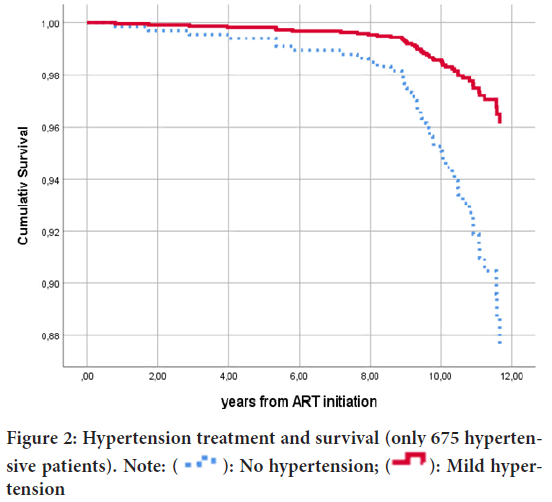
Figure 2: Hypertension treatment and survival (only 675 hypertensive patients). Note:  : No hypertension;
: No hypertension;  : Mild hypertension
: Mild hypertension
In this sample, we cannot find a clear impact of kind of ARV treatment on development of hypertension. More important seems to be life style and BMI and education. Longer time on ARVs seems to be associated to the development of hypertension (p<0.001). Our result is comparable to the results found by Gudmundsson LS, et al., 2005, in the study, they found that after a follow up of 30 years, patients with treated for hypertension but not BP well controlled (both men and women) had high risk of cardiovascular diseases and mortality compare to those who were treated and well controlled, this show the real importance of controlling hypertension. In the USA, similar result was also found by Wexler RK, 2007, in their study they noticed the inadequate hypertension control system had many implications. 99% of heart failure had experienced high blood pressure before and over 60% of patient with stroke had blood pressure before 140/90.
Survival according to hemoglobin baseline: In our cohort that patient with hemoglobin less than 10 g/dl had more abandons and death compare to those with HB>10 g/dl (40.8% vs. 13.1% respectively) we found that patients with HB>10 g/dl had more chances to be retained in our program than those with HB<10 g/dl with p<0.001, this due to the fact that low HB level is a sign of advanced illness, the chances for all these patients to die/ abandon is high. Our result is comparable to the result found by Johannessen A, et al., 2008. In their study they found that anemia at baseline was strongly associated to death with and this mortality was has as 55.1% when the HB was less than 8 g/dl, they also noticed that low BMI was associated to high mortality with 46% mortality when BMI<16.
Body mass index baseline: BMI was one of the parameters we looked in our cohort. Loss of weight is related to severe illness in HIV patients. We noticed that those who had BMI low BMI<25 had an increased risk of mortality/abandon in compared to those with BMI>25 (24.6% vs.8.7%) respectively, this is because most of patients with BMI<25 are very sick as mentioned for the low CD4 count and high Viral load. In total, the mortality/abandon was at 20.9% for all the patients regarding BMI. Johannessen A, et al., 2008 also noticed similar result in Tanzania cohort regarding survival and BMI in HIV positive patients as mentioned above. Oliveira I, et al., 2012 found in a study carried out in Guinea-bissau a strong relation between low and mortality, they noticed that Regarding the anthropometric measurements, median BMI at inclusion was 19.7 kg/m2 (IQR 17.4-22.4, n=1057) and MUAC was 256 mm (IQR 232-286, n=1064S. Martinez SS, et al., 2016 found in a cohort of a prospective study of 219 HIV positive patients, patients with BMI>25 had more survival than those with BMI<25, they also found that good baseline of BMI was associated to a lower risk of HIV-AIDS defining conditions p<0.001).
Naidoo K, et al., 2018 in a cohort of 100 infected HIV persons, they found that underweight (BMI<18.5) was associated to a high mortality (p=0.0020). There is an agreement on the relation between low BMI mainly at based line and risk of death; therefore there is a need to start HAART as soon as possible before the weight decreased
Survival according to CD4 count at baseline: In our study we note a strong association between low CD4 count and high mortality, we found that 233/657 (26.2%) died during the follow up when they started HAART with CD4 count less than 350 cells/ml, while only 49/407 (10.7%) patients died when they started HAART with CD4 count >350 cells/ml with p<0.001. Our result is in correlation of many studies regarding baseline CD4 count in patients infected with HIV. Mascolini M, 2017 found that high mortality was inversely associated with CD4 count before start HAART in a cohort of over 37,000 patients who were followed for 12 years, Mascolini M, 2017 mentioned another important factor (good adherence) which can contribute to advert the mortality in patients with low CD4 count during the follow up for a long period. In a retrospective study carried out in Ethiopia on 757 children who were HIV positive, Mulugeta A, et al., 2017 highlighted that among factors contributing to high mortality in children HIV positive were CD4 count, level of hemoglobin, stage of WHO, they noticed that children with low CD4 count at baseline had higher risk of death than those with high CD4 count, same scenario was noticed in their study regarding hemoglobin, they found that low hemoglobin at baseline was a high mortality predictor in children (Log rank, p<0.001). Oliveira I, et al., 2012 in their study in Guinea Bissau found that low CD4 count was strongly associated with high mortality; this was the same conclusion in their study regarding low BMI, high viral load at baseline. Researchers concluded the importance of starting HAART in patients when the CD4 count is over 350 cells/ml.
Viral load at baseline: The mortality related to viral load baseline is predicted by the level of viral load. High viral load is a sign of severe illness/ chronic illness in HIV naive patients. We compared survival in patients with viral load over 1000 copies vs.viral load less than 1000 copies/ml of blood, we noticed that high mortality was related to high viral load baseline and the mortality related to viral load over 1000 copies was 3.3 times the mortality related to those with viral load less than 1000 copies/ml at baseline (29.6 vs.8.8), we found a strong association between high viral load and high mortality with p=0.001, our results are similar to many researches results, in a large cohort at San Francisco, Mascolini M, 2017 noticed that RAPID ART reduces mortality related to HIV infection because of low viral load and good CD4 count. Alabi AS, et al., 2003 found similar result in a cohort of HIV-1 and HIV-2 cohort, they noticed that high viral load and low CD4 count were strongly associated to high mortality and recommended clinician to start ART as earlier as possible.
Conclusion
In conclusion, this study shows the marginal role played by ART-regimen in the development of hypertension in a large sample of sub-Saharan African HIV-positive patients. It is likely that the longer survival associated to HAART, promotes an improvement of the patients’ health status, that is linked to the development of Hypertension. In fact, all the parameters related to a better health status are independent determinants of the development of hypertension. The control of behavioural risk factors, the monitoring of blood pressure and the timely treatment of hypertension are the crucial factors to reduce the burden of hypertension on public health systems and to reduce patients’ mortality.
Study Limitations
Our cohort presented patient who were on HAART, therefore we were not able to compare the prevalence of hypertension with those who are HIV negative, we were unable to give more details concerning the real causes of hypertension related to low education level, marital status mainly those who were married, we need more socio-economic details to clarify the relation between education level, marital status and hypertension.
Recommendation
We recommend awareness of community about the risk of hypertension and especially those who are on HAART, regular BP checkup at least at every visit, treatment and good control of those with hypertension and this treatment will include diet, regular physical exercise and the BP medications.
More investigations need to be done to find real cause of hypertension related to marital status and education level and well as the drugs
References
- HIV/AIDS fact sheet. World Health Organization (WHO). 2017.
- Global health sector response to HIV, 2000-2015: Focus on innovations in Africa. World Health Organization (WHO). 2015.
- Feinstein MJ, Bahiru E, Achenbach C, Longenecker CT, Hsue P, So-Armah K, et al. Patterns of cardiovascular mortality for HIV-infected adults in the United States: 1999 to 2013. Am J Cardiol. 2016; 117(2): 214-220.
[Crossref] [Google scholar] [Pubmed]
- Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab. 2007; 92(7): 2506-2512.
[Crossref] [Google scholar] [Pubmed]
- Mutimura E, Crowther NJ, Stewart A, Todd Cade W. The human immunodeficiency virus and the cardiometabolic syndrome in the developing world: An African perspective. J Cardiometab Syndr. 2008; 3(2): 106-110.
[Crossref] [Google scholar] [Pubmed]
- Gazzaruso C, Bruno R, Garzaniti A, Giordanetti S, Fratino P, Sacchi P, et al. Hypertension among HIV patients: Prevalence and relationships to insulin resistance and metabolic syndrome. J Hypertens. 2003; 21(7): 1377-1382.
[Crossref] [Google scholar] [Pubmed]
- Kaul S, Fishbein MC, Siegel RJ. Cardiac manifestations of acquired immune deficiency syndrome: A 1991 update. Am Heart J. 1991; 122(2): 535-544.
[Crossref] [Google scholar] [Pubmed]
- Global health estimates summary tables: Projection of deaths by cause, age and sex. 2013. World Health Organization (WHO). 2013.
- Global health risks: Mortality and burden of disease attributable to selected major risks. World Health Organization (WHO). 2009.
- Himelman RB, Chung WS, Chernoff DN, Schiller NB, Hollander H. Cardiac manifestations of human immunodeficiency virus infection: A two-dimensional echocardiographic study. J Am Coll Cardiol. 1989; 13(5): 1030-1036.
[Crossref] [Google scholar] [Pubmed]
- Hecht SR, Berger M, van Tosh A, Croxson S. Unsuspected cardiac abnormalities in the acquired immune deficiency syndrome: An echocardiographic study. Chest. 1989; 96(4): 805-808.
[Crossref] [Google scholar] [Pubmed]
- Rerkpattanapipat P, Wongpraparut N, Jacobs LE, Kotler MN. Cardiac manifestations of acquired immunodeficiency syndrome. Arch Intern Med. 2000; 160(5): 602-608.
[Crossref] [Google scholar] [Pubmed]
- Medina-Torne S, Ganesan A, Barahona I, Crum-Cianflone NF. Hypertension is common among HIV-infected persons, but not associated with HAART. J Int Assoc Physicians AIDS Care (Chic). 2012; 11(1): 20-25.
[Crossref] [Google scholar] [Pubmed]
- Dysangco A, Liu Z, Stein JH, Dubé MP, Gupta SK. HIV infection, antiretroviral therapy, and measures of endothelial function, inflammation, metabolism, and oxidative stress. PLoS One. 2017; 12(8): e0183511.
[Crossref] [Google scholar] [Pubmed]
- Becker AC, Sliwa K, Stewart S, Libhaber E, Essop AR, Zambakides CA, et al. Acute coronary syndromes in treatment‐naïve black South Africans with human immunodeficiency virus infection. J Interv Cardiol. 2010; 23(1): 70-77.
[Crossref] [Google scholar] [Pubmed]
- Knudsen A, Mathiasen AB, Worck RH, Kastrup J, Gerstoft J, Katzenstein TL, et al. Angiographic features and cardiovascular risk factors in human immunodeficiency virus-infected patients with first-time acute coronary syndrome. Am J Cardiol. 2013; 111(1): 63-67.
[Crossref] [Google scholar] [Pubmed]
- Lo J, Abbara S, Shturman L, Soni A, Wei J, Rocha-Filho JA, et al. Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. AIDS. 2010; 24(2): 243.
[Crossref] [Google scholar] [Pubmed]
- Friis-Møller N, Weber R, Reiss P, Thiébaut R, Kirk O, Monforte AD, et al. Cardiovascular disease risk factors in HIV patients-association with antiretroviral therapy. Results from the DAD study. AIDS. 2003; 17(8): 1179-1193.
[Crossref] [Google scholar] [Pubmed]
- DAD study group. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007; 356(17): 1723-1735.
[Crossref] [Google scholar] [Pubmed]
- Cachay ER. Human Immunodeficiency Virus (HIV). MSD Manual Professional Version. 2023.
- Bloomfield GS, Hogan JW, Keter A, Sang E, Carter EJ, Velazquez EJ, et al. Hypertension and obesity as cardiovascular risk factors among HIV seropositive patients in Western Kenya. PloS one. 2011; 6(7): e22288.
[Crossref] [Google scholar] [Pubmed]
- Mateen FJ, Kanters S, Kalyesubula R, Mukasa B, Kawuma E, Kengne AP, et al. Hypertension prevalence and framingham risk score stratification in a large HIV-positive cohort in Uganda. J Hypertens. 2013; 31: 1372-1378.
[Crossref] [Google scholar] [Pubmed]
- Mutede BR, Magure T, Gombe NT, Bangure D, Tshimanga M. Prevalence and factors associated with hypertension among anti-retroviral therapy patients aged 15 years and above in Makonde District, Zimbabwe, 2012: An analytic cross sectional study. World J Cardiovasc Dis. 2015; 5(09): 266.
- Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: A review of the evidence. Am J Kidney Dis. 2011; 57(5): 773-780.
[Crossref] [Google scholar] [Pubmed]
- Mpondo BC, Kalluvya SE, Peck RN, Kabangila R, Kidenya BR, Ephraim L, et al. Impact of antiretroviral therapy on renal function among HIV-infected Tanzanian adults: A retrospective cohort study. PLoS One. 2014; 9(2): e89573.
[Crossref] [Google scholar] [Pubmed]
- Msango L, Downs JA, Kalluvya SE, Kidenya BR, Kabangila R, Johnson Jr WD, et al. Renal dysfunction among HIV-infected patients starting antiretroviral therapy in Mwanza, Tanzania. AIDS. 2011; 25(11): 1421-1425.
[Crossref] [Google scholar] [Pubmed]
- Dolan SE, Hadigan C, Killilea KM, Sullivan MP, Hemphill L, Lees RS, et al. Increased cardiovascular disease risk indices in HIV-infected women. J Acquir Immune Defic Syndr. 2005; 39(1): 44-54.
[Crossref] [Google scholar] [Pubmed]
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005; 365(9455): 217-223.
[Crossref] [Google scholar] [Pubmed]
- Matchaya GC. Trends in life expectancy and the macroeconomy in Malawi. Malawi Med J. 2007; 19(4): 154-158.
[Crossref] [Google scholar] [Pubmed]
- Msyamboza KP, Ngwira B, Dzowela T, Mvula C, Kathyola D, Harries AD, et al. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: Nationwide STEPS survey. Plos one. 2011; 6(5): e20316.
[Crossref] [Google scholar] [Pubmed]
- Amberbir A, Banda V, Singano V, Matengeni A, Pfaff C, Ismail Z, et al. Effect of cardio-metabolic risk factors on all-cause mortality among HIV patients on antiretroviral therapy in Malawi: A prospective cohort study. PLoS One. 2019; 14(1): e0210629.
[Crossref] [Google scholar] [Pubmed]
- Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan Africa: A systematic review and meta-analysis. Hypertension. 2015; 65(2): 291-298.
[Crossref] [Google scholar] [Pubmed]
- Countries-Malawi. World Health Organization (WHO). 2012.
- Mitambo C, Khan S, Matanje-Mwagomba BL, Kachimanga C, Wroe E, Segula D, et al. Improving the screening and treatment of hypertension in people living with HIV: An evidence-based policy brief by Malawi’s knowledge translation platform. Malawi Med J. 2017; 29(2): 224-228.
[Crossref] [Google scholar] [Pubmed]
- Celermajer DS. Endothelial dysfunction: Does it matter? Is it reversible? J Am Coll Cardiol. 1997; 30(2): 325-333.
[Crossref] [Google scholar] [Pubmed]
- Nehal M, Muredach R. Atherosclerotic cardiovascular disease risk in the HAART-treated HIV-1 population. HIV Clin Trials. 2005; 6(1): 5-24.
[Crossref] [Google scholar] [Pubmed]
- Martin U, Davies C, Hayavi S, Hartland A, Dunne F. Is normal pregnancy atherogenic? Clin Sci. 1999; 96(4): 421-425.
[Crossref] [Google scholar] [Pubmed]
- Rokx C, Verbon A, Rijnders BJ. Lipids and cardiovascular risk after switching HIV-1 patients on nevirapine and emtricitabine/tenofovir-DF to rilpivirine/emtricitabine/tenofovir-DF. AIDS Res Hum Retroviruses. 2015; 31(4): 363-367.
[Crossref] [Google scholar] [Pubmed]
- Crane HM, van Rompaey SE, Kitahata MM. Antiretroviral medications associated with elevated blood pressure among patients receiving highly active antiretroviral therapy. AIDS. 2006; 20(7): 1019-1026.
[Crossref] [Google scholar] [Pubmed]
- Peck RN, Shedafa R, Kalluvya S, Downs JA, Todd J, Suthanthiran M, et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: A cross-sectional study. BMC Med. 2014; 12(1): 1-1.
[Crossref] [Google scholar] [Pubmed]
- Ngala RA, Fianko K. Effects of HIV infection and anti-retroviral therapy on cardiovascular risk factors. Trends Mol Sci. 2014; 6(1): 1.
- Boccara F, Auclair M, Cohen A, Lefèvre C, Prot M, Bastard JP, et al. HIV protease inhibitors activate the adipocyte renin angiotensin system. Antivir ther. 2010; 15(3): 363-375.
[Crossref] [Google scholar] [Pubmed]
- Fuchs VR. Who Shall Live, 1975 New York. 1975.
- Carter M. Hypertension in patients with HIV associated with obesity, fat loss and previous treatment with stavudine. NAM AIDS Map. 2016.
- Leite LH, Sampaio AB. Risco cardiovascular: Marcadores antropométricos, clínicos e dietéticos em indivíduos infectados pelo vírus HIV. Revista de Nutrição. 2011; 24: 79-88.
- Dimala CA, Kadia BM, Kemah BL, Tindong M, Choukem SP. Association between CD4 cell count and blood pressure and its variation with body mass index categories in HIV-infected patients. Int J Hypertens. 2018.
[Crossref] [Google scholar] [Pubmed]
- Atsma F, Veldhuizen I, de Kort W, van Kraaij M, Pasker-de Jong P, Deinum J. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension. 2012; 60(4): 936-941.
[Crossref] [Google scholar] [Pubmed]
- Cabrales P, Han G, Nacharaju P, Friedman AJ, Friedman JM. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide. Am J Physiol Heart Circ Physiol. 2011; 300(1): H49-56.
[Crossref] [Google scholar] [Pubmed]
- Vázquez BY. Blood pressure and blood viscosity are not correlated in normal healthy subjects. Vasc Health Risk Manag. 2012; 8: 1.
[Crossref] [Google scholar] [Pubmed]
- Klaassen RJ, van Gelder T, Rischen-Vos J, Deinum J, Man't Veld AJ, Weimar W. Losartan, an angiotensin-II receptor antagonist, reduces hematocrits in kidney transplant recipients with posttransplant erythrocytosis. Transplantation. 1997; 64(5): 780-782.
[Crossref] [Google scholar] [Pubmed]
- Freudenthaler SM, Schenck T, Lucht I, Gleiter CH. Fenoterol stimulates human erythropoietin production via activation of the renin angiotensin system. Br J Clin Pharmacol. 1999; 48(4): 631.
[Crossref] [Google scholar] [Pubmed]
- Biaggioni I, Robertson D, Krantz S, Jones M, Haile V. The anemia of primary autonomic failure and its reversal with recombinant erythropoietin. Ann Intern Med. 1994; 121(3): 181-186.
[Crossref] [Google scholar] [Pubmed]
- Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment the NHANES I epidemiologic followup study. Am J Epidemiol. 2000; 152(3): 272-278.
[Crossref] [Google scholar] [Pubmed]
- Xiaojun C, Xuerui T. Associations of education with blood pressure in hypertensive patients: A Chinese community survey. Chin Med. 2013.
- Tedesco MA, Di Salvo G, Caputo S, Natale F, Ratti G, Iarussi D, et al. Educational level and hypertension: How socioeconomic differences condition health care. J Hum Hypertens. 2001; 15(10): 727-731.
[Crossref] [Google scholar] [Pubmed]
- Dyer AR, Stamler J, Shekelle RB, Schoenberger J. The relationship of education to blood pressure: Findings on 40,000 employed Chicagoans. Circulation. 1976; 54(6): 987-992.
[Crossref] [Google scholar] [Pubmed]
- Schwandt HM, Coresh J, Hindin MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: Incidence and prevalence in the Atherosclerosis Risk in Communities (ARIC) study participants. J Fam Issues. 2010; 31(9): 1211-1229.
[Crossref] [Google scholar] [Pubmed]
- Tuoyire DA, Ayetey H. Gender differences in the association between marital status and hypertension in Ghana. J Biosoc Sci. 2019; 51(3): 313-334.
[Crossref] [Google scholar] [Pubmed]
- Gudmundsson LS, Johannsson M, Thorgeirsson G, Sigfusson N, Sigvaldason H, Witteman JC. Hypertension control as predictor of mortality in treated men and women, followed for up to 30 years. Cardiovasc Drugs Ther. 2005; 19: 227-235.
[Crossref] [Google scholar] [Pubmed]
- Wexler RK. Treatment of hypertension critical in reducing morbidity and mortality. J Am Board Fam Med. 2007; 20(3): 322.
[Crossref] [Google scholar] [Pubmed]
- Johannessen A, Naman E, Ngowi BJ, Sandvik L, Matee MI, Aglen HE, et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008; 8(1): 1-10.
- Oliveira I, Andersen A, Furtado A, Medina C, da Silva D, da Silva ZJ, et al. Assessment of simple risk markers for early mortality among HIV-infected patients in Guinea-Bissau: A cohort study. BMJ open. 2012; 2(6): e001587.
[Crossref] [Google scholar] [Pubmed]
- Martinez SS, Campa A, Bussmann H, Moyo S, Makhema J, Huffman FG, et al. Effect of BMI and fat mass on HIV disease progression in HIV-infected, antiretroviral treatment-naïve adults in Botswana. Br J Nutr. 2016; 115(12): 2114-2121.
[Crossref] [Google scholar] [Pubmed]
- Naidoo K, Yende-Zuma N, Augustine S. A retrospective cohort study of body mass index and survival in HIV infected patients with and without TB co-infection. Infect dis poverty. 2018; 7(1): 1-6.
[Crossref] [Google scholar] [Pubmed]
- Mascolini M. CD4 count before starting HIV treatment predicts mortality for first 5 years of treatment. TheBodyPro. 2017.
- Mulugeta A, Assefa H, Tewelde T, Dube L. Determinants of survival among HIV positive children on antiretroviral therapy in public hospitals, Addis Ababa, Ethiopia. Qual Prim Care. 2017; 25(4): 235-241.
- Alabi AS, Jaffar S, Ariyoshi K, Blanchard T, van der Loeff MS, Awasana AA, et al. Plasma viral load, CD4 cell percentage, HLA and survival of HIV-1, HIV-2, and dually infected Gambian patients. AIDS. 2003; 17(10): 1513-1520.
[Crossref] [Google scholar] [Pubmed]
Author Info
Jean Baptiste Sagno*Citation: Sagno JB: Medium-Long Term Impacts of Anti-retroviral Drugs on Arterial Blood Pressure in People Living with HIV in Malawi
Received: 20-Jan-2023 Accepted: 03-Feb-2023 Published: 10-Feb-2023, DOI: 10.31858/0975-8453.14.2.131-141
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






