Research Article - (2022) Volume 13, Issue 4
Abstract
Background: Typically, Metformin-Associated Lactic Acidosis (MALA) results in Acute Kidney Injury (AKI). It has been proposed to be treated with dialysis to remove metformin. Due to the wide range of doses used, there is little information about initiating Hemodialysis (HD) with AKI and Metformin at any given dose.
Objective: To determine the relationship between risk prediction for dialysis and metformin exposure concentrations affecting AKI in hospitalized patients by comparing them to a propensity score-matched group of patients.
Methods: All type 2 diabetes patients with wide anion gap metabolic acidosis, lactic acidosis or Acute Kidney Injury were reviewed. Patients were divided into two groups based on the amount of metformin they received. Propensity Score Matching (PSM) was chosen as the predictive model for estimating probability.
Results: From 101 patients with AKI who met the study's inclusion criteria. Following matching, 53 patients and 30 controls were identified from 83 subjects. According to the ATE=0.179 result, patients taking 2000 mg or more of metformin per day are 18% more likely to develop HD than those taking less than 2000 mg.
Conclusion: When higher Metformin intake is recognized, the likelihood of receiving HD treatment increases by 0.18 or, it is attributed to an 18% increased chance of receiving HD treatment compared to those taking less than 2000 mg. The greater the dose of metformin, especially for those taking more than 2000 mg, appears to be a predictor of the need for Renal Replacement Therapy.
Keywords
Acute Kidney Injury (AKI), Hemodialysis, Lactic acidosis, Metfromin-Induced Lactic Acidosis (MALA), Metformin
Abbreviations
AKI: Acute Kidney Injury; ATE: Average Treatment Effect; EAT: Average Treatment Effects; CI: Confidence Interval; eGFR: estimated Glomerular Filtration Rate; HD: Hemodialysis; MALA: Metformin-Associated Lactic Acidosis; RRT: Renal Replacement Therapy
Introduction
Metformin is considered the first-line oral therapy in type 2 diabetes. Its primary pharmacological effect is to decrease hepatic glucose production and increase peripheral tissue insulin sensitivity. Its nonglycemic effect is weight stability (Nathan DM, et al., 2009; Dmitri K, et al., 2002). The kidney rapidly eliminates it from plasma (Scheen AJ, 1996). Previously metformin is used with caution in chronic kidney disease patients. However recent review of the literature was revised to recommend that metformin can be used safely in patients with mild (Glomerular Filtration rate; eGFR 45- 60 mL/min/m2) to moderate renal impairment (eGFR<45 mL/ min/m2). Its contraindicated in patients with eGFR<30 mL/min/ m2 and starting metformin in patients with an eGFR between 30- 45 mL/minute/1.73 m2 is not recommended (US Food and Drug Administration, 2016). However its use in clinical practice is concerned about lactic acidosis. A rare but potentially fatal complication is developed high anion gap metabolic acidosis with high blood lactates levels. It’s also called Metformin Associated Lactic Acidosis (MALA); usually develop with the conditions affecting its clearance or energy metabolism such as Acute Kidney Injury, congestive heart failure, dehydration, hepatic and respiratory failure (Renda F, et al., 2013). Treatment for MALA should include rapid vital function stabilization, correction of underlying conditions, force diuresis, and/or Renal Replacement Therapy (RRT) (Yeh HC, et al., 2017). Dialysis to remove metformin has been proposed as a treatment for MALA and has also been shown to be effective in correcting metabolic acidosis (Keller G, et al., 2011). While the RRT modality for MALA is controversial, conventional Hemodialysis seems to be efficient. A single dialysis session could remove about 60% of the total amount of metformin, and the acidosis parameters improved (Nguyen HL and Concepcion L, 2011). However, the dosage of this medication varies greatly between individuals. Unfortunately, there isn't much information about starting HD with AKI in relation to metformin at any given dose. Then, identifying this feature as an innovative predictor capable of being integrated into clinical probability assessment and prediction tools as a clinical probability assessment or prediction tool may assist clinicians in determining whether dialysis is effective and in making the decision to start dialysis.
The purpose of this study was to determine the relationship between risk prediction for dialysis and metformin exposure concentrations affecting AKI in hospitalized patients by comparing them to a propensity score-matched group of patients.
Materials and Methods
The research was carried out at the public hospital in Loei Province, Thailand. We reviewed the medical records of all type 2 diabetes patients admitted to our hospital between October 2017 and September 2020 with wide anion gap metabolic acidosis, lactic acidosis, or Acute Kidney Injury. Missing data and cases where follow-up was not possible were excluded. The overall protocol was approved by the Loei provincial public health ethics committee. The flowchart in Figure 1 illustrates the process of participant selection and the construction of propensity score-matched sets. Acute Kidney Injury patients were classified by Acute Kidney Injury (AKI) criteria (Mehta RL, et al., 2007). Baseline creatinine levels were represented by the most recent creatinine level preadmission, while in the stable state of the patients. Patients who took metformin were included in the study. On the first day of admission, demographic and clinical variables were recorded. Metformin dose, comorbidities, other medications, vasopressor, intravenous diuretic, and urine volume at 8 and 24 hours were obtained from medical records. Our primary outcome was conventional Hemodialysis requirements, stratified by metformin dose.
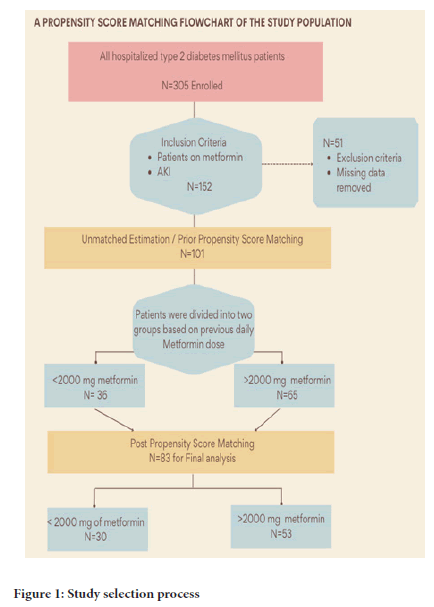
Figure 1:Study selection process
Propensity Score Matching (PSM) has been chosen as the predictive model for estimating probability. Because observational retrospective studies do not employ randomization, the subject receives the exposure, treatment, or intervention without being assigned to it. It is difficult to eliminate selection bias by splitting participants into two groups with similar characteristics because AKI related to Metformin-Associated Lactic Acidosis (MALA) is such a rare complication that only about 10 events per 100,000 patient-years of exposure have been reported (de Fronzo R, et al., 2016). As a result, MALA with Acute Kidney Injury should be extremely uncommon. Thus, by applying weights to observed characteristics, we can create two unequal groups that can be analyzed retrospectively using appropriate statistical tests and propensity scores. All statistical analyses were performed with Stata/SE 17 (Stata Corp, College Station, Texas, USA). As previously recommended (Harris H and Horst SJ, 2016), we conduct Propensity Score Matching in a series of six steps; Step 1) covariates are selected. Theoretically considerable covariates that predict group membership should be listed and included in the propensity score estimation. We make confounder selection decisions based on the most recent theoretical confounders identified in the literature on causal inference and statistical covariate selection methods. Therefore, in this step, our PSM was constructed using the following variables: Age, common comorbidities' presence/absence, urine output criteria, use of diuretics and levels of serum creatinine. Step 2) select a propensity scores model, Steps 3 and 4) choose a method for matching and generate matches by using one-to-one nearest neighbour matching with replacement for estimating the propensity score in STATA with logistic regression, step 5) balance comparison and step 6) estimating the intervention’s effects by using the Average Treatment Effect (ATE). The statistical methods were performed in accordance with published STATA Code.
Results
Based on our inclusion criteria, 101 AKI patients were identified from a total of 305 cases recruited by participants who met our inclusion criteria. Following the application of Propensity Score Matching, we were able to pair 53 treated patients with 30 controls from the remaining 83 subjects (Figure 1). The majority of patients were over 60 years old, accounting for 53.47% of the total. Of note, the average daily dose of metformin was 1792.07 ± 527.57 mg (500 mg was the lowest dose and 3000 mg was the highest). Those patients were divided into two groups based on the amount of metformin they received. A total of <2000 mg of metformin was administered to the first group (1st exposure levels), and a total of ≥ 2000 mg was administered to the second group (2nd exposure levels).
There were approximately 38% of patients receiving acute dialysis who end up receiving conventional HD. Detailed descriptions of the sample comparison between prior and post PSM, as well as its descriptive characteristics, are provided in Table 1. Among them, 66.67% were in the second exposure level group, receiving more than 2 g of metformin per day. However, there was no statistically significant difference in the need for Hemodialysis between the two groups on univariate analysis (Crude OR=1.18, 95% Confidence Interval (CI) =0.50-2.73, p=0.71).
| Characteristics | Prior to using PSM (n=101) | Post to using PSM (n=83) | % bias reduction | ||
|---|---|---|---|---|---|
| 1stexposure levels (n=36) | 2ndexposure levels (n=65) | 1stexposure levels (n=30) | 2ndexposure levels (n=53) | ||
| Age, years (mean ± SD) | 60.80 ± 8.55 | 60.04 ± 7.86 | 61.2 ± 8.99 | 60.60 ± 7.68 | 71.6 |
| Gender, % male | 38.89 | 38.46 | 46.67 | 37.74 | NA |
| Co-morbid (%Yes) | 91.67 | 86.15 | 90 | 86.79 | -3.9 |
| IV furosemide (%Yes) | 11.11 | 12.31 | 6.67 | 15.09 | 20.9 |
| Baseline creatinine (mmol/L.) (mean ± SD) | 1.04 ± 0.31 | 0.98 ± 0.28 | 1.04 ± 0.30 | 0.98 ± 0.27 | 96.7 |
| Urine 24 hrs (L.) (mean ± SD) | 1.42 ± 1.05 | 1.99 ± 1.47 | 1.47 ± 1.10 | 20.21 ± 1.53 | 82.9 |
| Metformin dosage (mg.) (mean ± SD) | 1222.22 ± 355.45 | 2107.69 ± 286.31 | 1226.66 ± 367.59 | 2064.81 ± 218.18 | NA |
Note: n=number; NA=not applicable; SD=Standard Deviation
Table 1: Table shows the characteristics of patients before and after the use of Propensity Score Matching (PSM)
The results of multivariable logistic regression revealed that metformin, age, and co-morbid baseline creatine were all insignificant variables associated with the decision to start dialysis, with the exception of urine 24 hours (as illustrated in Table 2). After matching, there were no statistically significant differences between the two groups of patients in terms of age, diuretics and levels of serum creatinine, but there were significant differences in urine volume at 24 hours and comorbidity. The overall propensity score averaged 0.003, a significant decrease from the unmatched score of 0.056. This implies that there is a fair balance between the treatment and control groups. In terms of bias reduction, only two covariates met the previous study's recommendation for reducing bias by at least 80%.
| Factors | β | 95% Confidence Interval | P |
|---|---|---|---|
| Age, per years | -0.05 | -0.12–0.02 | 0.16 |
| Co-morbid ( Yes/No) | 0.54 | -1.83–0.75 | 0.528 |
| IV furosemide ( Yes/No) | -0.86 | -2.48–2.23 | 0.294 |
| Baseline creatinine (per mmol/L.) | 0.01 | -1.83–0.75 | 0.994 |
| Urine 24 hours (per L.) | -0.0009 | -0.0014–(-0.0004) | <0.001* |
| Metformin (1st vs. 2nd exposure group) | 0.89 | -0.23–2 | 0.118 |
Note: β=beta coefficients *p<0.05
Table 2: Pre-matching multivariable logistic regression analyses
We compared two methods for estimating the likelihood that patients will undergo HD when using traditional methods for a given set of predictors based on data from each section separately. As shown in Table 3, the result of ATE=0.179 indicates that the chance of receiving HD is increased by 18 percentage points for patients who receive daily metformin doses greater than 2000 mg, as compared to patients who receive metformin at a daily dose below 2000 mg.
| Outcome | N(%) of Patients | β | 95% Confidence Interval | P** | ||
|---|---|---|---|---|---|---|
| Undergone Hemodialysis (HD) | 1stexposure levels | 2ndexposure levels | ||||
| Unmatched estimation using all five variables for adjusted odds ratios* | Total N | 36 | 65 | |||
| Yes | 13 (36.11) | 26 (40.00) | 0.88 | (-0.22 to 2.00) | 0.118 | |
| Propensity score matching using all five variables chosen for adjusted odds ratios* | Total N | 30 | 53 | |||
| Yes | 10(33.33) | 22(41.51) | 0.18*** | (0.02 to 0.34) | 0.029 | |
Note: *All five variables, including age, urine 24 hours, baseline creatinine, IV furosemide, and history of co-morbidity, were considered confounders, with the exception of gender, which was not taken into account when estimating the propensity score. **p<0.05; β=beta coefficients; N=number The result of Average Treatment Effects (EAT***)
Table 3: The association between metformin dosage and HD performed before and after propensity score matching
Discussion
Metformin inhibits pyruvate carboxylase, which results in hepatic gluconeogenesis inhibition and lactate accumulation. Thus, in the theory, AKI patients had a dramatically increased level of metformin (Rajasurya V, et al., 2019). In the cohort study of severe lactic acidosis with septic shock patients, metformin and non-metformin users, they found that among survivors, metformin users have a higher incidence of AKI and a greater frequency of Hemodialysis than non-survivor metformin users (Doenyas-Barak K, et al., 2016). However, the systematic review between 1977-2014, which searched for case reports and case series of MALA, found nearly half of enrolled patients received an inappropriate prescription of metformin based on FDA recommendation when using the GFR approach and received a significantly higher dose of metformin (2550 mg vs. 1700 mg, p<0.01) than the appropriate dosing group. Regardless, there was no statistical difference between the two groups in terms of mortality rate, serum metformin concentration (27 vs. 41.5 mg/L, p=0.27), or serum lactate level (14.2 vs. 17.5 mmol/L, p=0.27) (Yeh HC, et al., 2017). Metformin dosage was unrelated to the severity of MALA(6) (Yeh HC, et al., 2017; Vecchio S, et al., 2014; van Berlo‐van de Laar IR, et al., 2011), which may have altered RRT requirements. We discovered a statistically significant difference in RRT requirements between the lower dose metformin (2000 mg daily) and higher dose metformin (2000 mg daily) groups, which contradicting previous findings.
In this study when dealing with observational data, propensity matching methods can be used to make causal inferences by estimating treatment effect in the presence of confounding variables. This result is consistent with prior research demonstrating the utility of the many to one matching technique for PSM analysis. Notably, when the sample size is rare or when the 1:1 technique is not feasible, the matching process may become problematic (Rassen JA, et al., 2012). Our findings were consistent across regression estimates, indicating that metformin levels had no statistically significant effect on the risk of receiving HD, but metformin did have a statistically significant effect on the risk of receiving HD when full matching with multiple covariates was used. The following are some of the most notable findings from our PSM analysis: The odds of receiving HD treatment were approximately 18% higher in the higher metformin intake group than in the lower Metformin intake group when additional covariates were included in the model. The most significant contribution made by this paper is that the discovery of this attribute may assist in determining the efficacy of dialysis and may assist clinicians in evaluating the potential utility of prediction tools in their clinical practice to facilitate more equitable decision-making regarding the implementation of treatment services in correctional settings. The integration of supportive care with traditional intermittent Hemodialysis may play a crucial role in the management of AKI in this clinical scenario. The findings of two recent research provide support to this notion. First, the study by Boucaud-Maitre et al. their analyzed the factors that influence mortality related to metformin plasma levels and lactate concentrations. The results revealed that differ significantly between survivors and non-survivors (25.2 vs. 37.4 mg/l, p=0.002, 10.8 vs. 16.3 mmol- /l, p<0.001, respectively) (Boucaud‐Maitre D, et al., 2016). In accordance with the second study from Japanese, patients treated with 4-9 tablets (250 mg/tablet) exhibited substantially greater lactate levels, than those treated with 1-3 tablets (15.2 ± 0.5, 13.3 ± 0.5 mg/dL, respectively, p<0.01) (Yokoyama S, et al., 2016). Regardless of the main outcome, the benefit exists even for those treated with dialysis. This viewpoint is reflected in the notion that early dialysis to eliminate metformin from the plasma may be the treatment of choice for a patient on high-dose metformin to improve their results.
Although in some case series, the patient who presented with the worst laboratory parameters, received only supportive treatment, did not receive dialysis, and survived with the recovery of renal function (Haloob I and de Zoysa JR, 2016). Delaying the initiation of RRT may give many patients a chance to recover from AKI without dialysis. However suggesting that a "wait and see" approach is not safe for all patients, when deciding to delay RRT in patients with severe AKI, RRT should be initiated without delay if any complications such as hyperkalemia, organ edema, or medical therapy resistance are detected (Gaudry S, et al., 2016).
Despite the fact that several covariates have been addressed as a composite endpoint in various studies, some such potential factors should be prioritized. For instance, after MALA diagnosis, treatment should be alkalinizing, hemodynamic support, treatment of underlying conditions, force diuresis, and/or RRT (Pan LT and MacLaren G, 2009). Likewise, a recent clinical study detected lower plasma pH, a higher level of potassium (mean 5.651 ± 36), and lower serum proteins had a higher probability of RRT requirement. Additionally, higher potassium (mean 5.26 ± 1.15) was a prognostic factor of RRT requirements, according to our study. Rather than concentrating exclusively on the chemistry parameter, the recent observational study of AKI-MALA-RRT in the North-West of Italy showed that at admission, most patients had oliguria (Mariano F, et al., 2017). As a result, the use of intravenous furosemide in oliguric and organ edema patients and lower urine volume 24 hours after admission trended to be a prognostic factor for the RRT requirements (Crude OR=0.999, 95% CI; 0.998-0.999, p<0.01). As a result, these can be considered reasonable and therefore should be reviewed in context before incorporating our findings into clinical practice.
Limitations
First, our study is retrospective; the restoration of the data was not completed. Quite a few enrolled patients were excluded due to a loss of major data points such as baseline GFR and metformin dosage. Second, the plasma metformin concentration is not available in our hospital. However, routine assessment of metformin plasma concentration is impractical because metformin is an intracellular toxin. Likewise, any concentration of metformin may impair liver lactate clearance. It is considered that the presentation of lactic acidosis concomitant to recent ingestion of metformin may be related to this drug (Peters N, et al., 2008). A recent diagnostic study showed the combined parameters of lactate at 8.4 mmol/l and creatinine 2.89 mg/dL have a sensitivity and specificity of 85% and 95%, respectively, for identifying MALA. The specificity is increased to 99% when combining this with metformin use (van Berlo-van de Laar IR, et al., 2020). In addition, we consider MALA to be lactic acidosis or severe metabolic acidosis, which is observed in all patients with recent metformin ingestion.
Conclusion
Using the Propensity Score Matching technique, we discovered that when cofounders are considered in multivariable analyses, the odds of receiving HD treatment increase by 0.18, or 18 percent, when higher metformin intake is taken into account. Blood potassium levels, age, urine volume 24 hours after admission, intravenous diuretics, and comorbidity were all considered in relation to the risk of Hemodialysis requirements for this prediction feature.
References
- Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, et al. Medical management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy. Diabetes care. 2009; 32(1): 193-203.
[CrossRef] [Google Scholar] [Pubmed]
- Dmitri K, mc Farlane SI, James RS. Metformin: An update. Ann Intern Med. 2002; 137(1): 25-33.
[CrossRef] [Google Scholar] [Pubmed]
- Scheen AJ. Clinical pharmacokinetics of metformin. Clin Pharmacokinet. 1996; 30(5): 359-371.
[CrossRef] [Google Scholar] [Pubmed]
- US Food and Drug Administration. FDA Drug Safety Communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function. US Department of Health and Human Services. 2016.
- Renda F, Mura P, Finco G, Ferrazin F, Pani L, Landoni G. Metformin-associated lactic acidosis requiring hospitalization: A national 10 year survey and a systematic literature review. Eur Rev Med Pharmacol Sci. 2013; 17(1): 45-49.
[Google Scholar] [Pubmed]
- Yeh HC, Ting IW, Tsai CW, Wu JY, Kuo CC. Serum lactate level and mortality in metformin-associated lactic acidosis requiring renal replacement therapy: A systematic review of case reports and case series. BMC Nephrol. 2017; 18(1): 1-11.
[CrossRef] [Google Scholar] [Pubmed]
- Keller G, Cour M, Hernu R, Illinger J, Robert D, Argaud L. Management of metformin-associated lactic acidosis by continuous renal replacement therapy. PloS One. 2011; 6(8): 23200.
[CrossRef] [Google Scholar] [Pubmed]
- Nguyen HL, Concepcion L. Metformin intoxication requiring dialysis. Hemodial Int. 2011; 15: 68-71.
[CrossRef] [Google Scholar] [Pubmed]
- Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11(2): 1-8.
[CrossRef] [Google Scholar] [Pubmed]
- deFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism. 2016; 65(2): 20-29.
[CrossRef] [Google Scholar] [Pubmed]
- Harris H, Horst SJ. A brief guide to decisions at each step of the propensity score matching process. Pract Assess Res Evaluation. 2016; 21(1): 4.
- Rajasurya V, Anjum H, Surani S. Metformin use and metformin-associated lactic acidosis in intensive care unit patients with diabetes. Cureus. 2019; 11(5).
[CrossRef] [Google Scholar] [Pubmed]
- Doenyas-Barak K, Beberashvili I, Marcus R, Efrati S. Lactic acidosis and severe septic shock in metformin users: A cohort study. Crit Care. 2016; 20(1): 1-6.
[CrossRef] [Google Scholar] [Pubmed]
- Vecchio S, Giampreti A, Petrolini VM, Lonati D, Protti A, Papa P, et al. Metformin accumulation: lactic acidosis and high plasmatic metformin levels in a retrospective case series of 66 patients on chronic therapy. Clin Toxicol. 2014; 52(2): 129-135.
[CrossRef] [Google Scholar] [Pubmed]
- van Berlo‐van de Laar IR, Vermeij CG, Doorenbos CJ. Metformin associated lactic acidosis: Incidence and clinical correlation with metformin serum concentration measurements. J Clin Pharm Ther. 2011; 36(3): 376-382.
[CrossRef] [Google Scholar] [Pubmed]
- Rassen JA, Shelat AA, Myers J, Glynn RJ, Rothman KJ, Schneeweiss S. One‐to‐many propensity score matching in cohort studies. Pharmacoepidemiol Drug Saf. 2012; 21: 69-80.
[CrossRef] [Google Scholar] [Pubmed]
- Boucaud‐Maitre D, Ropers J, Porokhov B, Altman JJ, Bouhanick B, Doucet J, et al. Lactic acidosis: Relationship between metformin levels, lactate concentration and mortality. Diabet Med. 2016; 33(11): 1536-1543.
[CrossRef] [Google Scholar] [Pubmed]
- Yokoyama S, Tsuji H, Hiraoka S, Nishihara M. Investigation of risk factors affecting lactate levels in Japanese patients treated with metformin. Biol Pharm Bull. 2016; 39(12): 2022-2027.
[CrossRef] [Google Scholar] [Pubmed]
- Haloob I, de Zoysa JR. Metformin associated lactic acidosis in Auckland City Hospital 2005 to 2009. World J Nephrol. 2016; 5(4): 367.
[CrossRef] [Google Scholar] [Pubmed]
- Gaudry S, Hajage D, Schortgen F, Martin-Lefevre L, Pons B, Boulet E, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016; 375(2): 122-133.
[CrossRef] [Google Scholar] [Pubmed]
- Pan LT, MacLaren G. Continuous venovenous haemodiafiltration for metformin-induced lactic acidosis. Anaesth Intensive Care. 2009; 37(5): 830-832.
[CrossRef] [Google Scholar] [Pubmed]
- Mariano F, Pozzato M, Inguaggiato P, Guarena C, Turello E, Manes M, et al. Metformin-associated lactic acidosis undergoing renal replacement therapy in intensive care units: A five-million population-based study in the North-West of Italy. Blood Purif. 2017; 44(3): 198-205.
[CrossRef] [Google Scholar] [Pubmed]
- Peters N, Jay N, Barraud D, Cravoisy A, Nace L, Bollaert PE, et al. Metformin-associated lactic acidosis in an intensive care unit. Crit Care. 2008; 12(6): 1-5.
[CrossRef] [Google Scholar] [Pubmed]
- van Berlo-van de Laar IR, Gedik A, van‘t Riet E, de Meijer A, Taxis K, Jansman FG. Identifying patients with metformin associated lactic acidosis in the emergency department. Int J Clin Pharm. 2020; 42(5): 1286-1292.
[CrossRef] [Google Scholar] [Pubmed]
Author Info
Pattarapon Wongput1* and Chinakorn Sujimogkol1,22Department of Biostatistics, University of Michigan, Michigan, USA
Citation: Wongput P: Metformin Associated Lactic Acidosis in Acute Kidney Injury Patients: A Propensity Score Analysis
Received: 08-Mar-2022 Accepted: 29-Mar-2022 Published: 05-Apr-2022, DOI: 10.31858/0975-8453.13.4.256-260
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






