Research Article - (2023) Volume 14, Issue 7
Abstract
Objective: Oxidative Stress (OS) is a pathogenic mechanism present in Chronic Obstructive Pulmonary Disease (COPD), with a systemic effect and which can alter the quality of life of patients. The aim of this study is to study the relationship between OE and quality of life in patients with stable COPD.
Methods: Seventy-six subjects were studied, 54 with COPD and 22 controls. The amount of malondialdehyde (MDA) in serum (nmol/mL) and induced sputum (nmol/mg protein) were measured as markers of systemic and bronchial OE, respectively. In addition, quality of life was measured using the St. George’s questionnaire, which is specific for COPD patients.
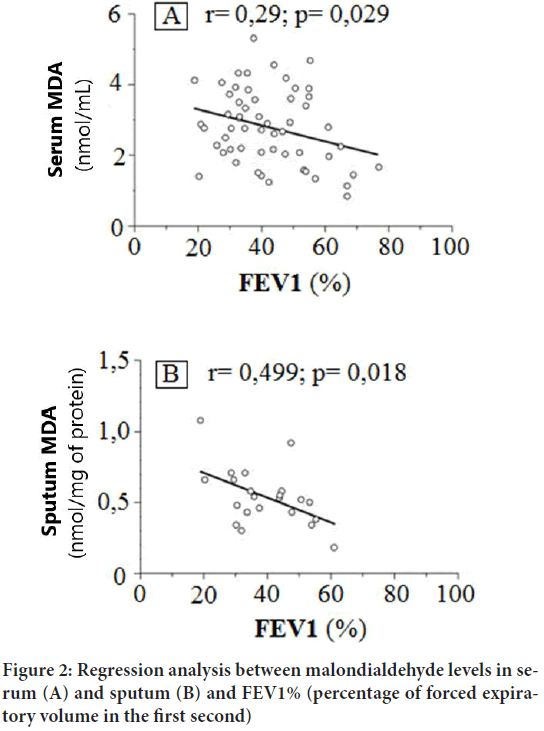
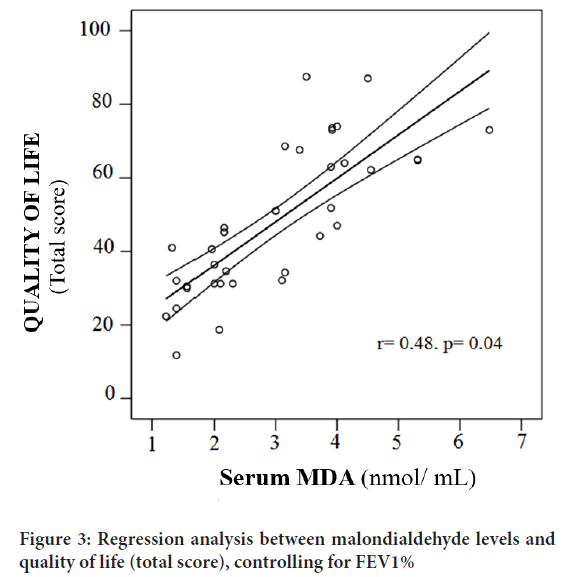
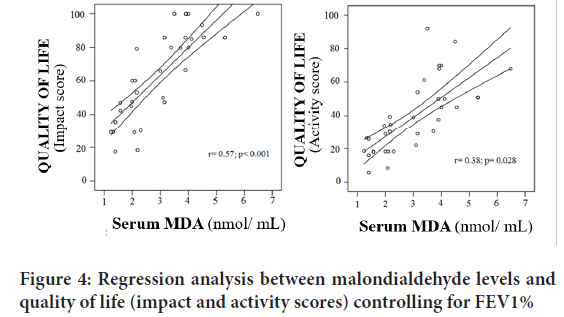
Results: Patients with COPD presented higher serum MDA levels than controls (2.98 ± 0.03 nmol/mL vs. 1.2 ± 0.03 nmol/mL, p<0.001 respectively). An inverse association was observed between Forced Expiratory Volume (FEV1)%, MDA levels in sputum (r=-0.499, p=0.018) and serum (r=-0.29, p=0.029). Finally, controlling for degree of bronchial obstruction, a direct association was observed between serum MDA levels and Total Quality of Life domains (r=0.48, p=0.04), on impact (r=0.57, p<0.001) and on activity (r=0.38, p=0.028).
Conclusion: Systemic oxidative stress is increased in stable phase COPD patients. In addition, increased bronchial obstruction increases both systemic and bronchial oxidative stress. Finally, regardless of the degree of bronchial obstruction, systemic oxidative stress decreases patients’ quality of life.
Keywords
Oxidative stress, Quality of life, COPD, Bronchial obstruction
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a disease characterized by a limitation to airflow that is not totally reversible, usually progressive and related to an abnormal inflammatory response, secondary to the inhalation of harmful particles or gases, especially tobacco (Pauwels RA, et al., 2001).
Oxidative Stress (OS) is understood to be that situation of a pathological process, derived from exposure to oxidative factors or secondary to an imbalance between systems and an adequate antioxidant capacity (especially when the latter is diminished) (Fischer BM, et al., 2015).
Today it is accepted that OS is part of the pathogenesis of COPD. Oxidizing substances can react and damage various cellular components such as cell membrane lipids, proteins (such as Alpha 1 Antitrypsin), DNA, enzymes and certain components of the extracellular matrix such as collagen (Repine JE, et al., 1997). OS in COPD begins with the inhalation of harmful substances such as tobacco. Subsequently, in the inflammatory cells “recruited” in the airways (especially polynuclear neutrophils), oxidative substances are generated that will induce cell damage and increase the inflammatory phenomenon, thus generating a “vicious circle”, which would constitute the pathogenesis of COPD (Haugen TS, et al., 1999). In COPD there is a relationship between the degree of bronchial obstruction and various OS markers derived from cellular lipid peroxidation (malondialdehyde-MDA, 8-isoprostane), Nitric Oxide (NO) and hydrogen peroxide (H2O2) among others, measured both in blood as in exhaled air. These substances are elevated both in active smoking (especially when associated with chronic airflow obstruction) and in COPD and especially during acute exacerbations (McGuinness AJ, Sapey E, 2017; Zinellu E, et al., 2017; Sahin U, et al., 2001; Oga T, et al., 2002).
When the disease progresses, the degree of bronchial obstruction increase, patients experience an impairment in their quality of life that aggravates their ability to carry out physical activities (such as walking), work (including those of a domestic nature) and even social activities. Apart from the degree of obstruction and dyspnea, one of the factors that can affect the quality of life and exercise capacity in these patients is the skeletal muscle dysfunction present in COPD (Gea J, et al., 2015). OS is one of the causes of skeletal muscle dysfunction in COPD patients and therefore capable of contributing to the impairment (decrease) in the quality of life of these patients (Couillard A, et al., 2022). On the other hand, the exercise itself, especially when it is exhaustive, can induce a pathological OS in patients with COPD, higher than in a healthy population. Apparently, the source of the pathological OS is the COPD patient’s own myocyte, which under stress and especially in certain circumstances such as hypoxia, generates oxidant radicals (Davies KJ, et al., 1982; Heunks LM, et al., 1982; Travaline JM, et al., 1997). Likewise, the OS itself present in COPD can cause functional muscle damage and early muscle fatigue with exertion, and may contribute to an alteration in the quality of life of these patients.
Due to these antecedents of OS involvement in COPD, we propose to carry out this study with the aim of seeing if there is a relationship between OS and quality of life in COPD patients.
Materials and Methods
76 subjects were included, 54 patients diagnosed with COPD (GOLD stage III) in stable phase without exacerbations or using systemic steroids during the previous six weeks and less than two moderate exacerbations or one severe exacerbation in the previous year and 22 healthy controls nonsmokers. All patients had a non-reversible obstruction, defined by a post-salbutamol FEV1 less than 12% of the baseline value. All patients were treated according to the Spanish Guidelines for Chronic Obstructive Pulmonary Disease (GesPOC) receiving two bronchodilators-a combination of an inhaled betamimetic and a long-acting anticholinergic. All study subjects were on a similar standard diet, with no added vitamin supplements or antioxidants. Spirometry was performed on each of the studied subjects using a Datospir type pneumotachograph (Sibel Med. Barcelona), according to SEPAR regulations (Aldás JS, et al., 1998).
The quantification of systemic (blood) and local (bronchial) oxidative stress was obtained by determining the levels of Malondialdehyde (MDA) in blood (COPD patients and control group) and induced sputum (34 COPD patients), through the reaction of thiobarbituric acid (TBARS), according to the method described by Djukanović R, et al., 2002 and Kikugawa K, et al., 1992. MDA values were expressed in blood in nmol/ml of serum and in sputum in nmol/mg of proteins. Induced sputum determinations were not performed in the control group, due to the impossibility of obtaining adequate and analyzable samples according to current standards.
The different comorbidity variables that could modify the EO values will be controlled using the Charlson test. The St. George questionnaire was self-administered to each of the COPD patients to measure quality of life, which is specific for COPD patients. In case of difficulty in reading it, it was administered by one of the researchers in a supervised manner and avoiding influencing the responses of the subjects. The questionnaire contains 50 items divided into a total score and three subscales: Symptoms, activity and the impact of the disease. The symptom scale refers to the frequency and intensity of symptoms; the activity scale determines the limitation of the various physical activities due to dyspnea and impact; it contains aspects related to psychological and social alterations, produced by the respiratory disease itself. Scores range from 0 to 100 and are calculated separately for each of the scales as well as a total score, the sum of all responses to all articles. A score of 0 indicates no deterioration in quality of life, while a score of 100 identifies the maximum deterioration. The questionnaire translated and validated into Spanish was used (Jones PW, 2001; Jones PW, et al., 1992; Ferrer M, et al., 1996). The study was approved by the Ethics Committee of the hospital.
Statistical analysis
The results of the quantitative variables are expressed with means and standard deviations. For the comparisons of means, the Student’s T-test was used, the correlations between MDA levels and quality of life were estimated with Pearson’s correlation coefficient. The relationship between MDA levels and quality of life, controlling for the degree of bronchial obstruction (FEV1) was modeled using linear regression. Values of p<0.05 were considered significant. Data were analyzed with the SPSS/PC statistical package, version 8.0 (Chicago, IL).
Results and Discussion
The baseline characteristics of the subjects are shown in Table 1. MDA blood levels in COPD patients were higher (2.98 ± 0.03 nmol/ml) than in controls (1.2 ± 0.03 nmol/ml); p<0.001 (Figure 1). Likewise, MDA levels both in sputum (r=0.499; p=0.018) and serum (r=0.29; p=0.029) increased with the degree of bronchial obstruction (Figure 2). Finally, the relationship between MDA levels in blood and quality of life was analyzed by controlling the degree of bronchial obstruction. The relationship between MDA in blood and the deterioration of quality of life was positive both globally (r=0.48; p=0.04) (Figure 3) and in the impact subscales (r=0.57; p<0.001) and activity (r=0.38; p=0.028) (Figure 4), not finding a relationship with symptoms.
| Age (in years) | COPD (n=78) | Controls (n=22) | p |
|---|---|---|---|
| Gender (males)-no. (%) | 66 ±1 | 68 + 18 | NS |
| 68 (87) | 18 (82) | NS | |
| FEV1 (%) | 38.9 ± 1.7 | 97 | p<0.001 |
| Severity score (Charlson) | 3.6 + 0.1 | 3.2 + 0.3 | NS |
| BMI (Kg/m2) | 32.1 + 3 | 33.5 + 4 | NS |
| FEV1 (litres) | 1.07 | 2.96 ± 2.3 | p<0.001 |
| FEV1% | 38.9 + 1.7 | 86 ± 2 | p<0.001 |
| FVC (litres) | 2.2 ± 0.9 | 3.2 ± 1.2 | p<0.001 |
| FVC (%) | 53 ± 2.3 | 89 ± 3.8 | p<0.001 |
| FEV1/FVC (%) | 48.6+ | 75.8 + | p<0.001 |
Table 1: Clinical and demographic characteristics of patients and controls
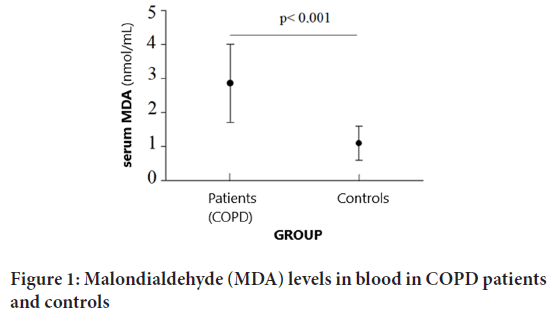
Figure 1: Malondialdehyde (MDA) levels in blood in COPD patients and controls
Figure 2: Regression analysis between malondialdehyde levels in serum (A) and sputum (B) and FEV1% (percentage of forced expiratory volume in the first second)
Figure 3: Regression analysis between malondialdehyde levels and quality of life (total score), controlling for FEV1%
Figure 4: Regression analysis between malondialdehyde levels and quality of life (impact and activity scores) controlling for FEV1%
In our study, we found an increase in systemic oxidative stress in severe COPD patients in stable phase, an inverse relationship between the level of systemic and bronchial oxidative stress with the degree of obstruction and a direct and independent relationship of the degree of bronchial obstruction between systemic OS and quality of life, especially in the impact and activity scales.
The increase in blood OS in stable phase COPD patients found in our study is a fact confirmed by other authors (Fischer BM, et al., 2015; Repine JE, et al., 1997; Zinellu E, et al., 2016). This is due to the fact that although initially exposure to tobacco smoke and later local inflammation induce OS at the bronchial level (sputum and expired air can be detected), it would later spread to the systemic level, being able to be detected in the blood, as well as in various tissues (such as striated muscle) (Jaitovich A and Barreiro E, 2018; Rahman I, et al., 1996).
Regarding the direct relationship between systemic/bronchial OS and degree of bronchial obstruction, there are several studies that confirm this finding (Kluchová Z, et al., 2007).
In our study, we found an indirect relationship between MDA in sputum and FEV1. Up to now, the usual quantification of bronchial OS was carried out by means of the direct detection and quantification of oxidative reactive substances (such as H2O2) or of biological derivatives of oxidative impact, especially lipids (lipid peroxidation), in exhaled or condensed air (Zeng M, et al., 2013). In our work, this relationship was carried out directly in induced sputum, by quantifying the MDA. This relationship is due to the fact that the greater the degree of inflammation and therefore the bronchial OS, the lower the FEV1 will be and the greater the degree of bronchial obstruction. This quantification of MDA in sputum could be used as an alternative to that carried out in exhaled air. The determination of MDA in other biological fluids, apart from sputum, has shown high stability, even in ambient air, with a high acceptable intra-class correlation coefficient, a fact that could make it a quantitative and safe determination of OS at the bronchial level (Paredi P, et al., 2000; Lee KH and Kang D, 2008).
In this study, a direct relationship was also found between systemic oxidative stress (MDA in blood) and quality of life in COPD patients, especially in the impact and activity scales. The quality of life of COPD patients, especially in severe patients, is related to dyspnea, degree of bronchial obstruction, number of exacerbations, body mass index, and degree of basic physical activity (de Miguel Díez J, et al., 2004). On the other hand, the degree of bronchial obstruction is related, not only to the local (bronchial) level of OS, but also to the systemic one (Tsukagoshi H, et al., 2000; Kostikas K, et al., 2003; Montuschi P, et al., 2000; Clini E, et al., 1998; Agusti A, et al., 2003; Barbaro MF, et al., 2007; Serviddio G, et al., 2006; Fermoselle C, et al., 2012). Therefore, it seems logical that there is a relationship between OS in blood and the impact and activity scales of the St. George QoL test.
Likewise, we found a direct and independent relationship between the degree of bronchial obstruction between levels of MDA in blood (systemic OS) and quality of life, both in the impact and activity scale. The relationship with the activity scale could be explained through a possible effect of the OS on muscle function (muscle dysfunction), which would contribute to the physical limitation that these patients have and its impact on their quality of life. Muscle dysfunction in COPD patients is multifactorial. Tissue hypoxia, malnutrition and OS constitute the pathophysiological basis of this dysfunction.
Various authors have found a relationship between OS and muscle dysfunction in COPD (Fermoselle C, et al., 2012). Koechlin et al, observed that there was an inverse relationship between local (muscular) and systemic (blood) OS and muscular endurance of the quadriceps in patients with COPD. Likewise, these same authors observed that intense exercise increased muscle and blood OS (systemic) in these patients (Koechlin C, et al., 2004). Similarly, Couillard A, et al., 2003, obtained similar results to the previous ones, where bronchial OS (local) was associated with muscle dysfunction in patients with COPD (Couillard A, et al., 2003). One of the mechanisms by which OS can produce muscle dysfunction in COPD patients is by stimulating cellular proteolysis at this level and leading to a loss of muscle mass (Mitch WE and Goldberg AL, 1996). On the other hand, the OS present in COPD patients can induce a peroxidation of lipids present in various cell membranes, including mitochondrial membranes, which would lead to a decrease in muscle energy production and the appearance of skeletal muscle dysfunction (Taivassalo T, Hussain SN, 2016; Berton E, et al., 2001; Barreiro E, et al., 2008; Haji G, et al., 2020; Gifford JR, et al., 2018).
Conclusion
In our study, although a relationship was found between MDA levels in sputum and symptom scales, it did not reach statistical significance (p<0.07) (data not shown in results). There is an increase in systemic oxidative stress in COPD patients in stable phase. Similarly, there is an inverse relationship between the degree of bronchial obstruction and systemic (blood) and local (bronchial) oxidative stress in COPD patients. Further, there is a direct relationship between systemic oxidative stress (blood) and quality of life in COPD patients.
Author Contributions
Preparation of the study and data collection was carried out by J Abreu González, CC Casanova Macarios JP, From Torres Tajés. Laboratory determinations were carried out by P Abreu González. A. Jimenez Sosa was involved in Statistical study and C. Martin García studied about the Respiratory function studies.
Ethical Approval
The study was approved by the Ethics Committee of the Hospital Universitario de Canarias.
Consent for Publication
Consent to participate in the study was requested from each patient and its subsequent publication.
Availability of Data and Materials
If necessary, the data set used in the study will be accessible.
References
- Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001; 163(5): 1256-1276.
[Crossref] [Google Scholar] [Pubmed]
- Fischer BM, Voynow JA, Ghio AJ. COPD: Balancing oxidants and antioxidants. Int J Chron Obstruct Pulmon Dis. 2015: 261-276.
[Crossref] [Google Scholar] [Pubmed]
- Repine JE, Bast AA, Lankhorst ID, Oxidative Stress Study Group. Oxidative stress in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997; 156(2): 341-357.
[Crossref] [Google Scholar] [Pubmed]
- Haugen TS, Skjonsberg OH, Kahler H, Lyberg T. Production of oxidants in alveolar macrophages and blood leukocytes. Eur Respir J. 1999; 14(5): 1100-1105.
[Crossref] [Google Scholar] [Pubmed]
- McGuinness AJ, Sapey E. Oxidative stress in COPD: Sources, markers, and potential mechanisms. J Clin Med. 2017; 6(2): 21.
[Crossref] [Google Scholar] [Pubmed]
- Zinellu E, Zinellu A, Fois AG, Carru C, Pirina P. Circulating biomarkers of oxidative stress in chronic obstructive pulmonary disease: A systematic review. Respir Res. 2016; 17: 1.
[Crossref] [Google Scholar] [Pubmed]
- Sahin U, Unlü M, Ozgüner F, Sütcü R, Akkaya A, Delibas N. Lipid peroxidation and glutathione peroxidase activity in chronic obstructive pulmonary disease exacerbation: Prognostic value of malondialdehyde. J Basic Clin Physiol Pharmacol. 2001; 12(1): 59-68.
[Crossref] [Google Scholar] [Pubmed]
- Oga T, Nishimura K, Tsukino M, Hajiro T, Ikeda A, Mishima M. Relationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary disease. Heart Lung. 2002; 31(5): 374-381.
[Crossref] [Google Scholar] [Pubmed]
- Gea J, Pascual S, Casadevall C, Orozco-Levi M, Barreiro E. Muscle dysfunction in chronic obstructive pulmonary disease: Update on causes and biological findings. J Thorac Dis. 2015; 7(10): E418.
[Crossref] [Google Scholar] [Pubmed]
- Couillard A, Koechlin C, Cristol JP, Varray A, Prefaut C. Evidence of local exercise-induced systemic oxidative stress in chronic obstructive pulmonary disease patients. Eur Respir J. 2002; 20(5): 1123-1129.
[Crossref] [Google Scholar] [Pubmed]
- Davies KJ, Quintanilha AT, Brooks GA, Packer L. Free radicals and tissue damage produced by exercise. Biochemical and biophysical research communications. 1982; 107(4): 1198-1205. Biochem Biophys Common Res. 1982; 107: 1198-1205.
[Crossref] [Google Scholar] [Pubmed]
- Heunks LM, Viña J, van Herwaarden CL, Folgering HT, Gimeno A, Dekhuijzen PR. Xanthine oxidase is involved in exercise-induced oxidative stress in chronic obstructive pulmonary disease. Am J Physiol. 1999; 277(6): R1697-R1704.
[Crossref] [Google Scholar] [Pubmed]
- Travaline JM, Sudarshan S, Roy BG, Cordova F, Leyenson V, Criner GJ. Effect of N-acetylcysteine on human diaphragm strength and fatigability. Am J Respir Crit Care Med. 1997; 156(5): 1567-1571.
[Crossref] [Google Scholar] [Pubmed]
- Aldás JS, Clará CP, Gómez JC, Mangado NG, Ballesteros LP, Torrent JR. Forced spirometry. 1998.
- Djukanović R, Sterk PJ, Fahy JV, Hargreave FE. Standardised methodology of sputum induction and processing. Eur Respir J Suppl. 2002; 20(37 suppl):1s-2s.
[Crossref] [Google Scholar] [Pubmed]
- Kikugawa K, Kojima T, Yamaki S, Kosugi H. Interpretation of the thiobarbituric acid reactivity of rat liver and brain homogenates in the presence of ferric ion and ethylenediaminetetraacetic acid. Anal Biochem. 1992; 202(2): 249-255.
[Crossref] [Google Scholar] [Pubmed]
- Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001; 56(11): 880-887.
[Crossref] [Google Scholar] [Pubmed]
- Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. Am Rev Respir Dis. 1992; 145(6): 1321-1327.
[Crossref] [Google Scholar] [Pubmed]
- Ferrer M, Alonso J, Prieto L, Plaza V, Monsó E, Marrades R, et al. Validity and reliability of the St George's Respiratory Questionnaire after adaptation to a different language and culture: The Spanish example. Eur Respir J. 1996; 9(6): 1160-1166.
[Crossref] [Google Scholar] [Pubmed]
- Jaitovich A, Barreiro E. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. What we know and can do for our patients. Am J Respir Crit Care Med. 2018; 198(2): 175-186.
[Crossref] [Google Scholar] [Pubmed]
- Rahman I, Morrison D, Donaldson K, MacNee W. Systemic oxidative stress in asthma, COPD, and smokers. Am J Respir Crit Care Med. 1996; 154(4): 1055-1060.
[Crossref] [Google Scholar] [Pubmed]
- Kluchová Z, Petrášová D, Joppa P, Dorková Z, Tkáčová R. The association between oxidative stress and obstructive lung impairment in patients with COPD. Physiol Res. 2007; 56(1): 51-56.
[Crossref] [Google Scholar] [Pubmed]
- Zeng M, Li Y, Jiang Y, Lu G, Huang X, Guan K. Local and systemic oxidative stress and glucocorticoid receptor levels in chronic obstructive pulmonary disease patients. Can Respir J. 2013; 20: 35-41.
[Crossref] [Google Scholar] [Pubmed]
- Paredi P, Kharitonov SA, Leak D, Ward S, Cramer D, Barnes PJ. Exhaled ethane, a marker of lipid peroxidation, is elevated in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000; 162(2): 369-373.
[Crossref] [Google Scholar] [Pubmed]
- Lee KH, Kang D. Stability and intra-individual variation of urinary malondialdehyde and 2-naphthol. J Prev Med Public Health. 2008; 41(3): 195-199.
[Crossref] [Google Scholar] [Pubmed]
- de Miguel Díez J, Alonso JI, González-Moro JR, de Lucas Ramos P, Cano JB, París JM. Quality of life with chronic obstructive pulmonary disease: The influence of level of patient care. Arch Bronconeumol. 2004; 40(10): 431-437.
[Crossref] [Google Scholar] [Pubmed]
- Tsukagoshi H, Shimizu Y, Iwamae S, Hisada T, Ishizuka T, Iizuka K, et al. Evidence of oxidative stress in asthma and COPD: Potential inhibitory effect of theophylline. Respir Med. 2000; 94(6): 584-588.
[Crossref] [Google Scholar] [Pubmed]
- Kostikas K, Papatheodorou G, Psathakis K, Panagou P, Loukides S. Oxidative stress in expired breath condensate of patients with COPD. Chest. 2003; 124(4): 1373-1380.
[Crossref] [Google Scholar] [Pubmed]
- Montuschi P, Collins JV, Ciabattoni G, Lazzeri N, Corradi M, Kharitonov SA, Barnes PJ. Exhaled 8-isoprostane as an in vivo biomarker of lung oxidative stress in patients with COPD and healthy smokers. Am J Respir Crit Care Med. 2000; 162(3): 1175-1177.
[Crossref] [Google Scholar] [Pubmed]
- Clini E, Bianchi L, Pagani M, Ambrosino N. Endogenous nitric oxide in patients with stable COPD: Correlates with severity of disease. Thorax. 1998; 53(10): 881-883.
[Crossref] [Google Scholar] [Pubmed]
- Agusti AG, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2003; 21(2): 347-360.
[Crossref] [Google Scholar] [Pubmed]
- Barbaro MF, Carpagnano GE, Spanevello A, Cagnazzo MG, Barnes PJ. Inflammation, oxidative stress and systemic effects in mild chronic obstructive pulmonary disease. Int J Immunopathol Pharmacol. 2007; 20(4): 753-763.
[Crossref] [Google Scholar] [Pubmed]
- Serviddio G, Carpagnano GE, Rollo T, Tamborra R, Barbaro MF, Vendemiale G, et al. Evidence of lower oxidative stress in the air spaces of patients with reversible COPD. Int J Immunopathol Pharmacol. 2006; 19(3): 617-628.
[Crossref] [Google Scholar] [Pubmed]
- Fermoselle C, Rabinovich R, Ausín P, Puig-Vilanova E, Coronell C, Sanchez F, et al. Does oxidative stress modulate limb muscle atrophy in severe COPD patients? Eur Respir J. 2012; 40(4): 851-862.
[Crossref] [Google Scholar] [Pubmed]
- Koechlin C, Couillard A, Simar D, Cristol JP, Bellet H, Hayot M, et al. Does oxidative stress alter quadriceps endurance in chronic obstructive pulmonary disease? Am J Respir Crit Care Med. 2004; 169(9): 1022-1027.
[Crossref] [Google Scholar] [Pubmed]
- Couillard A, Maltais F, Saey D, Debigaré R, Michaud A, Koechlin C, et al. Exercise-induced quadriceps oxidative stress and peripheral muscle dysfunction in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2003; 167(12): 1664-1669.
[Crossref] [Google Scholar] [Pubmed]
- Mitch WE, Goldberg AL. Mechanisms of muscle wasting-the role of the ubiquitin-proteasome pathway. N Engl J Med. 1996; 335(25): 1897-1905.
[Crossref] [Google Scholar] [Pubmed]
- Taivassalo T, Hussain SN. Contribution of the mitochondria to locomotor muscle dysfunction in patients with COPD. Chest. 2016; 149(5): 1302-1312.
[Crossref] [Google Scholar] [Pubmed]
- Berton E, Antonucci R, Palange P. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. Monaldi Arch Chest Dis. 2001; 56(5): 418-422.
[Google Scholar] [Pubmed]
- Barreiro E, Schols AM, Polkey MI, Galdiz JB, Gosker HR, Swallow EB, et al. Cytokine profile in quadriceps muscles of patients with severe COPD. Thorax. 2008; 63(2): 100-107.
[Crossref] [Google Scholar] [Pubmed]
- Haji G, Wiegman CH, Michaeloudes C, Patel MS, Curtis K, Bhavsar P, et al. Mitochondrial dysfunction in airways and quadriceps muscle of patients with chronic obstructive pulmonary disease. Respir Res. 2020; 21(1): 1.
[Crossref] [Google Scholar] [Pubmed]
- Gifford JR, Trinity JD, Kwon OS, Layec G, Garten RS, Park SY, et al. Altered skeletal muscle mitochondrial phenotype in COPD: Disease vs. disuse. J Appl Physiol. 2018; 124(4): 1045-1053.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Juan Abreu González1*, Pedro Abreu González2, Alejandro Jiménez Sosa3, Ciro Casanova Macarios4, De Torres Tajés5 and Martin Garc�a12Department of Human Physiology, University of La Laguna, San Cristóbal de La Laguna, Spain
3Department of Hospital Research, Hospital Universitario de Canarias, San Cristóbal de La Laguna, Spain
4Department of Human Physiology, Hospital Universitario Nuestra Senora de Candelaria, Santa Cruz de Tenerife, Spain
5Department of Pneumology, Hospital Universitario de Canarias, Navarra, Spain
Citation: González JA: Oxidative Stress and Quality of Life in Severe COPD in Stable Phase
Received: 12-Jun-2023 Accepted: 07-Jul-2023 Published: 14-Jul-2023, DOI: 10.31858/0975-8453.14.7.452-456
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3