Research Article - (2021) Volume 12, Issue 11
Retinal Nerve Fiber Layer, Ganglion Cell Complex and Choroidal Thickness Evaluation in Patients with Obstructive Sleep Apnea Syndrome
Ela Eren1*, Nilüfer Ilhan2 and Sebahat Genç3Abstract
Introduction: To evaluate the association of Obstructive Sleep Apnea Syndrome (OSAS) with Retinal Nerve Fiber Layer (RNFL), Ganglion Cell Complex (GCC) and Choroidal Tissue Thickness (CCT).
Methods: This cross-sectional study included 50 patients with OSAS and 50 controls between July 2014-January 2015). OSAS severity was classified by using the Apnea-Hypopnea Index (AHI). RNFL thickness, GCC thickness and CCT analyses were performed by Optic Coherence Tomography (OCT). Statistical analysis was performed using SPSS for Windows version 21 software.
Results: The mean Intraocular Pressure (IOP) of the patients with OSAS 16.1 ± 1.37, the cup/disc (C/D) ratio was 0.45 ± 0.17 and vertical C/D ratio was 0.43 ± 0.16. The control group mean IOP was 15.2 ± 1.03, the C/D ratio was 0.36 ± 0.20 and vertical C/D ratio was 0.34 ± 0.19. These are all important measurements in glaucome and statistically significant (p=0.00, 0.022, 0.012). Although the differences between the mean values of all quadrants RNFL thickness were similarly lower in OSAS group, this significance was not statistically different. Similarly, the average GCC, minimum GCC and subfoveal CCT values between groups were not significant (p=0.79, 0.53, 0.9).
Conclusion: In summary we found that peripapillary RNFL, GCC, CCT did not change with OSAS patients or the severity of OSAS. Furthermore, we found that IOP, C/D ratio and vertical C/D ratio of patients were all significantly higher than control group. However, multicenter longterm cohort studies are still needed to assess the definite changes of RNFL thickness, GCC and CCT in OSAS patients.
Keywords
OSAS, OCT, Glaucoma, Ganglion, Choroid
Introduction
Obstructive Sleep Apnea Syndrome (OSAS) is a breathing disorder which is related of oxygen desaturation during sleep. Especially it causes complete collapse of the pharyngeal air- way or partial collapse repetitively during sleep and generally ends with reduction in oxygen desaturation. Overnight Poli- somnography (PSG) is the gold standard in diagnosis of OSAS (Guilleminault C, 1994). The prevalence of OSAS is estimated to be 1% to 2% in men and 1.2% to 2.5% in women around the world (Young T, et al., 2002; Young T, et al., 1993). The prev- alence of OSAS in Turkey was reported as 1.8% (Köktürk O, 1998). The treatment of OSAS is Continuous Positive Airway Pressure (CPAP). OSAS causes hypoxia, hypercapnia and low oxygen saturation. The balance between vasodilatation and vasoconstriction in blood vessels is broken (Köktürk O, 1998; Caples SM, et al., 2007; Yuvaci I, et al., 2016).
OSAS is also associated with ophthalmic disorders. There are many reports in the pathogenesis theories of vascular compli- cations which can caused by that inflammatory processes, ox- idative stress, endothelial dysfunction and vascular remodel- ling in ocular disorders (Yuvaci I, et al., 2016; Arnaud C, et al., 2009). These changes may disrupt the perfusion of the Optic Nerve Head (ONH) and this result in ganglion cell loss. As a result, optic nerve may become more sensitive to increases in the intraocular pressure or optic nerve glaucomatous damage may develop even with normal intraocular pressure. The prev- alence of glaucoma in the OSAS was found to be 5.9% to 27% by several studies (Jelic S, Le Jemtel TH, 2008; Khandgave TP, et al., 2013; Bendel RE, et al., 2008).
Spectral-domain Optical Coherence Tomography (OCT) provides quantitative and reproducible measurements for in- vestigating RNFL thickness in glaucoma. In recent studies, a decreased RNFL thickness and increased ONH area-vol- ume parameters measured with OCT have been reported in patients with OSAS (Mojon DS, et al., 1999; Lin PW, et al., 2011). The choroid is a vascular layer between the sclera and the retina. The choroid evaluation can be used for detecting of systemic vascular injury. New-generation spectral domain OCT with enhanced scanning speed shows us to see high-res- olution images with more accurate measurements. In recent studies, OCT was an effective device for evaluating Choroidal Tissue Thickness (Casas P, et al., 2003). Previous studies also have been suggested that OSAS may also trigger the macular Ganglion Cell Complex (GCC) loss. In recent years GCC can be measured by OCT (Mojon DS, et al., 1999; Lin PW, et al., 2011; Casas P, et al., 2003; Maul EA, et al., 2011).
OSAS have effects on RNFL, GCC, macula and choroidal tis- sue. But overall studies have conflicting results. These studies especially focused on the prevalance of glaucoma or choroidal thickness of OSAS patients. In our study we evaluate all pos- terior ocular structures and whether there was a correlation between these structures and the clinical severity of OSAS.
Methods
This cross-sectional study included 50 patients with OSAS and 50 age-sex matched controls between July 2014-January 2015. The study was directed in according with the Declaration of Helsinki for bio- medical research and the study protocol was approved by the local ethics committee of Mustafa Kemal University School of Medicine (18/08/2014/152). All participants were given informed consent.
Diagnoses of OSAS was based on overnight PSG (Compumedics E Series 44 channel polysomnograph, Profusion PSG3 Software (Abbotsford, VIC, Aus- tralia)). OSAS severity was classified by using the Apnea-Hypopnea Index (AHI), which was defined as the number of apnea and hypopnea per hour of total sleep time. Apneas were full cessation of airflow more than 10 s. Hypo- pneas were defined as reduction of >50% in air flow signal with a fall of ≥ 3% in oxygen saturation or an arousal. Apneas and hypopneas were considered during the sleep time and AHI ≥ 5 were considered as OSAS and those with AHI 5-15 were regarded as having mild, AHI 15-30 to have moderate and AHI >30 to have severe OSAS.
All patients underwent a detailed ophthalmic examination. Visual acuity test- ing, refraction assessment, biomicroscopic investigation, intraocular pressure measurement with Goldman aplanation tonometry and fundus examination were all done. All participants were examined with OCT device (Cirrus HD- OCT 4000 (Carl Zeiss Meditec Inc., Dublin, CA, USA)). Temporal, nasal, in- ferior, superior and average RNFL thickness values were obtained. Data for RNFL thickness were acquired using the ‘Optic Disc Cube 200 × 200' protocol. The GCC mapping was conducted based on macular protocol centered on fovea with a cube of 512 × 128 with automated measurement of the GC-IPL thickness. Choroidal thickness obtained by enhanced depth modality of OCT (? =840 nm, 26000 A scans/s, and 5 µm axial resolution). The choroidal thick- ness was shown as the vertical distance between the high-reflective Retinal Pigment Epithelium (RPE) edge and the choroid-sclera junction line. Diurnal variations may exist in the choroidal thickness measurements (Marcus DM, etal., 2001); therefore, all of the measurements were performed between 09:00 and 12:00 with same ophtalmologist (E.E).
The exclusion criterias from the study were patients with a history of ocular surgery, ocular trauma, any anterior or posterior segment disease, all glauco- mas even normotensive glaucoma and ocular hypertension. Systemic hyper- tension and diabetes mellitus can affect the optic nerve and choroidal blood flow so we also exclude the patients who have these diseases.
Statistical analysis was performed using SPSS for Windows version 21 soft- ware (SPSS Inc, Chicago, IL, USA). The descriptive statistics for continuous variables were expressed as mean ± standard deviation and the significance of the difference between the mean values of the groups was evaluated using the Stundent’s t-test. A p value less than 0.05 was considered statistically signif- icant. Comparison between mean values of groups was evaluated by Pearson’s correlation tests. Pearson’s correlation efficient was used to measure strength and direction of the linear relationship between two variables.
Results
Fifty patients with OSAS (3 mild, 18 moderate, and 29 severe) and fifty volunteers were studied. There was no statistically significant difference in age, gender, visual acuity and refractive values between the groups. Baseline demographic characteristics of patients are shown in Table 1.
| OSAS group (n=50) | Control group (n=50) | P | |
|---|---|---|---|
| Age (year) | 49.2 ± 10.5 | 50.0 ± 8.7 | 0.68 |
| Sex (n, %) | |||
| Female | 16 (38.1%) | 26 (61.9%) | 0.06 |
| Male | 34 (58.6%) | 24 (41.4%) | |
| Visual acuity (snellen) | 0.96 ± 0.08 | 0.97 ± 0.1 | 0.67 |
| Refraction (D) (SE) | 0.64 ± 0.86 | 0.32 ± 0.96 | 0.19 |
OSAS: Obstructive Sleep Apnea Syndrome, SE: Spheric Equivalent, D: Diopter
Table 1: Demographic characteristics of Obstructive Sleep Apnea Syndrome (OSAS) and control groups
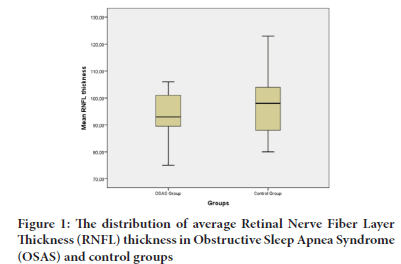
The mean RNFL thickness of the patients with OSAS were lower than the control group. However, this difference was not statistically signifi- cant. Figure 1 shows the distribution of average RNFL thickness in pa- tients and control group.
Figure 1: The distribution of average Retinal Nerve Fiber Layer Thickness (RNFL) thickness in Obstructive Sleep Apnea Syndrome (OSAS) and control groups
In addition, we found that the differences between the mean values of all quadrants RNFL thickness were similarly lower in OSAS group than in control groups. But this significance was not statistically different. Table 2 shows the mean RNFL thickness ( µ ) values in the groups. According to severity of disease there was no correlation was found between mean RNFL values and AHI (P=0.86, r=-0.02).
| RNFL thickness | OSAS group | Control group | |
|---|---|---|---|
| µm | (n=50) | (n=50) | P |
| Superior | 118.9 ± 13.1 | 128.6 ± 19.8 | 0.16 |
| Nasal | 71.7 ± 12.3 | 72.0 ± 10.7 | 0.89 |
| Inferior | 122.8 ± 16.8 | 125.9 ± 19.6 | 0.4 |
| Temporal | 63.7 ± 7.6 | 65.9 ± 10.6 | 0.35 |
| Average RNFL | 94.3 ± 8.7 | 96.5 ± 12.3 | 0.32 |
OSAS: Obstructive Sleep Apnea Syndrome, RNFL: Retinal Nerve Fiber Layer
Table 2: The mean Retinal Nerve Fiber Layer (RNFL) thickness ( µ ) values in the Obstructive Sleep Apnea Syndrome (OSAS) and control groups
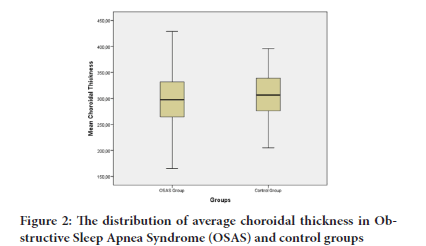
The RNFL thickness and GCC measurements were not statistically sig- nificant. The mean IOP, C/D ratio and vertical C/D ratio of the OSAS group significantly higher thought us there might be glaucome insid- ance higher in OSAS group. Table 3 shows optic nerve-related indica- tors in Obstructive Sleep Apnea Syndrome (OSAS) and control groups The subfoveal choroidal thickness of OSAS patients was 301.3 ± 56.1 µm and the control group was 305.3 ± 44.0 µm. There was not significant correlation was found between choroidal thickness and severity of disease according to AHI (p=0.9 r=-0.01). Figure 2 shows the distribu- tion of choroidal thickness in patients with OSAS and control group.
| OSAS group (n=50) | Control group (n=50) | P | |
|---|---|---|---|
| C\D | 0.45 ± 0.017 | 0.36 ± 0.02 | 0.022* |
| Vertical C\D | 0.43 ± 0.016 | 0.34 ± 0.019 | 0.012* |
| Average GCC | 84.2 ± 1 | 83.9 ± 1 | 0.79 |
| Minimum GCC | 81.4 ± 1.2 | 80.3 ± 1.2 | 0.53 |
| Mean IOP | 16.1 ± 1.37 | 15.2 ± 1.03 | 0.00* |
OSAS: Obstructive Sleep Apnea Syndrome, C\D: Cup\Disc ratio; GCC: Ganglion Cell Complex, IOP: Intraocular Pressure
*p<0.05
Table 3: Optic nerve-related indicators in Obstructive Sleep Apnea Syndrome (OSAS) and control groups
Figure 2: The distribution of average choroidal thickness in Obstructive Sleep Apnea Syndrome (OSAS) and control groups
Discussion
OSAS is a syndrome characterized by recurrent apnea or hypopnea episodes during sleep, and frequently decrease in blood oxygen sat- uration (SpO2). Optic disc damage can be occured by loss of ganglion cells. The hypoxia secondary to OSAS-induced imbalance between mediators; NO and endothelin can cause this ganglion cell loss (Tan CS, et al., 2012).
High IOP is the most important risk factor for the glaucoma. The high- er IOP causes a change in the ONH structures, especially makes RNFL thinning. A study by Karakucuk et al. (Stiefel P, et al., 2013) found that four patients have glaucome and the prevalence of glaucoma in OSAS patients was 12.9% (n=4/31). They also found a positive correlation between IOP and AHI. In our study we found that IOP values in OSAS group was significantly higher than in controls. IOP is important risk factor for glaucoma and glaucomatous ONH damage. At the same time there is no correlation between AHI groups.
Another important parameter is increase vertical cup/disk (C/D) ratio in glaucomatous optic nerve. A few studies were compared vertical C/D ratio between OSAS and control. Sergi et al. did not find any dif- ference in the cup/disk ratio between the OSAS patients and the con- trol group. They found a significant correlation between AHI and the cup/disk ratio (Karakucuk S, et al., 2008). In contrast with their study, our study shows that the vertical cup/disk ratio significantly higher in OSAS group than in controls without OSAS.
In glaucoma, RNFL thickness decreases progressively. This thinning can be present in eyes of patients with glaucoma before detectable changes occur in the visual field (Sergi M, et al., 2007; Kremmer S, et al., 2000). If a decrease in the RNFL can be detected, it gives an alert to the risk for developing glaucoma (Quigley HA, et al., 1989). Firstly Kargi et al. (Kargi SH, et al., 2005) were reported RNFL thickness decreases in patients with OSAS. Conversely, a study performed in Turkish popu- lation by Adam et al. (Adam M, et al., 2013) reported that there is no difference in RNFL thickness between healthy and OSAS subjects. An- other study by Ferrandez et al. (Ferrandez B, et al., 2016) reported that RNFL thickness did not differ significantly between OSAS and con- trol groups. Similarly in our study, we detected no correlation between OSAS patients and control group in RNFL parameters.
In addition to the measurement of peripapillary RNFL thickness by OCT, measurement of the macular Ganglion Cell Complex thickness has been used in several ocular and neurological diseases, particularly glaucoma. Ferrandez et al. (Ferrandez B, et al., 2016) showed that neither Ganglion Cell Layer (GCL) nor Ganglion Cell Inner Plexiform Layer (GC-IPL) thickness were reduced in OSAS patients compared with healthy controls. Conversely, Huseyinoglu et al. (Huseyinoglu N, et al., 2014) found GCL thickness decreases in patients with severe OSAS compared to the control group. In addition, there was a signifi- cant negative correlation between AHI and GCL thickness (Ferrandez B, et al., 2016). Kara (Kara N, et al., 2018) reported that the GC-IPL thickness in patients with severe OSAS was significantly lower than that of controls. In our study we found no significant correlation in GCL thickness between OSAS and control group.
The retina is metabolically very active tissue in the human body, and it has a double blood supply from the central retinal artery and the choroid. Certain characteristics of the choroid have been studied histo- logically. Spaide et al. (Spaide RF, et al., 2008) described a "Enhanced Deep Imaging" (EDI) technique to monitor the full thickness of the choroid and this optimize the parameters of OCT. Karalezli et al. (Karalezli A, et al., 2014) showed that the median choroidal thickness was statistically thinner in the eye of patients with severe OSAS than that of the controls. On the other hand, Tonini et al. (Tonini M, et al., 2010) reported that choroidal vascular response to hypoxia does not affected in the patients with OSAS. In a study Yuvaci et al. (Yuvaci I, et al., 2016) although differences in choroidal thickness were observed, no significant differences were found between the control group and the other OSAS groups. Similarly in our study although central chor- oidal thickness was thinner in OSAS group but data was not statis- tically significant.
The different results in several studies may be because of the calibra- tions of measuring instruments, the duration of OSAS, the demo- graphic characteristics of the participants, the vascular dysregulation present in patients with OSAS. In addition to these general factors, there are some limitations of our study and the major one is the limited sample of patients. A larger cohort study can give us more meaningful analysis on the relation between the severity of OSAS and posterior ocular findings. Another limitation was we were the exact timing of the development of OSAS was not known, which has a certain influence on the degree of hypoxia. The results of our study may be compared after long-term follow up and after CPAP treatment.
Conclusion
In summary we found that peripapillary RNFL, GCC, central chor- oidal thickness did not change with OSAS patients or the severity of OSAS. Furthermore, we found that IOP, C/D ratio and vertical C/D ratio of patients were all significantly higher than control group. These association between OSAS and glaucome supports the several previous studies. However, multicenter long-term cohort studies are still needed to assess the definite changes of RNFL thickness, GCC and CCT in OSAS patients.
References
- Guilleminault C. Clinical features and evaluation of Obstructive Sleep Apnea. Principles and practice of sleep medicine. 1994.
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of Obstructive Sleep Apnea: a population health perspective. Am J Respir Crit Care Med. 2002; 165(9): 1217-1239.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; 328(17): 1230-1235.
- Köktürk O. Epidemiology of sleep apnea syndrome. Tuberk Toraks. 1998; 46: 193-201.
- Caples SM, Garcia-Touchard A, Somers VK. Sleep-disordered breathing and cardiovascular risk. Sleep. 2007; 30(3): 291-303.
- Yuvaci I, Pangal E, Bayram N, Yüksel SA, Alabay B, Agadayi A, et al. Evaluation of posterior ocular changes using enhanced depth imaging-optical coherence tomography in patients with Obstructive Sleep Apnea Syndrome. Arq Bras Oftalmol. 2016; 79(4): 247-252.
- Arnaud C, Dematteis M, Pepin JL, Baguet JP, Lévy P. Obstructive Sleep Apnea, immuno-inflammation, and atherosclerosis. Semin Immunopathol. 2009; 31(1): 113-125.
- Jelic S, Le Jemtel TH. Inflammation, oxidative stress, and the vascular endothelium in Obstructive Sleep Apnea. Trends Cardiovasc Med. 2008; 18(7): 253-260.
- Khandgave TP, Puthran N, Ingole AB, Nicholson AD. The assessment of sleep apnoea as a risk factor in glaucoma. J Clin Diagn Res. 2013; 7(7): 1391.
- Bendel RE, Kaplan J, Heckman M, Fredrickson PA, Lin SC. Prevalence of glaucoma in patients with obstructive sleep apnoea-a cross-sectional case-series. Eye. 2008; 22(9): 1105-1109.
- Mojon DS, Hess CW, Goldblum D, Fleischhauer J, Koerner F, Bassetti C, et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999; 106(5): 1009-1012.
- Lin PW, Friedman M, Lin HC, Chang HW, Pulver TM, Chin CH. Decreased retinal nerve fiber layer thickness in patients with Obstructive Sleep Apnea/hypopnea syndrome. Graefes Arch Clin Exp Ophthalmol. 2011; 249(4): 585-593.
- Casas P, Ascaso FJ, Vicente E, Tejero-Garcés G, Adiego MI, Cristóbal JA. Retinal and optic nerve evaluation by optical coherence tomography in adults with Obstructive Sleep Apnea-Hypopnea Syndrome (OSAHS). Graefes Arch Clin Exp Ophthalmol. 2013; 251(6): 1625-1634.
- Maul EA, Friedman DS, Chang DS, Boland MV, Ramulu PY, Jampel HD, et al. Choroidal thickness measured by spectral domain optical coherence tomography: factors affecting thickness in glaucoma patients. Ophthalmology. 2011; 118(8): 1571-1579.
- Marcus DM, Costarides AP, Gokhale P, Papastergiou G, Miller JJ, Johnson MH, et al. Sleep disorders: a risk factor for normal-tension glaucoma?. J glaucoma. 2001; 10(3): 177-183.
- Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012; 53(1): 261-266.
- Stiefel P, Sánchez-Armengol MA, Villar J, Vallejo-Vaz A, Moreno-Luna R, Capote F. Obstructive Sleep Apnea Syndrome, vascular pathology, endothelial function and endothelial cells and circulating microparticles. Arch Med Res. 2013; 44(6): 409-414.
- Karakucuk S, Goktas S, Aksu M, Erdogan N, Demirci S, Oner A, et al. Ocular blood flow in patients with Obstructive Sleep Apnea Syndrome (OSAS). Graefes Arch Clin Exp Ophthalmol. 2008; 246(1): 129-134.
- Sergi M, Salerno DE, Rizzi M, Blini M, Andreoli A, Messenio D, et al. Prevalence of normal tension glaucoma in Obstructive Sleep Apnea Syndrome patients. J glaucoma. 2007; 16(1): 42-46.
- Kremmer S, Ayertey HD, Selbach JM, Steuhl KP. Scanning laser polarimetry, retinal nerve fiber layer photography, and perimetry in the diagnosis of glaucomatous nerve fiber defects. Graefes Arch Clin Exp Ophthalmol. 2000; 238(11): 922-926.
- Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989; 107(5): 453-464.
- Kargi SH, Altin R, Koksal M, Kart L, Cinar F, Ugurbas SH, et al. Retinal nerve fibre layer measurements are reduced in patients with obstructive sleep apnoea syndrome. Eye. 2005; 19(5): 575-579.
- Adam M, Okka M, Yosunkaya S, Bozkurt B, Kerimoglu H, Turan M. The evaluation of retinal nerve fiber layer thickness in patients with Obstructive Sleep Apnea Syndrome. J ophthalmol. 2013; 2013.
- Ferrandez B, Ferreras A, Calvo P, Abadia B, Marin JM, Pajarin AB. Assessment of the retinal nerve fiber layer in individuals with Obstructive Sleep Apnea. BMC ophthalmol. 2016; 16(1): 1-7.
- Ferrandez B, Ferreras A, Calvo P, Abadia B, Pajarin AB, Marin JM, et al. Macular retinal ganglion cell layer thickness is not reduced in patients with Obstructive Sleep Apnea. Ophthalmic Res. 2016; 56(2): 85-91.
- Huseyinoglu N, Ekinci M, Ozben S, Buyukuysal C, Kale MY, Sanivar HS. Optic disc and retinal nerve fiber layer parameters as indicators of neurodegenerative brain changes in patients with Obstructive Sleep Apnea Syndrome. Sleep Breath. 2014; 18(1): 95-102.
- Kara N, Sayin N, Bayramoglu SE, Savas AU. Peripapillary retina nerve fiber layer thickness and macular ganglion cell layer thickness in patients with Obstructive Sleep Apnea Syndrome. Eye. 2018; 32(4): 701-706.
- Spaide RF, Koizumi H, Pozonni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008; 146(4): 496-500.
- Karalezli A, Eroglu FC, Kivanc T, Dogan R. Evaluation of choroidal thickness using spectral-domain optical coherence tomography in patients with severe Obstructive Sleep Apnea Syndrome: a comparative study. Int J Ophthalmol. 2014; 7(6): 1030.
- Tonini M,, Khayi H, Pepin JL, Renard E, Baguet JP, Lévy P, et al. Choroidal blood-flow responses to hyperoxia and hypercapnia in men with Obstructive Sleep Apnea. Sleep. 2010; 33(6): 811-818.
Author Info
Ela Eren1*, Nilüfer Ilhan2 and Sebahat Genç32Department of Ophthalmology, Mustafa Kemal University Medical Hospital, Hatay, Turkey
3Department of Chest Medicine, Mustafa Kemal University Medical Hospital, Hatay, Turkey
Received: 25-May-2021 Accepted: 07-Jun-2021 Published: 14-Jun-2021
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 ┬╗ doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 ┬╗ doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to ŌĆ£Healthcare for AllŌĆØ Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 ┬╗ doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 ┬╗ doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 ┬╗ doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 ┬╗ doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 ┬╗ doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to ŌĆ£Healthcare for AllŌĆØ Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 ┬╗ doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 ┬╗ doi: 10.5530/srp.2019.1.3