Review Article - (2023) Volume 14, Issue 6
Abstract
This review article provides an overview of the use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) in orthopedics, including their pharmacology, efficacy, safety, use in various ortho-related conditions, and potential adverse effects. In orthopedic departments, NSAIDs are frequently prescribed to treat pain and inflammation caused by a variety of disorders such as osteoarthritis, rheumatoid arthritis, acute injuries, bursitis, tendonitis, gout, lower back pain, and surgeries. NSAIDs work by inhibiting the enzymes that produce prostaglandins, which are mediators of pain and inflammation. Though generally safe and effective, NSAIDs have major concerns over their potential side effects such as Gastro-Intestinal (GI) complications, cardiovascular complications, renal toxicity, and impairment in bone healing. This article explores the basic pharmacology of NSAIDs and the safety profile of NSAIDs in orthopedics, including the potential risks associated with their use. The article concludes that while NSAIDs are considered safe, there are potential risks associated with their use, and clinicians should carefully consider the risks and benefits of NSAID therapy and take steps to mitigate potential adverse effects.
Keywords
Osteoarthritis, Rheumatoid arthritis, Gout, Lower back pain, Pain, Inflammation
Introduction
In orthopedic medication, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are the most commonly used for the treatment of pain and inflammation and other variety of conditions like osteoarthritis, rheumatoid arthritis, acute injuries, bursitis, tendinitis, gout, lower back pain and for surgeries as well (Santander-Pérez PA, et al., 2023). NSAIDs work by inhibiting the enzymes that produce prostaglandins which are the mediators of pain and inflammation. Though NSAIDs are generally safe and effective, there are major concerns on their potential side effects like increase in perioperative bleeding in surgical conditions (Santander-Pérez PA, et al., 2023) and GI complications. NSAIDs can irritate the lining of the stomach and intestines, increasing the risk of ulceration in stomach, bleeding, and perforation etc., (Lanas A and Sopeña F, 2009). NSAIDS may also increase CVS complications including heart attack, stroke. Further, a meta-analysis study found that using NSAIDS for longer duration is associated with 40% increased of above conditions compared to non-NSAIDs users (Trelle S, et al., 2011) and renal toxicity including impaired kidney function (Srisawat N and Johnson RJ, 2009), predominantly in patients with history of renal disease or in patients or individuals using other nephrotoxic medications for a prolonged period. Some of the studies with NSAIDS have shown long-term use of the drug might result in impairment of bone healing during fractured conditions particularly with long-term use of that medication. This review article aims to provide an overview of the use of NSAIDs in orthopedics, including their pharmacology, efficacy, safety, use in various ortho related conditions and potential adverse effects.
Literature Review
General pharmacology
NSAIDS, are among the most prescribed medications in the population with ortho-related issues due to its analgesic as well as anti-inflammatory properties (Santander-Pérez PA, et al., 2023). The pharmacology or the mechanism of NSAIDS is simple and it involves the direct inhibition of Cyclooxygenase (COX) enzyme, responsible for the production of anti-inflammatory mediators (Trelle S, et al., 2011; Zhang W, et al., 2008) such as prostaglandins (performs important physiological processes in the body such as platelet aggregation, vasodilation, and bronchoconstriction), thromboxane (a powerful vasoconstrictor and platelet aggregation promoter), prostacyclin (also known as PGI2, and prostaglandin I2 which is a powerful vasodilator and platelet aggregation inhibitor) (Figure 1 and Table 1).
| Class of drug | Sub classes | Examples |
|---|---|---|
| Non selective COX inhibitors | Salicylates | Aspirin |
| Acetic acid derivatives | Ketorolac, indomethacin, nabumetone | |
| Pyrazolone derivatives | Phenylbutazone, oxyphenbutazone | |
| Propionic acid derivatives | Ibuprofen, naproxen, ketoprofen, fluriprofen | |
| Fenamates | Mephenamic acid | |
| Enolic acid derivatives | Piroxicam, tinoxicam | |
| Preferentially COX-2 inhibitors | - | Nimesulide, diclofenac, aceclofenac, meloxicam, etodolac |
| Selective COX-2 inhibitors | - | Celecoxib, etoricoxib, parecoxib |
| Analgesic-antipyretic with poor anti-inflammatory action | Para aminophenol derivatives | Paracetamol (Acetaminophen) |
| Pyrazolone derivatives | Metamizol (Dipyrone), propyphenazone | |
| Benzoxazocine derivatives | Nefopam |
Table 1: Classification of NSAIDS
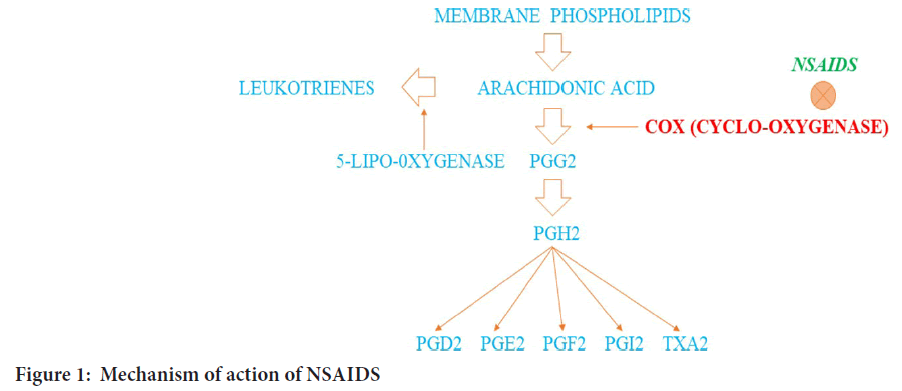
Figure 1: Mechanism of action of NSAIDS
There are two isoforms of COX enzymes (COX-1 and COX-2). Fundamentally, COX-1 is expressed in tissues across numerous systems and is involved in the production of prostaglandins (regulator of various physiological processes, including gastric cyto-protection and platelet aggregation). COX-2, functions alternatively by induction of response to pro-inflammatory stimuli and leads to the production of prostaglandins, resulting in reducing pain, inflammation and fever. Since COX-1 is responsible for the maintenance of gastric mucosal integrity and platelet aggregation, COX-1 inhibition can result in unintended side effects, such as gastric ulcers, bleeding etc. NSAIDs like celecoxib (selectively inhibit COX-2), reduce the risk of gastrointestinal complications like ulceration of the stomach, GI bleeding. However, selective inhibitors of COX-2 have been linked with an increased risk of cardiac events (Trelle S, et al., 2011), which has led to the withdrawal of some of these agents from the market. NSAIDs are available in various formulations (oral tablets, capsules, liquids, as well as topical gels and patches) and the choice of NSAID and route of administration will depend on that specific condition being treated, the severity of symptoms, as well as the individual patient factors.
Indication for NSAIDS in orthopedic practice
• Treatment of inflammation-related, acute pain.
• Treatment of inflammatory chronic pains, such as rheumatoid arthritis, osteoarthritis, and ankylosing spondylitis.
• Suppression of inflammation and its related edema.
• Treatment of soft tissue rheumatism.
• The management of febrile illnesses and acute infections.
• Myositis ossificans prevention, management, and therapy.
• Treatment for post-operative pain, metastatic bone disease, and other cancers.
• Thromboembolic phenomenon will be prevented on the arterial side of the vasculature.
• Neuritis, lumbago and myalgias.
Safety and efficacy
NSAIDs are considered safe, but there are potential risks associated with their use, one of those major risks associated with NSAID use is GI complications (bleeding, perforation, and ulceration). Based on a systematic review and meta-analysis utilization of NSAIDs is linked with a greater risk of GI complications, particularly in geriatric patients and individuals with a known history of GI disorders (Hawkey CJ, 1999; Lanas A, et al., 2017). Another potential risk of NSAID use is renal toxicity. Long-term use of NSAIDs increases the risk of developing chronic renal disease and can worsen the condition of acute kidney injury. According to Gill SS, et al., 2014 study, people who have undergone orthopedic surgery and have used NSAIDs for a long time are at an elevated risk of suffering an acute renal injury. The bone healing process can also be affected with the use of NSAIDs. Some studies suggest that NSAIDs can delay or impair bone healing, particularly in long bone fractures (Simon AM, et al., 2018). However, the evidence is conflicting, and more researches are needed to clarify the relationship between bone healing and use of NSAIDs. The major risks associated with NSAIDs use (GI complications, renal toxicity etc.,) can be mitigated by appropriate patient selection, appropriate dosing regimens, and close monitoring. In addition, the use of lower doses and shorter treatment durations may reduce the risk of adverse effects. Due to the rise of possible side effects encountered using NSAID, clinicians (or) the prescribers should carefully consider the risks and benefits of NSAID therapy and take steps to mitigate potential adverse effects linked with the treatment of NSAIDs.
In orthopedic practice, NSAIDs are frequently utilized due to their analgesic and anti-inflammatory properties. Osteoarthritis, rheumatoid arthritis, tendinitis, bursitis, and other orthopedic disorders are thought to be helped by NSAIDs in terms of lowering pain and inflammation. In patients with osteoarthritis of the knee and hip, NSAIDs were beneficial in lowering pain and enhancing function, according to a meta-analysis study by da Costa BR, et al., 2017. The study included 74 randomized controlled trials involving over 58,000 patients and found that NSAIDs were more effective than placebo in reducing pain and improving function in patients with osteoarthritis. NSAIDs have also been shown to be effective in the management of acute musculoskeletal pain. A randomized controlled trial found that ibuprofen (a commonly used NSAID), was more effective than placebo in reducing pain and improving function in patients with acute low back pain (Friedman BW, et al., 2015). In addition to their analgesic and anti-inflammatory effects, NSAIDs have been shown to have other benefits in orthopedic patients. According to Hawker GA, et al., 2015 NSAIDs decrease the likelihood of joint replacement surgery in those with osteoarthritis of the knee. The study included over 4,000 patients with knee osteoarthritis and found that NSAID use was associated with a reduced risk of joint replacement surgery over a 7-year follow-up period. In summary, NSAIDs work excellently to reduce pain and inflammation in variety of orthopedic problems.
Discussion
NSAIDs and osteoarthritis
Osteoarthritis (OA) is a degenerative joint disorder in which the synovial joint fails as a result of osteophyte growth, meniscal injury, ligamentous laxity, and subchondral bone alterations (Bennell KL, et al., 2012). Even though the non-pharmacological treatments are given the priority, analgesics play an important role in managing the painful conditions of OA. As first- or second-line treatments for patients with symptomatic OA, current practice guidelines encourage the use of a mild analgesic, such as acetaminophen (paracetamol), or a NSAID, administered either systemically or topically (Bannwarth B, 2006). The COX enzyme, which catalyzes the conversion of arachidonic acid to prostaglandins and thromboxane, is inhibited by NSAIDs (Barger BK, et al., 2020). The main adverse effect of NSAIDs is gastrointestinal toxicity (McGettigan P and Henry D, 2006). Compared to nonselective oral NSAIDs, meloxicam and naproxen combined with lansoprazole have a lower risk of adverse GI events (Hawkey C, et al., 1998). And use of topical NSAIDs like diclofenac gels, patches show to produce more efficacy with lesser toxicity (Rainsford KD, et al., 2008). Studies show that NSAIDs increase matrix synthesis and protect chondrocytes against apoptosis and regain the articular cartilage function (Mastbergen SC, et al., 2005).
NSAIDs and rheumatoid arthritis
The synovial membrane is inflamed in Rheumatoid Arthritis (RA), a chronic systemic autoimmune inflammatory disease that causes bone erosion, gradual degradation of articular cartilage, and other abnormalities (Guo Q, et al., 2018). The Major Histocompatibility Complex (MHC) II genetic polymorphism is the primary risk factor for developing RA (Nepom GT, et al., 1998). Joint pain, edema, and stiffness in the upper and lower extremities are symptoms of RA. More than five joints are typically involved, both sides of the body are affected and tiny joints in the wrists, hands, and feet are its preferred targets (Rau R, et al., 1998). Reduced joint pain and inflammation, improved joint function, and prevention of additional joint damage are the main objectives of RA therapy (Bullock J, et al., 2019). Non-steroidal anti-inflammatory medications (NSAIDs), corticosteroids, Disease-Modifying Anti-Rheumatic Drugs (DMARDs), and biological DMARDs are being utilized to treat RA in order to prevent joint deterioration (Singh JA, et al., 2016). The topical administration of NSAIDs such as diclofenac sodium, methyl salicylate increases local drug delivery to affected tissues with reduced systemic side effects (Jurca T, et al., 2020). NSAIDs are pretty much showing greater improvement in the diseased condition of RA due to their analgesic and anti-inflammatory properties also it is a cost effective treatment which can be afforded by wide range of population (Berner G, et al., 1989).
NSAIDs and musculoskeletal pain
Musculoskeletal pain includes wide range of disorders from ligament injuries to intra-articular disorders which affects the quality of life (Galer BS, et al., 2004). Pain is a complicated sensory experience linked to real or potential tissue injury (Basbuam AI, 1991). These conditions are very common but they affect the individual lifestyle as well as the society (Horton R, 2012). The most widely used medication for the treatment of musculoskeletal pain are NSAIDs because of their availability and ease of use (Atchison JW, et al., 2013). Because NSAIDs have become more effective at managing both acute and long-term musculoskeletal pain (Stanos SP, 2007), diclofenac gel is emerged as the mostly used topical NSAID for the treatment of musculoskeletal pain (Zimmerman J, et al., 1995).
NSAIDs and fracture healing
Fracture healing is a complicated process that involves numerous concurrent and follow-up cellular and molecular actions. Aspects of the healing process include the production of hematomas, inflammation, bone repair with the development of a soft and hard callus through intramembranous and endochondral bone formation, and bone remodeling (Grohs JG, et al., 2007). Prostaglandin E2 (PGE2) is commonly found in bone (Kawaguchi H, et al., 1995). When a bone is damaged there is an increased synthesis of both endogenous and exogenous prostaglandins, here only the endogenous prostaglandins support the fracture healing as the NSAIDs inhibit the synthesis of exogenous prostaglandins (Norrdin RW, et al., 1990). The ability of NSAIDs in inhibiting exogenous prostaglandins is clear and undisputed (Murnaghan M, et al., 2006). Hence use of NSAIDs after a fracture shows better improvement in pain and facilitates fracture healing (Geusens P, et al., 2013).
NSAIDs and gout
Gout is a kind of inflammatory arthritis caused by a malfunction in the metabolism of uric acid, which leads to the deposition of monosodium urate crystals in the joints and soft tissues (Star VL and Hochberg MC, 1994). The major focus of treatment needs to be aimed at monosodium urate crystal dissolution (Perez‐Ruiz F, et al., 2002). Effective therapy is necessary since gout flares are painful and incapacitating. Acute flares are treated with glucocorticoids, colchicine, and NSAIDs (Terkeltaub RA, et al., 2010). NSAIDs effectiveness in treating acute gout flares is similar to most agents which are available for the treatment of gout flare-ups (Schumacher Jr HR, et al., 2002). Compared to nonselective NSAIDs, COX-2-selective inhibitors can also effectively relieve pain while having superior gastrointestinal tolerability (Kim KY, et al., 2003). Indomethacin 50 mg for every six hours, then 50 mg for every eight hours; naproxen 500 mg for every eight hours, then 500 mg for every twelve hours; or piroxicam 40 mg for every twelve hours, then 20 mg for every 1 hour would be the recommended doses starting amounts. Most medications became clinically effective after 1 to 3 days of initial treatment (Fam AG, 1990). NSAIDs are crucial for treating acute gout, especially in patients who are having trouble responding to other treatments.
NSAIDs and orthopedic surgeries
NSAIDs are the most predominantly used class of drugs in management of pain during orthopedic surgeries for their analgesic and anti-inflammatory properties. They have been found to be effective in reducing pain, inflammation, and swelling in the postoperative period by inhibiting the action of Cyclooxygenase (COX) enzymes (American college of surgeons, 2018). NSAIDs are often used in combination with other pain management techniques such as opioids, physical therapy, and ice therapy to provide optimal pain relief after surgery. However, the use of NSAIDs in orthopedic surgeries has been a subject of debate due to concerns regarding their potential adverse effects, especially in relation to bone healing (Moukharskaya J and Verschraegen C, 2012). A study conducted to assess the effect of NSAID use on bone healing after orthopedic surgeries. The study found that NSAID use did not have a significant impact on the rate of bone healing or the incidence after orthopedic surgeries. The study concluded that the use of NSAIDs in the postoperative period was safe and did not impair bone healing (Wu K, et al., 2021). Another study conducted to assess the efficacy of different pain management strategies after orthopedic surgeries. The study found that a combination of NSAIDs and opioids provided superior pain relief compared to opioids alone. However, the study also highlighted the potential adverse effects of NSAIDs, including gastrointestinal bleeding and renal dysfunction (Perez-Ruiz F, et al., 2000).
Despite the potential adverse effects, the use of NSAIDs in orthopedic surgeries remains a common practice due to their effectiveness in pain management. Orthopedic surgeons must carefully consider the risks and benefits of NSAID use and compare them against other pain management strategies. In summary, NSAIDs play a vital role in the management of pain and inflammation after orthopedic surgeries. While concerns regarding their potential adverse effects on bone healing exist, current evidence suggests that NSAIDs are safe to use in the postoperative period. Orthopedic surgeons must carefully evaluate the risks and benefits of NSAID use in each patient and consider alternative pain management strategies if necessary.
Conclusion
In orthopaedics, NSAIDs are the most often recommended class of drugs. They are an invaluable resource for any healthcare professionals who treat pain caused by inflammation, which involves the inhibition of COX enzymes and are responsible for the production of prostaglandins involved in pain and inflammation. The safety profile of NSAIDs is a concern, particularly in geriatric patients and those with pre-existing gastrointestinal and renal disorders. NSAIDs can also impair bone healing, although the evidence is conflicting. The risks associated with use of NSAIDs can be mitigated by appropriate patient selection, dosing regimens, and close monitoring. Clinicians and prescribers must consider the risks and benefits of NSAID therapy carefully and take steps to minimize potential adverse effects. Due to their analgesic and anti-inflammatory effects, non-steroidal anti-inflammatory medicines (NSAIDs) play a crucial role in treating a variety of musculoskeletal illnesses. The most recent practice guidelines have encouraged using NSAIDs as a first- or second-line treatment for symptomatic rheumatoid arthritis and osteoarthritis. Topical NSAIDs have shown more efficacy with lesser toxicity compared to oral NSAIDs. Moreover, NSAIDs have been proven to be effective in treating musculoskeletal pain and fracture healing. Acute flare-ups of gout are treated with NSAIDs, and COX-2 selective inhibitors offer efficient pain relief with superior gastrointestinal tolerability. However, the main adverse effect of NSAIDs is gastrointestinal toxicity, and physicians should be careful while prescribing NSAIDs to patients with a history of gastrointestinal disorders. Overall, when administered properly, NSAIDs can significantly reduce pain and raise the quality of life for those with musculoskeletal illnesses.
Acknowledgement
I would like to extend my sincere thanks to all the authors whose works were referenced in this article review. Your contributions have been invaluable, and without them, this review would not have been possible.
References
- Santander-Pérez PA, Ceschin ÁP, Ramos AA, Nisihara R, Junior JK. Serum concentrations of progesterone and prolactin as predictors of success in in vitro fertilization: A retrospective cohort study. JBRA Assist Reprod. 2023; 27(1): 71.
[Crossref] [Google Scholar] [Pubmed]
- Lanas A, Sopeña F. Nonsteroidal anti-inflammatory drugs and lower gastrointestinal complications. Gastroenterol Clin North Am. 2009; 38(2): 333-352.
[Crossref] [Google Scholar] [Pubmed]
- Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: Network meta-analysis. BMJ. 2011; 342.
[Crossref] [Google Scholar] [Pubmed]
- Srisawat N, Johnson RJ. Association of cyclo-oxygenase-2 inhibitors with increased risk of acute kidney injury: A meta-analysis of randomized controlled trials. Nephrol Dial Transplant. 2009; 24(10): 3159-3167.
- Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008; 16(2): 137-162.
[Crossref] [Google Scholar] [Pubmed]
- Hawkey CJ. COX-2 inhibitors. Lancet. 1999; 353(9149): 307-314.
[Crossref] [Google Scholar] [Pubmed]
- Lanas A, Chan FK, Scheiman J. GI and cardiovascular risks of NSAIDs: A systematic review and meta-analysis. Br J Clin Pharmacol. 2017; 82(4): 957- 968.
- Gill SS, Khunti K, Land M. Perioperative NSAIDs and acute kidney injury in patients undergoing orthopaedic surgery. J Bone Jt Surg. 2014; 96(9): 679-686.
- Simon AM, Manigrasso MB, O'Connor JP. The relationship between NSAIDs and delayed bone healing: A systematic review. J Orthop Trauma. 2018; 32(6): 293-299.
- da Costa BR, Reichenbach S, Keller N, Nartey L, Wandel S, Jüni P, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: A network meta-analysis. Lancet. 2017; 390(10090): e21-e33.
[Crossref] [Google Scholar] [Pubmed]
- Friedman BW, Dym AA, Davitt M, Holden L, Solorzano C, Esses D, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: A randomized clinical trial. JAMA. 2015; 314(15): 1572-1580.
[Crossref] [Google Scholar] [Pubmed]
- Hawker GA, Croxford R, Bierman AS. Use of nonsteroidal anti-inflammatory drugs in patients with knee osteoarthritis and the risk of knee replacement surgery: A population-based, case-control study. Arthritis Res Ther. 2015; 17: 371.
- Bennell KL, Hunter DJ, Hinman RS. Management of osteoarthritis of the knee. BMJ. 2012; 345.
[Crossref] [Google Scholar] [Pubmed]
- Bannwarth B. Acetaminophen or NSAIDs for the treatment of osteoarthritis. Best Pract Res Clin Rheumatol. 2006; 20(1): 117-129.
- Barger BK, Bisges AM, Fox DB, Torres B. Low-level laser therapy for osteoarthritis treatment in dogs at missouri veterinary practice. J Am Anim Hosp Assoc. 2020; 56(3): 139-145.
[Crossref] [Google Scholar] [Pubmed]
- McGettigan P, Henry D. Cardiovascular risk and inhibition of cyclooxygenase: A systematic review of the observational studies of selective and nonselective inhibitors of cyclooxygenase 2. JAMA. 2006; 296(13): 1633-1644.
[Crossref] [Google Scholar] [Pubmed]
- Hawkey C, Kahan A, Steinbrück K, Alegre C, Baumelou E, Begaud B, et al. Gastrointestinal tolerability of meloxicam compared to diclofenac in osteoarthritis patients. International MELISSA Study Group. Meloxicam Large-scale International Study Safety Assessment. Br J Rheumatol. 1998; 37(9): 937-945.
[Crossref] [Google Scholar] [Pubmed]
- Rainsford KD, Kean WF, Ehrlich GE. Review of the pharmaceutical properties and clinical effects of the topical NSAID formulation, diclofenac epolamine. Curr Med Res Opin. 2008; 24(10): 2967-2992.
[Crossref] [Google Scholar] [Pubmed]
- Mastbergen SC, Jansen NW, Bijlsma JW, Lafeber FP. Differential direct effects of cyclo-oxygenase-1/2 inhibition on proteoglycan turnover of human osteoarthritic cartilage: An in vitro study. Arthritis Res Ther. 2005; 8: 1-9.
[Crossref] [Google Scholar] [Pubmed]
- Guo Q, Wang Y, Xu D, Nossent J, Pavlos NJ, Xu J. Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018; 6(1): 15.
[Crossref] [Google Scholar] [Pubmed]
- Nepom GT. Major histocompatibility complex-directed susceptibility to rheumatoid arthritis. Adv Immunol. 1998; 68: 315-332.
[Crossref] [Google Scholar] [Pubmed]
- Rau R, Wassenberg S, Herborn G, Stucki G, Gebler A. A new method of scoring radiographic change in. J Rheumatol. 1998: 25.
[Google Scholar] [Pubmed]
- Bullock J, Rizvi SA, Saleh AM, Ahmed SS, Do DP, Ansari RA, et al. Rheumatoid arthritis: A brief overview of the treatment. Med Princ Pract. 2019; 27(6): 501-507.
[Crossref] [Google Scholar] [Pubmed]
- Singh JA, Saag KG, Bridges Jr SL, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American college of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2016; 68(1): 1-26.
[Crossref] [Google Scholar] [Pubmed]
- Jurca T, Józsa L, Suciu R, Pallag A, Marian E, Bácskay I, et al. Formulation of topical dosage forms containing synthetic and natural anti-inflammatory agents for the treatment of rheumatoid arthritis. Molecules. 2020; 26(1): 24.
[Crossref] [Google Scholar] [Pubmed]
- Berner G, Engels B, Vögtle-Junkert U. Percutaneous ibuprofen therapy with trauma-dolgit gel: Bioequivalence studies. Drugs Exp Clin Res. 1989; 15(11-12): 559-564.
[Crossref] [Google Scholar] [Pubmed]
- Galer BS, Gammaitoni AR, Oleka N, Jensen MP, Argoff CE. Use of the lidocaine patch 5% in reducing intensity of various pain qualities reported by patients with low-back pain. Curr Med Res Opin. 2004; 20(sup2): S5-12.
[Crossref] [Google Scholar] [Pubmed]
- Basbuam AI. The perception of pain. Principles of Neural Science. 1991: 472-491.
- Horton R. GBD 2010: Understanding disease, injury, and risk. Lancet. 2012; 380(9859): 2053-2054.
[Crossref] [Google Scholar] [Pubmed]
- Atchison JW, Herndon CM, Rusie E. NSAIDs for musculoskeletal pain management: current perspectives and novel strategies to improve safety. J Manag Care Pharm. 2013; 19(9 Supp A): 1-9.
[Crossref] [Google Scholar] [Pubmed]
- Stanos SP. Topical agents for the management of musculoskeletal pain. J Pain Symptom Manage. 2007; 33(3): 342-355.
[Crossref] [Google Scholar] [Pubmed]
- Zimmerman J, Siguencia J, Tsvang E. Upper gastrointestinal hemorrhage associated with cutaneous application of diclofenac gel. Am J Gastroenterol. 1995; 90(11).
[Google Scholar] [Pubmed]
- Grohs JG, Schmidt M, Wanivenhaus A. Selective COX-2 inhibitor versus indomethacin for the prevention of heterotopic ossification after hip replacement: A double-blind randomized trial of 100 patients with 1-year follow-up. Acta Orthop. 2007; 78(1): 95-98.
[Crossref] [Google Scholar] [Pubmed]
- Kawaguchi H, Pilbeam CC, Harrison JR, Raisz LG. The role of prostaglandins in the regulation of bone metabolism. Clin Orthop Relat Res. 1995; 313: 36-46.
[Google Scholar] [Pubmed]
- Norrdin RW, Jee WS, High WB. The role of prostaglandins in bone in vivo. Prostaglandins Leukot Essent Fatty Acids. 1990; 41(3): 139-149.
[Crossref] [Google Scholar] [Pubmed]
- Murnaghan M, Li G, Marsh DR. Nonsteroidal anti-inflammatory drug-induced fracture nonunion: An inhibition of angiogenesis? J Bone Joint Surg Am. 2006; 88(suppl_3): 140-147.
[Crossref] [Google Scholar] [Pubmed]
- Geusens P, Emans PJ, de Jong JJ, van den Bergh J. NSAIDs and fracture healing. Curr Opin Rheumatol. 2013; 25(4): 524-531.
[Crossref] [Google Scholar] [Pubmed]
- Star VL, Hochberg MC. Gout: Steps to relieve acute symptoms, prevent further attacks. Consultant. 1994; 34(12): 1697-1704.
- Perez‐Ruiz F, Calabozo M, Pijoan JI, Herrero‐Beites AM, Ruibal A. Effect of urate‐lowering therapy on the velocity of size reduction of tophi in chronic gout. Arthritis Rheum. 2002; 47(4): 356-360.
[Crossref] [Google Scholar] [Pubmed]
- Terkeltaub RA, Furst DE, Bennett K, Kook KA, Crockett RS, Davis MW. High versus low dosing of oral colchicine for early acute gout flare: Twenty‐four-hour outcome of the first multicenter, randomized, double‐blind, placebo‐controlled, parallel‐group, dose‐comparison colchicine study. Arthritis Rheum. 2010; 62(4): 1060-1068.
[Crossref] [Google Scholar] [Pubmed]
- Schumacher Jr HR, Boice JA, Daikh DI, Mukhopadhyay S, Malmstrom K, Ng J, et al. Randomised double blind trial of etoricoxib and indometacin in treatment of acute gouty arthritis. BMJ. 2002; 324(7352): 1488-1492.
[Crossref] [Google Scholar] [Pubmed]
- Kim KY, Schumacher HR, Hunsche E, Wertheimer AI, Kong SX. A literature review of the epidemiology and treatment of acute gout. Clin Ther. 2003; 25(6): 1593-1617.
[Crossref] [Google Scholar] [Pubmed]
- Fam AG. Strategies and controversies in the treatment of gout and hyperuricaemia. Baillieres Clin Rheumatol. 1990; 4(2): 177-192.
[Crossref] [Google Scholar] [Pubmed]
- American college of surgeons. Pain management in the surgical patient: A review of current best practices. Bull J Am Coll Surg. 2018; 103(5): 25-32.
- Moukharskaya J, Verschraegen C. Topoisomerase 1 inhibitors and cancer therapy. Hematol Oncol Clin North Am. 2012; 26(3): 507-525.
[Crossref] [Google Scholar] [Pubmed]
- Wu K, Chen K, Chen P. Non-steroidal anti-inflammatory drugs and bone healing after orthopedic surgery: A systematic review and meta-analysis. J Orthop Surg Res. 2021; 16(1): 1-11.
- Perez-Ruiz F, Gonzalez Mielgo FJ, Herrero-Beites AM. Optimisation of the treatment of acute gout. BioDrugs. 2000; 13: 415-423.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Julliyan Dilleban*, Thenraja and SundaresanCitation: Systematic Review Pharmacy Dilleban J: Role of Non-Steroidal Anti-Inflammatory Drugs in Orthopedics
Received: 12-May-2023 Accepted: 26-May-2023 Published: 02-Jun-2023, DOI: 10.31858/0975-8453.14.6.375-379
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






