Research Article - (2023) Volume 14, Issue 4
Abstract
Objective: The purpose of this study is to evaluate the effectiveness of acupuncture therapy for patients with insomnia and functional gastrointestinal diseases.
Methods: PubMed, EMBASE, the Cochrane Library, Web of science, China National Knowledge Infrastructure (CNKI), Wanfang Database, China Science Technology Journal Database, SinoMed Database were searched to identify eligible Randomized Controlled Trials (RCTs). Screening documents, data extraction, quality assessment of methodology and quality assessment of evidence were also conducted by two authors separately at the same time. The results of meta-analysis were made via Rev Man software (5.3).
Results: We included 9 RCTs (984 participants), meeting the inclusion and exclusion criteria. The results of meta-analysis demonstrated about sleep effect, compared with the western medicine group, the Pittsburgh Sleep Quality Index (PSQI) score of the acupuncture group was lower than that of the western medicine group (MD-2.60, 95% CI (-4.95,-0.25), I2=96%, n=526, 4 trials). Compared with acupuncture group, the PSQI score of acupuncture combined with Tui Na group was lower than that of acupuncture group (MD-2.49, 95% CI (-2.66,-2.32), I2=14%, n=458, 5 trials). It also discussed about gastrointestinal function, only 1 RCT reported gastrointestinal-related indicators and the results showed that the acupuncture group effect was better than western medicine group in regulating the level of brain-gut peptide.
Conclusion: Acupuncture and acupuncture combined with Tui Na can both improve the sleep quality of patients with insomnia and functional gastrointestinal diseases, and the efficacy of acupuncture combined with Tui Na is better than that of acupuncture alone. However, it is not clear whether it can improve gastrointestinal symptoms. More high-quality clinical trials are needed to provide more powerful and comprehensive evidence in the future.
Keywords
Acupuncture, Tui Na, Insomnia, Functional gastrointestinal diseases
Introduction
Insomnia refers to a subjective experience of dissatisfaction with sleep time and/or quality, despite proper sleeping opportunities and sleeping environment, characterized by falling asleep and sleep maintenance disorders, and abnormal daytime social functions (Sleep Disorder Society, 2012; American Psychiatric Association, 2013). About one third of adults have insomnia symptoms, and 45.5% subjects in China have experienced different degrees of insomnia (Sleep Disorder Society, 2012; American Psychiatric Association, 2013; Soldatos CR, et al., 2005). Insomnia increases the risk of many health problems, for example cardiovascular diseases (Li M, et al., 2014), obesity and diabetes (Anothaisintawee T, et al., 2016; Chan WS, et al., 2018), depression and anxiety (Hertenstein E, et al., 2019) and functional gastrointestinal diseases (Andreev DN, et al., 2021; Wang B, et al., 2018) and etc. Thus, insomnia brings about a heavy burden to individual and society.
Functional Gastrointestinal Disorders (FGIDs) are a kind of non-organic diseases characterized by the presence of chronic and recurrent gastrointestinal symptoms (Drossman DA and Hasler WL, 2016; Black CJ, et al., 2020). FGIDs are mainly represented by Irritable Bowel Syndrome (IBS), Functional Constipation (FC) and Functional Dyspepsia (FD). From the most recent global epidemiology study, an estimated 40% of the world population suffer from FGIDs (Sperber AD, et al., 2021), and the prevalence rate in China is 34.4%, which affects the life quality of people and increases the medical burden (Sperber AD, et al., 2021).
The comorbidity of insomnia and functional gastrointestinal diseases is widespread. Many insomnia patients have Functional Gastrointestinal Disorders, and insomnia is also often found in patients with functional gastrointestinal disease usually (Hyun MK, et al., 2019; Lei WY, et al., 2019), which is also mentioned in the classic book Huangdi Neijing (The Yellow Emperor’s Canon of Internal Medicine) “stomach disharmony leading to restless sleep” in thousands of years ago (Tian DH, 2005).
As for the comorbidity of insomnia and functional gastrointestinal diseases, modern medicine study also provides a theoretical basis through the understanding of Brain-Gut Axis (BGA) (Tait C and Sayuk GS, 2021). The BGA dysfunction may be the pathological basis and the brain-gut peptides such as 5-Hydroxytryptamine (5-HT) is the material basis of patients with insomnia and FGIDs (Jiang W and Wang CJ, 2021). Until now, there is no consensus on the effective treatment for patients with insomnia and FGIDs. At present, the clinical methods for patients with insomnia and FGIDs are mainly symptomatic treatment.
The treatment of insomnia includes drug therapy and non-drug therapy. Although non-drug therapies such as cognitive behavioral therapy and stimulation control therapy are recommended for insomnia by the guide, hypnotics are still needed to achieve better sleep quality for these patients (Lou BX and Oks M, 2021; Shang ZJ, et al., 2021), among which the most common adverse reactions of hypnotics include dizziness, dry mouth, loss of appetite, constipation, etc. Especially for patients with insomnia and FGIDs, gastrointestinal adverse reactions will aggravate gastrointestinal symptoms (China Sleep Research Institute, 2021).
Currently, the medicine treatment of FGIDs is mainly symptomatic treatment with drugs, but there are still some problems (Black CJ, et al., 2020). For example, the proton pump inhibitor is widely used as the first-line therapy for FD (Wauters L, et al., 2021; Suzuki H, 2021), but some scholars have found that it may cause insomnia in patients (Lu Y, 2020; Zhou XL, et al., 2022). For patients with insomnia and FGIDs, while treating gastrointestinal diseases, it may increase the risk of insomnia.
In short, there are many contradictions in clinical treatment, and it is urgent to find new treatment methods. For the comorbidity of insomnia and FGIDs, acupuncture has the characteristics of rapid effect, strong tolerance, low recurrence rate and high safety. A large number of studies have shown that acupuncture is effective and safe in the treatment of insomnia or FGIDs (Feng H, et al., 2020; Fang QQ, et al., 2021; Wang XY, et al., 2021). Tui Na has the function of dredging channels and collaterals, and is widely used in the treatment of insomnia or FGIDs (Wang XY, et al., 2021; Feng G, et al., 2019; You Y, et al., 2021; Larussa T, et al., 2019). Acupuncture combined with Tui Na therapy is a more common treatment for patients with insomnia and FGIDs in clinical practice.
In recent years, several related studies have mentioned the problems of clinical treatment and found the clinical treatment methods, acupuncture and Tui Na, but these still lack high-quality clinical evidence to prove whether acupuncture or Tui Na is effective. Therefore, in our study, we first analyze the difference of curative effect between acupuncture and western medicine in treating patients with insomnia and FGIDs. Furthermore, we compared the efficacy of acupuncture alone with acupuncture combined with Tui Na in treating patients with insomnia and FGIDs to provide evidence-based basis for clinical practice.
Materials and Methods
We followed the methods of Feng G, et al., 2019.
Protocol and registration
The review protocol was conducted under the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and this system review had been registered on Prospero (CRD42022343673).
Inclusion criteria
Participants: Adult patients who met the diagnostic criteria for insomnia and FGIDs (Diagnostic and Statistical Manual of Mental Disorders (DSM- 5) and Chinese Classification of Mental Disorders (CCMD-3) were used as the diagnostic criteria for insomnia, and Rome II, Rome III or Rome IV were used as diagnostic criteria for FGIDs).
Intervention measures: Firstly, the treatment group was treated with acupuncture alone, while the control group was treated with benzodiazepines; furtherly, the treatment group was treated with acupuncture combined with Tui Na, while the control group was treated with acupuncture alone.
Outcome indicators: Pittsburgh Sleep Quality Index (PSQI) scores for the insomnia and FGIDs related assessment indicators.
Study type: Randomized Controlled Trials (RCTs) published in Chinese and English.
Exclusion criteria
• The data in RCTs did not meet the insomnia and FGIDs diagnostic criteria.
• The treatment group was treated with non-acupuncture, and the control group was treated with placebo, sham acupuncture, or non-benzodiazepines.
• Outcomes reported incompletely no PSQI scale score or missing data.
• Duplication of the study.
Literature search
Two authors (Dixiang Zhong and Ting Hong) separately searched eight databases from their inception to June 1, 2022 at the same time: PubMed, Excerpta Medica Database (EMBASE), the Cochrane Library, Web of science, China National Knowledge Infrastructure (CNKI), Wanfang Database, China Science Technology Journal Database, SinoMed Database. The details of the search strategy of PubMed were shown in Appendix.
Screening and data extraction
Two researchers (Yuanyuan Qi and Wendan Xue) independently screened RCTs according to the inclusion-exclusion criteria. Then, three researchers (Mengyun Zhu, Zheyou Chu, and Minrou Xu) separately extracted data from eligible RCTs. The extracted data included the authors, year of publication, sample size, characteristics of participants (age and sex, etc.), intervention measures, and outcome indicators. If differing opinions arose, a third researcher (Yingchun Miao) was consulted. Yingchun Miao conducted the search, Mei Han evaluated the abstract.
Risk of bias
The methodological quality of these included RCTs will be scored by two researchers (Dixiang Zhong and Ting Hong) according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins J and Green S, 2011). The following seven items were assessed: Random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Tree levels were used to evaluate the quality of the method: “Low risk of bias” (+), “high risk of bias” (-), and “unclear risk of bias” (?). If disagreement was seen in the assessments, this was resolved through discussion with a more experienced researcher (Yingchun Miao).
Data synthesis
The meta-analysis was conducted using RevMan (5.3) and Stata 16.0 software. Outcome indicators of insomnia and FGIDs were all continuous variables, so we used the Mean Difference (MD) and 95% Confidence Interval (CI) to represent the difference between the groups. We tested heterogeneity using the I square (I2) and p value (p), and if p<0.1 or I2>50%, it was assumed that the heterogeneity was significant and the random-effects model was selected. Otherwise, the fixed-effects model was validated, and the sources of heterogeneity were explored using subgroup analysis or sensitivity analysis. If the number of included RCTs was enough, the inverted funnel plot will be used to evaluate the impact of publication bias.
Results
Literature search
A total of 1,902 related articles were collected via the search strategy. After excluding 124 duplicate studies, 1778 articles remained, and after the multilayer screening, 9 RCTs (Xu F, et al., 2019; Ren ML, et al., 2017; Xu F, et al., 2013; Liang FJ, et al., 2020; Feng WT, 2017; Zhu LP and Ji N, 2019; Wang ZH, 2019; Wang Y, 2021; Gao YD, 2018) were included in this review. More details of literature search are shown in Figure 1.
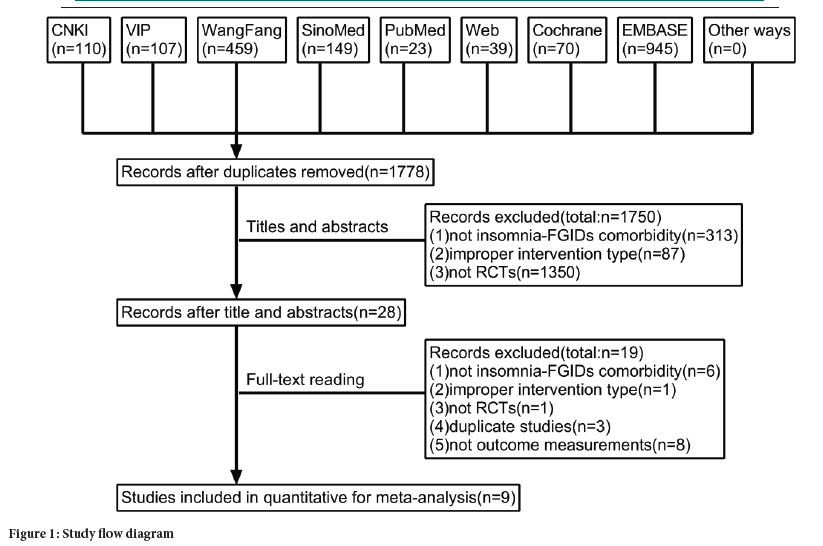
Figure 1: Study flow diagram
Study characteristics
We included 9 RCTs with 984 participants, 492 participants in the intervention group and 492 participants in the control group. 4 RCTs (Xu F, et al.,2019; Ren ML, et al., 2017; Xu F, et al., 2013; Liang FJ, et al., 2020) compared acupuncture with benzodiazepines. 5 RCTs (Feng WT, 2017; Zhu LP and Ji N, 2019; Wang ZH, 2019; Wang Y, 2021; Gao YD, 2018) compared acupuncture alone with acupuncture combined with Tui Na. The duration of treatment varied from 3 weeks to 1 month, 1 RCT did not mention it (Zhu LP and Ji N, 2019). 3 RCTs (Xu F, et al., 2019; Liang FJ, et al., 2020; Zhu LP and Ji N, 2019) did not mention the mean course. More details are shown in Table 1.
| Study ID | Participants (M/F) | Age (years) | Course (years) | Intervention | Control | Duration | Outcomes |
|---|---|---|---|---|---|---|---|
| Xu F, et al., 2019 | I: 170 | 18-70 | - | Acupuncture | Estazolam, 1 mg Qn | 30 days | PSQI |
| C: 170 | |||||||
| Ren ML, et al., 2017 | I: 16/17 | I: 63.8 ± 8.0 | I: 3.4 ± 1.7 | ||||
| C: 17/16 | C: 64.9 ± 8.2 | C: 3.0 ± 1.6 | |||||
| Xu F, et al., 2013 | I: 10/20 | I: 41.35 ± 11.68 | I: 20.65 ± 26.97 | ||||
| C: 8/22 | C: 40.55 ± 12.06 | C: 24.03 ± 29.01 | |||||
| Liang FJ, et al., 2020 | I: 8/22 | I: 56.07 ± 10.46 | - | Alprazolam, 0.4 mg Qn/Qod | 28 days | PSQI, 5-HT, VIP | |
| C: 15/15 | C: 60.10 ± 11.22 | ||||||
| Feng WT, 2017 | I: 56/44 | I: 51.33 ± 7.06 | I: 3.2 ± 0.8 | Acupuncture+Tui Na | Acupuncture | 30 days | PSQI |
| C: 55/45 | C: 52.47 ± 8.21 | C: 3.1 ± 0.5 | |||||
| Zhu LP and Ji N, 2019 | I: 22/18 | I: 51.23 ± 2.15 | - | - | |||
| C: 23/1I | C: 50.94 ± 2.01 | ||||||
| Wang ZH, 2019 | I: 20/20 | I: 51.4 ± 7.1 | I: 3.3 ± 0.8 | 21 days | |||
| C: 21/19 | C: 51.7 ± 6.9 | C: 3.4 ± 1.1 | |||||
| Wang Y, 2021 | I: 11/19 | I: 51.88 ± 12.38 | I: 2.98 ± 0.76 | 30 days | |||
| C: 10/20 | C: 51.81 ± 12.39 | C: 2.93 ± 0.79 | |||||
| Gao YD, 2018 | I: 10/9 | I: 41.5 ± 3.8 | I: 2.1 ± 0.4 | ||||
| C: 11/8 | C: 41.6 ± 3.7 | C: 2.0 ± 0.5 | |||||
| Note: I: Intervention; C: Control; M: Male; F: Female; Qn: Once at night; Qod: Every other day; PSQI: Pittsburgh Sleep Quality Index; 5-HT: 5-Hydroxytryptamine; VIP: Vasoactive Peptide | |||||||
Table 1: Characteristics of included Randomized Clinical Trials (RCTs)
Methodological quality evaluation
5 RCTs (Xu F, et al., 2019; Ren ML, et al., 2017; Xu F, et al., 2013; Liang FJ, et al., 2020; Wang ZH, 2019; Wang Y, 2021) reported the right randomization methods, while the remaining 4 RCTS (Xu F, et al., 2013; Liang FJ, et al., 2020; Wang ZH, 2019; Gao YD, 2018) did not mention how to produce the random sequence. None of the articles reported allocation concealment and blinding of outcome assessment. Due to the characteristics of acupuncture, it was hard to blind doctors and patients. So, we assessed all of them as ‘high’ risk. Only one RCT (Liang FJ, et al., 2020) reported the outcome indicators of insomnia and FGIDs, while the remaining 8 RCTs (Xu F, et al., 2019; Ren ML, et al., 2017; Xu F, et al., 2013; Feng WT, 2017; Zhu LP and Ji N, 2019; Wang ZH, 2019; Wang Y, 2021; Gao YD, 2018) only reported the PSQI. The detailed methodological quality evaluation is shown in Figures 2 and 3.
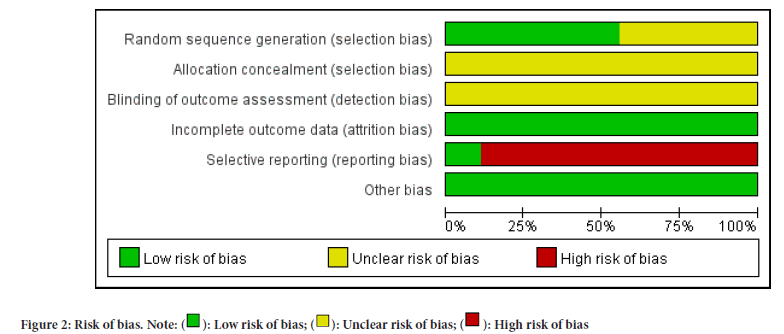
Figure 2: Risk of bias. Note: ( ): Low risk of bias; (
): Low risk of bias; ( ): Unclear risk of bias; (
): Unclear risk of bias; ( ): High risk of bias
): High risk of bias
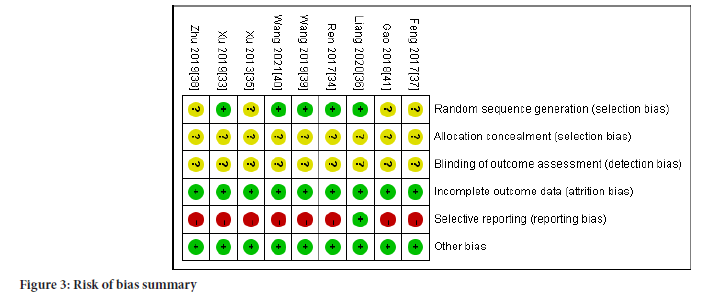
Figure 3:Risk of bias summary.
Results of meta-analysis
In these included 9 RCTs, all 9 RCTs reported PSQI score, and 1 RCT (Liang FJ, et al., 2020) reported FGIDs related assessment indicators.
PSQI score: In a comparison between the acupuncture group with the benzodiazepines group, 4 RCTs (Xu F, et al., 2019; Ren ML, et al., 2017; Xu F, et al., 2013; Liang FJ, et al., 2020) reported the PSQI score involving a total of 526 participants. Meta-analysis showed that acupuncture group was more effective than benzodiazepines group after treatment (MD-2.60, 95% CI (-4.95, -0.25), I2=96%) (Figure 4).
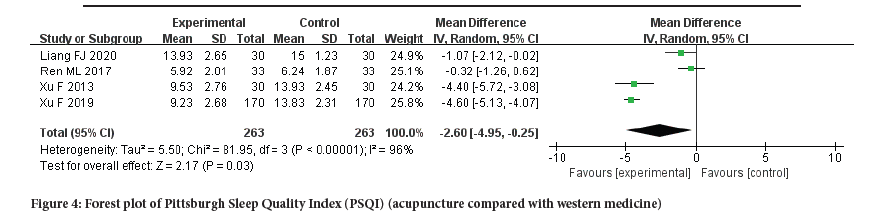
Figure 4:Forest plot of Pittsburgh Sleep Quality Index (PSQI) (acupuncture compared with western medicine).
In a comparison between the acupuncture group with acupuncture combined with Tui Na group, 5 RCTs (Feng WT, 2017; Zhu LP and Ji N, 2019; Wang ZH, 2019; Wang Y, 2021; Gao YD, 2018) were included the PSQI score involving a total of 458 participants. Meta-analysis showed that acupuncture combined with Tui Na group was more effective than acupuncture group after treatment (MD-2.48, 95% CI (-2.64, -2.33), I2=14%) (Figure 5).
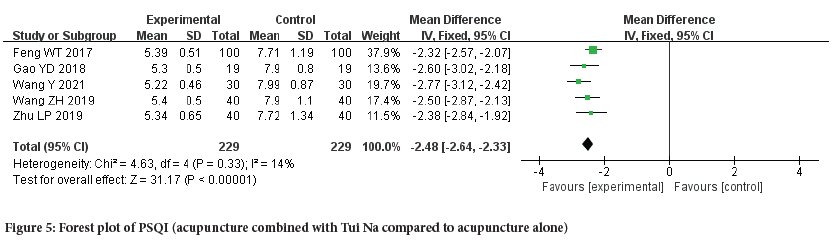
Figure 5:Forest plot of PSQI (acupuncture combined with Tui Na compared to acupuncture alone).
FGIDs related assessment indicators: One RCT (Liang FJ, et al., 2020) (total 60 participants) compared the acupuncture group with benzodiazepines group reported FGIDs related assessment indicators such as 5-HT and Vasoactive Intestinal Peptide (VIP). The results of 5-HT and VIP showed that there was a significant difference between acupuncture group and benzodiazepines group.
Sensitive analysis and publication bias: For PSQI score, comparing acupuncture group with benzodiazepines group, the heterogeneity was major among the studies (I2=96%>50%). But we did not find the heterogeneity source through the sensitivity analysis. More details of the sensitive analysis are shown in Figure 6. Considering the heterogeneity may come from the lack of included literature, the difference of acupuncture point selection, manipulation and intervention measures in the control group.
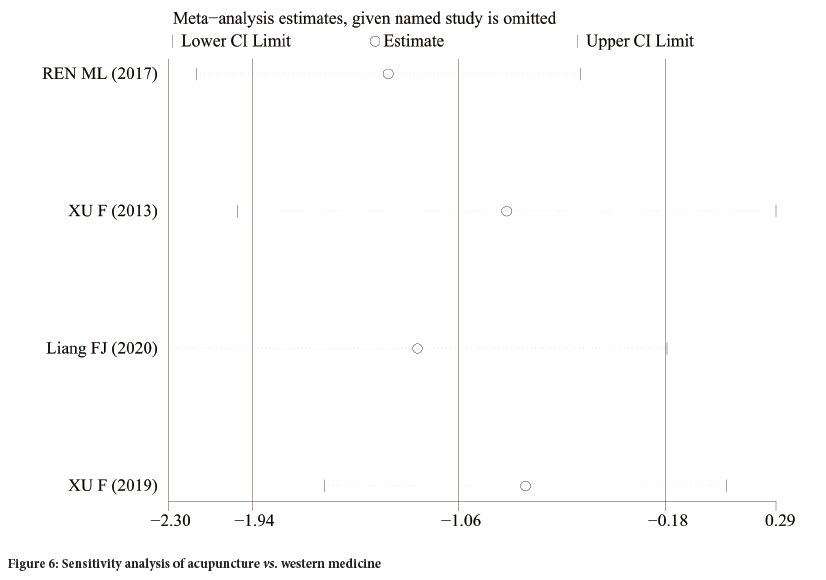
Figure 6:Sensitivity analysis of acupuncture vs. western medicine.
Discussion
Summary of results
We analyze the effect of acupuncture for patients with insomnia and FGIDs. Meta-analysis showed that the acupuncture group was better than the western medicine group in improving the sleep quality and regulating the level of brain-gut peptide for patients with insomnia and FGIDs, and acupuncture combined with Tui Na group is superior to acupuncture group in improving the sleep quality.
Possible mechanisms of acupuncture or Tui Na therapy for insomnia and FGIDs
Our review showed that acupuncture and acupuncture combined with Tui Na therapy appeared to be effective for patients with insomnia and functional gastrointestinal diseases. It is necessary to discuss the possible mechanisms of acupuncture or Tui Na therapy for insomnia and FGIDs. The possible mechanisms may be explained by Traditional Chinese Medicine (TCM) and modern medicine respectively. In TCM theory, the main and general cause of insomnia and FGIDs is the disharmony and imbalance of yin-yang, and qi-blood (Liu JC, et al., 2021). The possible mechanism of acupuncture and Tui Na for insomnia and FGIDs is that acupuncture and Tui Na can dredge channel and restore the harmony and balance of Yin-yang, Qi-blood. Modern medicine provides a certain basis for this comorbidity of insomnia and FGIDs through the understanding of Brain- Gut Axis (BGA) (Wang XY, et al., 2021; Hou LW, et al., 2020). Studies have shown that the brain-gut interaction mainly involves four ways: Microbiome, inflammation, nerve and endocrine (Ferrara M, et al., 2022). The four ways involve many material base, for example intestinal microbiome (Jackson ML, et al., 2015; Nishida K, et al., 2017), pro-inflammatory factors (Interleukin-1 (IL-1), Tumor Necrosis Factor (TNF)) (Joscelyn J and Kasper LH, 2014; Yehuda S, et al., 2009; Xiao HS and Liu L, 2021; Ren L, 2006), neurotransmitters (γ-Aminobutyric Acid (GABA) and Glutamic acid (Glu)) (Julio-Pieper M, et al., 2013), brain-gut peptides (Somatostatin (SS), Melatonin (MT) and 5- Hydroxytryptamine (5-HT)), and etc.
Acupuncture can regulate the levels of TNF-α, IL-25, GABA, Glu, SS, 5-HT and improve the diversity of intestinal flora in patients with acupuncture and FGIDs. Tui Na can improve the sleep quality and gastrointestinal function of patients by regulating neurotransmitters. Acupuncture combined with Tui Na can improve gastrointestinal symptoms by regulating the abundance of intestinal flora and SS level. In addition, acupuncture combined with Tui Na can improve sleep quality by regulating the levels of IL-6, TNF-α, and 5-HT.
Conclusion
Acupuncture and acupuncture combined with Tui Na can both improve the sleep quality of patients with insomnia and functional gastrointestinal diseases, and the efficacy of acupuncture combined with Tui Na is better than acupuncture alone. Practitioners could recommend this therapy to patients with insomnia and FGIDs according to the condition. However, it is not clear whether it can improve gastrointestinal symptoms. More high-quality clinical trials are needed to provide more powerful and comprehensive evidence in the future.
Limitations and Implications
As we mentioned above, the comorbidity of insomnia and FGIDs is common in clinic, but there is no effective treatment. Clinical practice and studies have found that acupuncture and Tui Na have a certain effect for patients with insomnia and FGIDs. So, we evaluate the effect of acupuncture and Tui Na for patients with insomnia and FGIDs, and furtherly provide evidence-based basis for clinical practice.+
Limitations
Although all literatures mentioned randomness, only five literatures described the correct random sequence generation method, and none of the nine literatures described the distribution result hiding and the blind method of outcome evaluator, all of which could cause selection bias. There are great differences in acupuncture point selection and manipulation, and the frequency and times of acupuncture treatment are not uniform. Especially, there are great differences between acupuncture intervention treatment and western medicine treatment in the control group, and some Tui Na treatment details are not clearly reported, which affects the homogeneity of the literature included in this study. Only one RCT mentioned the FGIDs related assessment indicators.
Implications for clinical practice
This meta-analysis study shows that acupuncture and acupuncture combined with Tui Na were effective for patients suffering from insomnia and FGIDs. Clinicians could recommend this therapy to patients, and finally make decisions based on various factors, such as the experience of doctors, the preferences of patients, etc. In addition, most of the included studies neglected the evaluation of the efficacy of gastrointestinal function, so we suggest that future researches should report the effects both of sleep and gastrointestinal function for patients with insomnia and FGIDs.
Declarations
The data supporting this meta-analysis are from previously reported studies and datasets, which have been cited. The processed data are available from the corresponding author upon request.
Data availability
The data supporting this meta-analysis are from previously reported studies and datasets, which have been cited. The processed data are available from the corresponding author upon request.
Authors’ contributions
The paper was drafted by Dixiang Zhong and revised by Yingchun Miao and Mei Han. The search strategy was performed by Dixiang Zhong and Ting Hong. Yuanyuan Qi and Wendan Xue independently screened the potential studies. Mengyun Zhu, Zheyou Chu, and Minrou Xu extracted data from the included studies and completed the data synthesis, Yingchun Miao offered arbitration in case of disagreement. All authors contributed to the interpretation of the results and gave their final approval for the version to be published.
Acknowledgments
The authors sincerely thank Guiyu Feng, Dongzhimen Hospital, Beijing University of Chinese Medicine, for helping to guide the design of research methods. This work was supported by Beijing ENN Fund for Chinese Medicine (2018-XAJLJJ-020).
Supplementary materials
The search strategy of PUBMED database as an example.
References
- Sleep Disorder Society. Guideline for the evaluation and treatment of insomnia in Chinese adults. Chin J Neurol. 2012; 17(7): 534-540.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing. 2013.
- Soldatos CR, Allaert FA, Ohta T, Dikeos DG. How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med. 2005; 6(1): 5-13.
[Crossref] [Google Scholar] [Pubmed]
- Li M, Zhang XW, Hou WS, Tang ZY. Insomnia and risk of cardiovascular disease: a meta-analysis of cohort studies. Int J Cardiol. 2014; 176(3): 1044-1047.
[Crossref] [Google Scholar] [Pubmed]
- Anothaisintawee T, Reutrakul S, van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Med Rev. 2016; 30: 11-24.
[Crossref] [Google Scholar] [Pubmed]
- Chan WS, Levsen MP, McCrae CS. A meta-analysis of associations between obesity and insomnia diagnosis and symptoms. Sleep Med Rev. 2018; 40: 170-182.
[Crossref] [Google Scholar] [Pubmed]
- Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. 2019; 43: 96-105.
[Crossref] [Google Scholar] [Pubmed]
- Andreev DN, Kucheryavy YA, Mayev IV. The prevalence and risk of sleep disorders in patients with functional dyspepsia: A meta-analysis.Zh Nevrol Psikhiatr Im S S Korsakova. 2021; 121(1): 26-30.
[Crossref] [Google Scholar] [Pubmed]
- Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: A systematic review with meta-analysis. Saudi J Gastroenterol. 2018; 24(3): 141.
[Crossref] [Google Scholar] [Pubmed]
- Drossman DA, Hasler WL. Rome IV-functional GI disorders: Disorders of gut-brain interaction. Gastroenterology. 2016; 150(6): 1257-1261.
[Crossref] [Google Scholar] [Pubmed]
- Black CJ, Drossman DA, Talley NJ, Ruddy J, Ford AC. Functional gastrointestinal disorders: Advances in understanding and management. Lancet. 2020; 396(10263): 1664-1674.
[Crossref] [Google Scholar] [Pubmed]
- Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021; 160(1): 99-114.
[Crossref] [Google Scholar] [Pubmed]
- Hyun MK, Baek Y, Lee S. Association between digestive symptoms and sleep disturbance: A cross-sectional community-based study. BMC Gastroenterol. 2019; 19: 1-6.
[Crossref] [Google Scholar] [Pubmed]
- Lei WY, Chang WC, Wong MW, Hung JS, Wen SH, Yi CH, et al. Sleep disturbance and its association with gastrointestinal symptoms/diseases and psychological comorbidity. Digestion. 2019; 99(3): 205-212.
[Crossref] [Google Scholar] [Pubmed]
- Tian DH. Huangdi Neijing Suwen. People's Medical Publishing House. 2005.
- Tait C, Sayuk GS. The Brain-Gut-Microbiotal Axis: A framework for understanding functional GI illness and their therapeutic interventions. Eur J Intern Med. 2021; 84: 1-9.
[Crossref] [Google Scholar] [Pubmed]
- Jiang W, Wang CJ. Disscussion on clinical experience of harmonizing spleen and stomach to treat insomnia based on theory of ''Brain-Gut Interaction''. Liaoning Journal of Traditional Chinese Medicine. 2021; 48(9): 41-44.
- Lou BX, Oks M. Insomnia: Pharmacologic treatment. Clin Geriatr Med. 2021; 37(3): 401-415.
[Crossref] [Google Scholar] [Pubmed]
- Shang ZJ, Zhang Z, Li HW. Clinical analysis of drug therapy for chronic insomnia. China Journal of Health Psychology. 2021; 29(2): 197-200.
- China Sleep Research Institute. Guide to diagnosis and treatment of insomnia in China. Chin J Neurol. 2017; 97(24): 1844-1856.
- Wauters L, Dickman R, Drug V, Mulak A, Serra J, Enck P, et al. United European Gastroenterology (UEG) and European Society for Neurogastroenterology and Motility (ESNM) consensus on functional dyspepsia. United European Gastroenterol J. 2021; 9(3): 307-331.
- Suzuki H. Recent advances in the definition and management of functional dyspepsia. Keio J Med. 2021; 70(1): 7-18.
[Crossref] [Google Scholar] [Pubmed]
- Lu Y. Adverse reactions of proton pump inhibitors and clinical rational drug use. China Continuing Medical Education. 2020; 12(3): 112-113.
- Zhou XL, Liu BS, Gong KK, Qiang J. 755 new and serious adverse drug reaction reports of proton pump inhibitors. Central South Pharmacy. 2022; 20(4): 949-954.
- Feng H, Liu Y, Xu H, Liu YH, Chen GL, Liu WJ. Effect of acupuncture and estazolam on episodic memory and sleep structure in patients with chronic insomnia disorder: A randomized controlled trial. Zhongguo Zhen Jiu. 2020; 40(7): 707-712.
[Crossref] [Google Scholar] [Pubmed]
- Fang QQ, Wang XQ, Liu CY, Xi HQ, Wan QY, Qin S, et al. The efficacy of acupuncture on the sleep structure of patients with insomnia: A systematic review and meta‐analysis. Anat Rec. 2021; 304(11): 2412-2425.
[Crossref] [Google Scholar] [Pubmed]
- Wang XY, Wang H, Guan YY, Cai RL, Shen GM. Acupuncture for functional gastrointestinal disorders: A systematic review and meta‐analysis. J Gastroenterol Hepatol. 2021; 36(11): 3015-3026.
[Crossref] [Google Scholar] [Pubmed]
- Feng G, Han M, Li X, Geng L, Miao Y. Clinical effectiveness of Tui Na for insomnia compared with estazolam: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2019; 47: 102186.
[Crossref] [Google Scholar] [Pubmed]
- You Y, Gao JJ, Xie MD. Research progress in the treatment of functional dyspepsia by massage. TCM Res. 2021; 34(11): 60-64.
- Larussa T, Rossi M, Suraci E, Marasco R, Imeneo M, Abenavoli L, et al. Use of complementary and alternative medicine by patients with irritable bowel syndrome according to the Roma IV criteria: A Single-Center Italian Survey. Medicina. 2019; 55(2): 46.
[Crossref] [Google Scholar] [Pubmed]
- Higgins J, Green S. Conchrane handbook for systematic reviews of interventions. Wiley. 2011.
- Xu F, Xuan LH, Zhou HJ, Chen FY, Zheng ZJ, Bi Y, et al. Acupoint catgut embedding alleviates insomnia in different Chinese medicine syndrome types: A randomized controlled trial. Chin J Integr Med. 2019; 25: 543-549.
[Crossref] [Google Scholar] [Pubmed]
- Ren ML, Qin M, Zeng KX. Clinical observation of insomnia of liver-qi stagnation treated by combination of qin’s scalp-acupuncture and percussopunctator sticking with plum-blossom needle. Journal of Clinical Acupuncture and Moxibustion. 2017; 33(12): 52-55.
- Xu F, Xuan LH, Zheng ZJ. Clinical study on acupoint catgut embedding therapy for insomnia of disharmony in stomach. Zhejiang Journal of Traditional Chinese Medicine. 2013; 48(11): 791-793.
- Liang FJ, Hu HX, Zhang JP, Yin MM, Wang Z. Influences of acupuncture on serum brain-gut peptides and sleep quality in treating primary insomnia with disturbance of stomach-qi. Chinese Journal of Integrative Medicine on Cardio-Cerebrovascular Disease. 2020; 18(13): 2042-2045.
- Feng WT. Clinical effect observation of acupuncture combined with massage in treating insomnia of the spleen and stomach disharmony type. China Foreign Med Treatment. 2017; 36(1): 170-172.
- Zhu LP, Ji N. Clinical effect observation of acupuncture combined with massage in treating insomnia of the spleen and stomach disharmony type. Electronic Journal of Clinical Medical Literature. 2019; 6(77): 52.
- Wang ZH. Clinical observation of acupuncture combined with massage in treating insomnia of the spleen and stomach disharmony type. China’s Naturopathy. 2019; 27(3): 21-22.
- Wang Y. Clinical efficacy and safety evaluation of acupuncture combined with massage in treating insomnia caused by disharmony between spleen and stomach. Diabetes. 2021; 18(7): 20-21.
- Gao YD. Clinical effect and prognostic evaluation of acupuncture and massage in treating insomnia due to disharmony between spleen and stomach. Biped and Health. 2018; 27(13): 186-187.
- Liu JC, Peng YS, Zhang WC. Discussion and application progress on the theory based on ‘stomach disorder leads to sleeplessness. China Journal of Traditional Chinese Medicine and Pharmacy. 2021; 36(11): 6635-6638.
- Wang XY, Zhang QM, Wang YG. Biological basis of stomach disorder leads to sleeplessness. Acta Chinese Medicine and Pharmacology. 2021; 49(12): 1-4.
- Hou LW,Rong PJ, Wei W. Application perspectives of digestive diseases and insomnia comorbidity based on brain-gut axis. China Journal of Traditional Chinese Medicine and Pharmacy. 2020; 35(09): 4541-4544.
- Ferrara M, Bertozzi G, Zanza C, Longhitano Y, Piccolella F, Lauritano CE, et al. Traumatic brain injury and gut brain axis: The disruption of an alliance. Rev Recent Clin Trials. 2022; 17(4): 268-279.
[Crossref] [Google Scholar] [Pubmed]
- Jackson ML, Butt H, Ball M, Lewis DP, Bruck D. Sleep quality and the treatment of intestinal microbiota imbalance in chronic fatigue syndrome: A pilot study. Sleep Sci. 2015; 8(3): 124-133.
[Crossref] [Google Scholar] [Pubmed]
- Nishida K, Sawada D, Kawai T, Kuwano Y, Fujiwara S, Rokutan K. Para‐psychobiotic Lactobacillus gasseri CP2305 ameliorates stress‐related symptoms and sleep quality. J Appl Microbiol. 2017; 123(6): 1561-1570.
[Crossref] [Google Scholar] [Pubmed]
- Joscelyn J, Kasper LH. Digesting the emerging role for the gut microbiome in central nervous system demyelination. Mult Scler. 2014; 20(12): 1553-1559.
[Crossref] [Google Scholar] [Pubmed]
- Yehuda S, Sredni B, Carasso RL, Kenigsbuch-Sredni D. REM sleep deprivation in rats results in inflammation and interleukin-17 elevation. J Interferon Cytokine Res. 2009; 29(7): 393-398.
[Crossref] [Google Scholar] [Pubmed]
- Xiao HS, Liu L. Discussion on the mechanism of treating insomnia based on brain-intestinal axis theory and stomach-tranquilizing therapy. Journal of Chengdu University of Traditional Chinese Medicine. 2021; 44(2): 108-113.
- Ren L. Study on hypnogenic effect and the mechanism of electroacpuncture in different acupoints groups. Jinan University. 2006.
- Julio-Pieper M, O’Connor RM, Dinan TG, Cryan JF. Regulation of the brain-gut axis by group III metabotropic glutamate receptors. Eur J Pharmacol. 2013; 698(1-3): 19-30.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Dixiang Zhong1, Mei Han2, Ting Hong1, Yuanyuan Qi1, Wendan Xue1, Mengyun Zhu1, Zheyou Chu1, Minrou Xu1 and Yingchun Miao11*2Department of Traditional Chinese medicine, Beijing University of Chinese Medicine, Beijing, China
Citation: Zhong D: The Clinical Effectiveness of Acupuncture for Patients with Insomnia and Functional Gastrointestinal Diseases: A Meta-Analysis of Randomized Controlled Trials
Received: 03-Mar-2023 Accepted: 27-Mar-2023 Published: 06-Apr-2023, DOI: 10.31858/0975-8453.14.4.278-285
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






