Research Article - (2022) Volume 13, Issue 6
Abstract
Background: Malnutrition has a negative impacted hospital outcome; hospitalized patients should receive proper nutritional management. Enteral Nutrition (EN) is the most common route for non-volitional dietary support, usually fed 4 times/day, different from patients with volitional feeding who receive only 3 meals/day. This practice may affect Blood Glucose (BG) control and increase nursing care's working burden. The aim of this study to compare BG control and enteral feeding complications between 3 and 4 times feeding/day in diabetes hospitalized patients who require EN.
Methods: A non-blind randomized controlled trial study of type 2 diabetes hospitalized patients who required EN in Thammasat University Hospital (TUH) from April 1 to December 31, 2019. The study patients were randomized and stratified by Glycated hemoglobin (HbA1C) at <8% or ≥ 8% to treat 3 meals or 4 meals/day at least 5 days or until stopped EN or discharged. The primary outcome was a percentage of times BG was in controlled at ≤ 180 mg/dl. Secondary outcomes were any feeding complications.
Results: 37 patients were included. 83% of the patients were female. There were none significant in mean percentage of BG control between 3 times and 4 times/day either in HbA1C<8% and HbA1C ≥ 8% (52.21% and 68.43%, p-value=0.192 and 54.29% and 55.10%, p-value=0.942, respectively). Percentage of hypoglycemic events were none significant in 3 vs. 4 times feeding at 1.70% vs. 0.99%, p-value=0.552 and 2.53% vs. 2.00%, p-value=0.727 in HbA1C<8% and HbA1C ≥ 8%, respectively. Other complications were not significant between 2 groups.
Conclusion: There was no clinically significant outcome on BG control and other complications between 3 and 4 times feeding/day in type 2 diabetes hospitalized patients. Three times feeding can be implied in clinical practice to reduce burden of nursing care.
Keywords
Enteral Nutrition (EN), Enteral feeding, Type 2 diabetes, Blood Glucose (BG), Feeding intolerance
Introduction
Type 2 diabetes mellitus is one of the most common non-communicable diseases and has been found in about 95% of diabetes patients. Therapy aims to control an acceptable blood sugar level to prevent complications. The most challenging part of the treatment plan is determining what to eat and following a meal plan. There is not a one-size-fits-all eating pattern for individuals with diabetes, and meal planning should be individualized. Medical Nutrition Therapy (MNT) is associated with A1C decreases of 0.3%-2% for people with type 2 diabetes (Care D, 2019). The goals of nutrition therapy are to promote healthy eating patterns to improve overall health, including achieving and maintaining body weight, control Blood Glucose, blood pressure, and serum lipid, and delay or prevent the complications of diabetes. Atherosclerosis complications such as cardiovascular and cerebrovascular diseases can render diabetes patients bedridden, resulting in required caregivers. Enteral Nutrition (EN) is the most common route for non- volitional nutritional support, usually used in bedridden patients. Indications of EN are in patients who decrease consciousness, dysphagia from neurological disease, and loss of appetite from chronic inflammatory diseases such as chronic liver disease and chronic kidney disease.
Also, malnourished patients result from surgical or psychological problems and inadequate energy intake for more than five days or underfeed less than 50% of calories requirement in 7 to 10 days (Stroud M, et al., 2003; Ciocon JO, 1990). However, there was no recommendation about meal frequency in EN feeding. Usually, patients with tube feeding are fed around four times a day as it is compatible with routine nursing care. Therefore, they also are fed four times a day at home. This practice may not be practical for their caregivers as people usually eat only three main meals a day.
Moreover, feeding time may affect diabetic patients, for example, the ability to control blood sugar or body weight. There was a study to compare the effect of six vs. two meals a day (breakfast and lunch) on body weight, Hepatic Fat Content (HFC), insulin resistance, and beta-cell function. The study was a randomized, open, crossover, single-center study in 54 patients with type 2 diabetes treated with oral hypoglycemic agents, both men and women, age 30-70 years, Body Mass Index (BMI) 27-50 kg/m2 and Glycated hemoglobin (HbA1C) 6%-11.8% to follow two regimens of a hypo energetic diet, six meals and two meals, each for 12 weeks. The diet in both regimens had the same macronutrient and energy content. The result found that bodyweight reduction, Hepatic Fat Content, insulin resistance, fasting plasma glucose, and C-peptide also glucagon were improved in 2 meals a day (Kahleova H, et al., 2014). A previous study found that dietary control with less meal frequency may influence Blood Glucose, lipid, insulin sensitivity, and metabolism rate. However, in hospitalized diabetes patients with EN feeding, the standard care is fed 4-6 meals/day to reduce the risk of aspiration or feeding intolerance. It is different from patients with volitional feeding who receive only three meals/day. This practice may affect Blood Glucose control in enteral feeding diabetes patients and increases in working burden of nursing care. As a result, this study aimed to compare Blood Glucose control and enteral feeding complications between 3 and 4 times feeding/day in hospitalized diabetes patients who require EN.
Materials and Methods
Study design
We conducted a non-blind randomized controlled trial in hospitalized type 2 diabetes mellitus patients in the medical ward of Thammasat University Hospital (TUH), who required enteral feeding. Study participants received either regular feeding four times or experimental feeding three times. The primary outcome was the percentage of times that Blood Glucose was in controlled at ≤ 180 mg/dl. Secondary outcomes were any feeding complications such as frequency of hypoglycemia, diarrhea, and Gastric Residual Volume (GRV) over 100 ml before the next feeding time. We enrolled hospitalized patients aged 18 years old or more diagnosed with type 2 diabetes mellitus and had a nasogastric tube for gastric feeding. They also had an Acute Physiology and Chronic Health Evaluation II (APACHE II) score of less than 30 and were stable on enteral feeding with more than 50% of energy requirement for more than 48 hours. Also, enteral feeding was in 5 days planned. Vital signs were stable. Endotracheal tube or tracheostomy tube intubation with ventilator used is acceptable. However, the exclusion criteria were pregnancy, critical illness with unstable vital signs, or end-of- life care. Also, patients with a gut obstruction or feeding intolerance with GRV>250 ml, diarrhea>3 times/day or >500 ml/day for two days, or who have received continuous dripping of enteral feeding were excluded.
Study protocol
After informed consent, patients will receive commercial diabetic formula with 30-35 kcal/kg/day and protein 0.8-2 gm/kg/day as an enteral feeding protocol of TUH. The study patients were randomized using a block of four and stratified by HbA1C at <8% or ≥ 8%. Accu- Chek® did Blood Glucose collection before feeding. Accu-Chek® has an accuracy that can detect Blood Glucose from 10 to 600 mg/dl in 5 seconds under a temperature of 8 to 44 degrees Celsius. Blood collection used just only 0.6 microliters from fingers, feet, arm, or forearm, also possible. The SD values at glucose levels <100 mg/dL are 3.2 mg/dL or less, and coefficient of variance values for glucose levels >100 mg/dL are 3.9% or less compared with venous blood sampling. Thammasat insulin protocol was used to correct Blood Glucose just only by the investigator. The data was collected for at least five days or until discharge or death.
Statistical analyses
The study was a pilot study; therefore, out of total participants only 30 participants could represent the study outcome. Categorical data will be shown as numbers and percentages. The comparison of the two groups will be conducted by Chi-squared test. Continuous data will be shown as mean and standard deviation. The comparison of these two groups will be shown by student T-test or Mann-Whitney U test. The data with p<0.05 is a significant statistic. SPSS version 18 will be used in data analysis. This study was approved by the Human Research Ethics Committee of Faculty of medicine Thammasat University with project number MTU- EC-IM-1-044/62 and registered to Thai Clinical Trails Registry number TCTR20190723002. This study has no conflict of interest.
Results
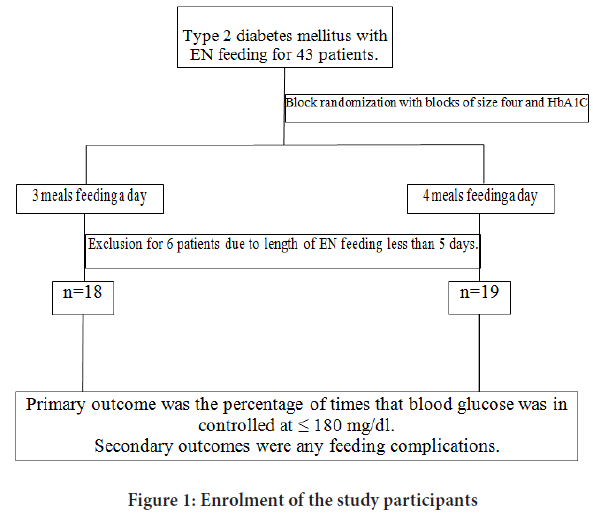
The study enrolled a total of 43 patients with type 2 diabetes mellitus with EN feeding between April 1 to December 31, 2019. The 6 participants were excluded due to the length of EN feeding being less than five days. Finally, a total of 37 patients have met the inclusion criteria and underwent randomization (Figure 1). The baseline characteristics of the participants are shown in Table 1. The study of 37 patients who were randomized to feed 3 meals/day for 18 patients and 4 meals/day for 19 patients. There was no significant statistic in baseline characteristic of 2 groups except there was female for 83% in 3 meals/day and 53% in 4 meals/day (p-value=0.046) and enteral feeding volume was 368.89 ± 33.46 ml/feed in 3 meals/day and 268.42 ± 49.89 ml/feed in 4 meals/days (p-value<0.001). Mean ages were 78.44 ± 8.14, 74.11 ± 10.03 years (p-value=0.159), HbA1C 8.31% ± 2.92%, 8.52% ± 3.47% (p-value=0.844), BMI 22.04 ± 4.52, 22.07 ± 5.07 kg/m2 (p-value=0.987), APACHE II score 15.56 ± 5.74, 18.00 ± 6.67 (p-value=0.241), Nutrition Alert Form (NAF) score C or severe malnutrition 56%, 47% (p-value=0.871), Pre-study Blood Glucose 226.01 ± 59.71, 197.95 ± 79.26 mg/dl (p-value=0.234), Pre-study insulin therapy was 16.7%, 26.3% (p-value=0.476), Length of study 17.50 ± 9.87, 17.21 ± 14.79 days (p-value=0.945), Calories intake 31.27 ± 5.06, 31.31 ± 3.30 kcal/kg/ day (p-value=0.975) and protein intake 1.24 ± 0.27, 1.27 ± 0.26 gm/kg/day (p-value=0.733) in 3 meals and 4 meals feeding respectively.
| Baseline characteristic of patients | Treatment A (3 meals/day) (n=18) | Treatment B (4 meals/d) (n=19) | p-value |
|---|---|---|---|
| Age (years) | 78.44 ± 8.14 | 74.11 ± 10.03 | 0.159 |
| Sex | Female: 15* (83%) | Female: 10* (53%) | 0.046 |
| Male: 3 (17%) | Male: 9 (47%) | ||
| Glycated hemoglobin (HbA1C) (%) | 8.31 ± 2.92 | 8.52 ± 3.47 | 0.844 |
| Body Mass Index (BMI) (kg/m2) | 22.04 ± 4.52 | 22.07 ± 5.07 | 0.987 |
| APACHE II score** | 15.56 ± 5.74 | 18.00 ± 6.67 | 0.241 |
| Nutrition Alert Form (NAF) score*** | A=1 (5%) | A=1 (6%) | 0.871 |
| B=7 (39%) | B=9 (47%) | ||
| C=10 (56%) | C=9 (47%) | ||
| Pre-study blood glucose (mg/dl) | 226.01 ± 59.71 | 197.95 ± 79.26 | 0.234 |
| Pre-study insulin therapy | 16.70% | 26.30% | 0.476 |
| Length of study (day) | 17.50 ± 9.87 | 17.21 ± 14.79 | 0.945 |
| Calories intake (kcal/kg/day) | 31.27 ± 5.06 | 31.31 ± 3.30 | 0.975 |
| Protein intake (gm/kg/day) | 1.24 ± 0.27 | 1.27 ± 0.26 | 0.733 |
| Enteral feeding volume/feed (ml) | 368.89 ± 33.46* | 268.42 ± 49.89* | <0.001 |
Note: Presented in mean ± SD and independent-samples T test Treatment A=3 meals/day, Treatment B=4 meals/day; *P<0.05; **APACHE II Score: Acute Physiology And Chronic Health Evaluation; ***NAF score A=normal-mild malnutrition, B=moderate malnutrition, C=severe malnutrition
Table 1: Baseline characteristic of patients
Figure 1: Enrolment of the study participants
There were none significant in mean percentage of BG control in ≤ 180 mg/ dl between 3 times feeding and 4 times feeding a day, 53.14% and 62.12% (p-value=0.275), respectively. Percentage of hypoglycemia were none significant in both groups, 2.19% and 1.93% (p-value=0.849), 3 meals and 4 meals respectively (Table 2).
| Percentage of time in Blood Glucose (BG) level | Treatment A (3 meals/day, n=18) | Treatment B (4 meals/day, n=19) | p-value |
|---|---|---|---|
| ≤ 180 mg/dl | 713 in 1231 times | 831 in 1290 times | 0.275 |
| 53.14% | 62.12% | ||
| <70 mg/dl | 27 in 1231 times | 25 in 1290 times | 0.849 |
| 2.19% | 1.93% |
Table 2: Percentage of time of blood sugar in 3 meals feeding and 4 meals feeding
There were none significant in percentage of Blood Glucose control ≤ 180 mg/dl in 3 meals/day and 4 meals/day in HbA1C<8% or ≥ 8% (52.21% and 68.43%, p-value=0.192 and 54.29% and 55.10%, p-value=0.942, respectively). Hypoglycemic events happened in 52 times in 2521 times, 2.06%. Hypoglycemic events were 27 times in 1231 time, 2.19% in 3 meals/ day and 25 times in 1290 times, 1.93% in 4 meals/day (p-value=0.849).
Both HbA1C<8% and HbA1C ≥ 8% has nonsignificant hypoglycemic events in 3 meals/day or 4 meals/day, 1.70% and 0.99% (p-value=0.552) and 2.53% and 2.00% (p-value=0.727), respectively as in Table 3. All patients with hypoglycemic events had no hypoglycemic symptoms. We corrected hypoglycemia by early feeding and repeat BG at 15 minutes after fed. Hypoglycemic events were in morning for 15 times in 27 times, 55.56% in 3 meals/day. In 4 meals/day, hypoglycemic events were in morning for 9 times and lunch for 8 times from total hypoglycemic events 25 times, 36% and 32% respectively (Table 3). There were none significant in complication of EN feeding (Table 4).
| Percentage of time in Blood Glucose (BG) level | HbA1C<8% | HbA1C ≥ 8% | ||
|---|---|---|---|---|
| Treatment A (3 meals/day, n=10) | Treatment B (4 meals/day, n=10) | Treatment A (3 meals/day, n=8) | Treatment B (4 meals/day, n=9) | |
| ≤ 180 mg/dl | 354 in 606 times | 501 in 762 times | 359 in 625 times | 330 in 528 times |
| 52.21% | 68.43% | 54.29% | 55.10% | |
| p-value | 0.192 | 0.942 | ||
| <70 mg/dl | 9 in 606 times | 13 in 762 times | 18 in 625 times | 12 in 528 times |
| 1.70% | 0.99% | 2.53% | 2.00% | |
| p-value | 0.552 | 0.727 | ||
Table 3: Percentage of time of blood sugar in HbA1C<8% and HbA1C ≥ 8%
| Nausea/Vomiting | Diarrhoea | Gastric Residual Volume (GRV)>100ml | |||
|---|---|---|---|---|---|
| Treatment A | Treatment B | Treatment A | Treatment B | Treatment A | Treatment B |
| No | No | No | No | 1 event | 1 event |
Table 4: Complication of Enteral Nutrition (EN)
Discussion
There was no study on meals frequency in EN before. Based on our knowledge, our study was the first study to identify the effects of feeding time to the impacts on blood sugar control and feeding complications in diabetic patients who required EN. We decided to do the study on hospitalized patients because if there were any complications from EN, we can correct the problem immediately.
As in recommendation of American Diabetes Association 2019 (Care D, 2019), the treatment goal of diabetes mellitus elderly patients with multiple coexisting chronic illnesses or impairments of activities of daily living or long-term care, fasting or pre-prandial glucose is 90-180 mg/dl and HbA1C which <8% or <8.5% is acceptable. In this studied, we designed to subgroup in HbA1C<8% and HbA1C ≥ 8% group to analyze the effect of HbA1C to Blood Glucose control because most of study populations were elderly and had co-morbidity with macro vascular complications. So, the cut point of HbA1C of this studied can be implied to use with safe.
Also, calories and protein intake in this study is appropriate as in recommendation of nutrition support for adults EN (Tejavanija S, 2017), as the participants in both 3 meals/day and 4 meals/day have received Diabetes mellitus formula commercial EN with calories intake 31.27 ± 5.06, 31.31 ± 3.30 kcal/kg/day (p-value=0.975) and protein intake 1.24 ± 0.27, 1.27 ± 0.26 gm/kg/day (p-value=0.733), respectively, which there was non-statistic significant between the groups. Diabetes mellitus formula EN was used in this studied, so Blood Glucose may not have an effect by feeding formula.
Blood Glucose was collected by Accu-Chek® Performa system (Accu- Chek®, 2014) with ISO 15197:2013, which has accuracy as SD values at glucose levels <100 mg/dL are 3.2 mg/dL or less, and coefficient of variance values for glucose levels >100 mg/dL are 3.9% or less compared with venous blood sampling to ensure Blood Glucose level collection of this studied.
Glycemic target is <180 mg/dl as in recommendation of glycemic targets in hospitalized patients (Care D, 2019) and Normoglycemia in Intensive Care Evaluation-Survival Using Glucose Algorithm Regulation (NICE-SUGAR) trial (Nice-Sugar Study Investigators, et al., 2009). Insulin will be infused if Blood Glucose exceeds 180 mg/dl by Thammasat insulin injection protocol (Jongsirikul S, et al., 2019). As in this protocol, the Blood Glucose correction makes sure that Blood Glucose variation does not depend on investigators.
The result has shown that there were none significant in mean percentage of BG control in ≤ 180 mg/dl between 3 times feeding and 4 times feeding a day, 53.14% and 62.12% (p-value=0.275), respectively. Percentage of hypoglycemia were none significant in both groups, 2.19% and 1.93% (p-value=0.849), 3 meals and 4 meals respectively.
In subgroup analysis of HbA1C<8% or ≥ 8%, Blood Glucose controlled was non-significant in 3 meals/day and 4 meals/day, 52.21% and 68.43%, p-value=0.192 and 54.29% and 55.10%, p-value=0.942, respectively.
Hypoglycemic events in HbA1C<8% or ≥ 8% was no statistically significant in both 3 meals/day and 4 meals/day groups, 1.70% and 0.99% (p-value=0.552) and 2.53% and 2.00% (p-value=0.727), respectively. There was a studied in 2009 found that hypoglycemic in hospitalized patients were 10.1% in critical illness ward and 3.5% in general medical ward (Cook CB, et al., 2009).
Our studied had hypoglycemic events lower than the past studied. The hypoglycemic events were occurred in morning for 55% in 3 meals/day but in 4 meals/day, hypoglycemic is not correlated to each meal. This maybe because 3 meals/day has longer fasting time. Late feeding for 1-2 hours of dinner time may correct the frequent morning hypoglycemia.
There were no symptoms of hypoglycemia in this studied, we corrected by early feeding and checked Blood Glucose 15 minutes after that.
Other complications were not different in 2 groups. Gastric Residual Volume>100 ml occurred in both group each 1 event even though enteral feeding volume per feed was more in 3 meals group (368.89 ± 33.46 ml/ feed in 3 meals and 268.42 ± 49.89 ml/feed in 4 meals, p-value<0.001). Metoclopramide was given to correct this complication. And patients have no feeding intolerance after that.
There was no previous studied on diabetes EN and Blood Glucose. Munsters MJ and Saris WH studied in 2012, male with BMI 21.6 ± 0.6 kg/m2 who were randomized to receive low meal frequency (3 meals/day) and high meal frequency (14 meals/day) with same calories intake and Carbohydrate: Protein: Fat is 55:15:30. This study showed that 3 meals/day has low Blood Glucose level, improve in resting metabolic rate and increased satiety and reduced hunger. Three meals per day can be relevant for blood sugar and body weight control on the long term.
Another studied in 2014 by Kahleova H, et al. a comparison the effect of 6 six vs. 2 meals a day, on body weight, Hepatic Fat Content (HFC), insulin resistance and beta cell function. A randomized studied in 54 patients with type 2 diabetes treated with oral hypoglycemic agents, both men and women, age 30-70 years, BMI 27-50 kg/m2 and HbA1C 6%-11.8% to follow two regimens of diet, 6 and 2 meals, each for 12 weeks. The result found that body weight reduction, Hepatic Fat Content, insulin resistance, fasting plasma glucose and C-peptide also glucagon were also improved in 2 meals a day.
And there was a study (Farshchi HR, et al., 2005) on meal frequency and blood sugar in obese women with BMI 37.1 ± 4.8 kg/m2. A randomized crossover trial, phase 1 (14 days) normal diet (6 occasions/day with a regular meal pattern) or variable meal frequency (3-9 meals/day, irregular meal pattern). In phase 2 (14 days), it is similar to phase I but in alternative meal pattern. Blood sugar, lipid, insulin concentrations were collected before and 3 hours after meals. The result found that regular meal pattern associated with lower energy intake, greater postprandial thermogenesis and lower fasting total and Low-Density Lipoprotein (LDL) cholesterol.
The result of this study has been correlated with the previous research that fewer meals influence blood sugar control.
The strengths of our trial included a randomized controlled trial, and there was no previous study of meal frequency in enteral feeding.
Our trial has some limitation that is a pilot study with a small size of the population. Another studied with more populations sized may show an effect.
Conclusion
According to our knowledge, there was no study on meals frequency in EN before. This study was the first study to identify the effects of 3 and 4 times feeding/day on blood sugar control and feeding complications in diabetic patients who required EN. There was no clinically significant outcome on BG control and other complication between 3 and 4 times feeding/day in type 2 diabetes hospitalized patients. Therefore, 3 times feeding can be implied in clinical practice to reduce burden of nursing care.
References
- Care D. Lifestyle Management: Standards of medical care in diabetes 2019. Diabetes Care. 2019; 42(1): S46-S60.
[Crossref] [Google Scholar] [Pubmed]
- Stroud M, Duncan H, Nightingale J. Guidelines for enteral feeding in adult hospital patients. Gut. 2003; 52(7): 1-2.
[Crossref] [Google Scholar] [Pubmed]
- Ciocon JO. Indications for tube feedings in elderly patients. Dysphagia. 1990; 5(1): 1-5.
[Crossref] [Google Scholar] [Pubmed]
- Kahleova H, Belinova L, Malinska H, Oliyarnyk O, Trnovska J, Skop V, et al. Eating two larger meals a day (breakfast and lunch) is more effective than six smaller meals in a reduced-energy regimen for patients with type 2 diabetes: A randomised crossover study. Diabetologia. 2014; 57(8): 1552-1560.
[Crossref] [Google Scholar] [Pubmed]
- Care D. Older Adults: Standards of Medical Care in Diabetes 2019. Diabetes Care. 2019; 42(1): S139-S147.
[Crossref] [Google Scholar] [Pubmed]
- Tejavanija S. Clinical Practice Recommendation for the nutrition management in adult hospitalized patients. Society of parenteral and enteral nutrition of Thailand. 2017; 1: 26-37.
- Accu-Chek®. Evaluation Report: Accu-Chek® Performa Test Strips with Advanced Chemistry. Accu-Chek®. 2014.
- Care D. Diabetes care in the hospital: Standards of medical care in diabetes-2019. Diabetes Care. 2019; 42(1): S173-S181.
[Crossref] [Google Scholar] [Pubmed]
- Nice-Sugar Study Investigators, Finfer S, Chittock D, Yu-Shuo S, Blair D, Foster D, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009; 360(13): 1283-1297.
[Crossref] [Google Scholar] [Pubmed]
- Jongsirikul S, Tharavanij T, Anthanont P, Sritipsukho P, Tonglim J. Glycemic control of in-patient type2 diabetes mellitus comparing between Thammasart insulin protocol and routine care: Randomized-controlled trial. The 35th Annual Meeting of the Royal College of Physicians of Thailand. 2019.
- Cook CB, Kongable GL, Potter DJ, Abad VJ, Leija DE, Anderson M. Inpatient glucose control: A glycemic survey of 126 US hospitals. J Hosp Med. 2009; 4(9): 7-14.
[Crossref] [Google Scholar] [Pubmed]
- Munsters MJ, Saris WH. Effects of meal frequency on metabolic profiles and substrate partitioning in lean healthy males. PloS One. 2012; 7(6): 38632.
[Crossref] [Google Scholar] [Pubmed]
- Farshchi HR, Taylor MA, Macdonald IA. Beneficial metabolic effects of regular meal frequency on dietary thermogenesis, insulin sensitivity, and fasting lipid profiles in healthy obese women. Am J Clin Nutr. 2005; 81(1): 16-24.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Kwansuphang Wongwatanasanti1* and Sanit Wichansawakun22Department of Clinical Nutrition, Thammasat University, Pathum-Thani, Thailand
Citation: Wongwatanasanti K: The Comparison of the Effects of 3 Meals Feeding a Day and 4 Meals Feeding a Day in Type 2 Diabetes Mellitus Hospitalized Patients in Thammasat University Hospital on Blood Sugar Control and Enteral Feeding Complications
Received: 02-May-2022 Accepted: 27-May-2022 Published: 03-Jun-2022, DOI: 10.31858/0975-8453.13.6.385-389
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3