Research Article - (2022) Volume 13, Issue 3
Abstract
Background: Spinal Anesthesia (SA) is a common technique used worldwide for cesarean sections. A common, but potentially fatal, complication is hypotension. It can cause a significant effect on the mother and fetus. Hydration has become the cornerstone of prophylaxis of hypotension in obstetrics previously but recent studies showed that co-loading also may be a better option in the prevention of spinal induced hypotension. This study aimed to assess the effect of preloading and co-loading in the prevention of hypotension among mothers who underwent cesarean delivery under spinal anesthesia. Methods: Prospective cohort study was conducted at Debre Tabor Comprehensive Specialized Hospital from February 15 to April 15/2021 Ninety-six pregnant mothers who have c/s were included in the study period. The pregnant were given 20 ml/kg of fluid. The preload group gave fluid 20 minutes before spinal block; while the co-load group received fluid starting as soon as CSF was tapped. Independent sample t-test and Chi-square test were used. Data was entered and analyzed using SPSS version 25. Results: The incidence of systolic hypotension after spinal anesthesia was 77.1% in the preload group and 35.4% in the co-load. The preload group mothers develop more hypotension than co load mothers. Conclusion: Hypotension occurred 77.1% of the time in the preload group and 35.4 percent of the time in the co-load group, according to this study. As a result, crystalloid co-loading was superior to preloading in preventing spinal anesthesia-induced hypotension in mothers who had a cesarean section.
Keywords
Caesarean section, Co-load, Fluid, Preload, Spinal anesthesia
Abbreviations
ASA: American Society of Anesthesia; BMI: Biomass Index; BP: Blood Pressure; CS: Caesarean Section; DBP: Diastolic Blood Pressure; DTCSH: Debre Tabor Comprehensive Specialized Hospital; MAP: Mean Arterial Blood Pressure; SA: Spinal Anesthesia; SAB: Subarachnoid Block; SBP: Systolic Blood Pressure; SIH: Spinal Induced Hypotension
Introduction
Spinal anesthesia (SA) is accomplished by introducing small amounts of local anesthetic into the cerebrospinal fluid in the subarachnoid space (Casey WF and Ankcorn C, 2000). It is commonly used for surgical procedures performed in the lower abdomen, pelvis, perineal and lower extremities; to generalize, is beneficial for procedures below the umbilicus (Olawin AM and Das JM, 2019). SA has many advantages; it is less expensive, has fewer side effects on the respiratory system if a high block is avoided, the airway remains intact, reducing the risk of aspiration, and provides excellent muscle relaxation for lower abdominal and lower limb surgery (Casey WF and Ankcorn C, 2000).
Spinal anesthesia (SA) is the most commonly used technique for elective cesarean sections around the world. However, hypotension is still the most common complication with this technique (Naskar C, et al., 2013). SIH is the most common cardiovascular response to spinal anesthesia, resulting in a decrease in cardiac output and blood flow to the placenta as a result of the sympathetic blockade caused by neuraxial anesthesia (Farid Z, et al., 2016).
Maternal hypotension lasting more than 2 min may be associated with lower Apgar scores. It is caused by an increase in venous capacitance and a reduction in systemic vascular resistance. On the other hand, uterine blood flow is dependent on perfusion pressure, so the reduced blood flow due to hypotension leads to compromise in fetal oxygenation (Varshney RK and Kapoor K, 2016).
The clinicians have used various methods and techniques such as leg wrapping, elastic stockings, optimizing patient’s position, intravenous fluids, and vasopressors from time to time to offset these hypotensive effects of spinal anesthesia with varying degrees of success. One of the foremost methods includes prophylactic administration of intravenous fluids before implementation of the subarachnoid block to offset the effects of hypotension (Bajwa SJS, et al., 2013).
Hypotension during spinal anesthesia for cesarean delivery is a common and problematic complication, both from the maternal and fetal- neonatal point of view (Lotfy ME, et al., 2014). The sympathectomy, caused by spinal anesthesia, causes Systemic Vascular Resistance (SVR) to drop and the venous capacitance to increase; and secondary relative hypovolemia causes hypotension in turn (Kilinç N, et al., 2020). Its occurrence seen in patients undergoing cesarean section under spinal anesthesia varies from 60%-70% (Bhardwaj N, et al., 2020; Ni HF, et al., 2017). It can lead to nausea, vomiting, aspiration, dizziness, syncope, and arrhythmias in the mother. Maternal hypotension further compromises uteroplacental blood flow which can cause fetal hypoxia and acidosis (Bhardwaj N, et al., 2020).
Techniques used to prevent maternal hypotension include intravascular volume expansion using IV. Fluid preload immediately before spinal injection, use of left lateral tilt or manual uterine displacement, or both and administration of IV. Fluids and vasopressor drugs are both prophylactically and in response to the cardiovascular changes after neural block (Jackson R, et al., 1995).
Replacement of intravascular volume and vasopressors are considered the gold standard for the prevention and treatment of SIH (Kaufner L, et al., 2019). However, the timing of fluid administration remained controversial (Jackson R, et al., 1995; Jain P and Valecha D, 2017). There were no studies conducted on the effect of preloading and co-loading of fluid administration to prevent SIH in DTCSH. This study was aimed to compare the effectiveness of pre-loading and co-loading of fluid administration to prevent SIH (Teoh WH and Sia RT, 2009; Oh AY, et al., 2014).
Spinal anesthesia is a common and well-accepted technique applied in obstetric surgical intervention and its greatest complication is hypotension. Unless this complication is promptly managed, jeopardizes both the mother and the fetus. Some studies showed that the incidence of spinal hypotension can be reduced by fluid but there are arguments in the timing of fluid administration.
As far as we know, no similar research has been done, and no published evidence exists on the effect of preloading and co-loading fluid administration (Banerjee A, et al., 2010) on SIH prevention in our country Ethiopia. So that, it can be used as a source of information for future researchers, and it can also be used by program planners and policymakers to devise different strategies that help to improve and prevent spinal anesthesia-induced hypotension in the caesarian section (c/s).
Materials and Methods
Study design, setting, and population
The prospective cohort study was conducted from February 15 to April 15/2021 in DTCSH, located at the zonal city of Debre Tabor in south Gondar, Ethiopia. Approval of institutional ethical committee and informed written consent of patients was obtained. This study was reported in line with STROCSS criteria and registered on www.researchregistry with research registry 7326 which is available at https://www.researchregistry.com/register-now#home/. Total ninety sixty ASA II pregnant mothers were included in the study. Preload group received 20 ml/kg of NS 20 minute before and co load group were given the same volume of solution for after CSF tapping (Jacob JJ, et al., 2012; Parmar SB, et al., 2012). Hypotension was defined as a decrease in systolic blood pressure of more than 20% from the baseline or a decrease of systolic blood pressure to less than 90 mm Hg as an absolute value.
Inclusion criteria
All volunteer pregnant mothers who come for cesarean section and that have undergone spinal anesthesia (Kumari S and George JK, 2017).
Exclusion criteria
Pregnancy-induced hypertension, those who have received a combination of a spinal block with another type of anesthesia, patients with hypotension due to antepartum hemorrhage or sepsis coming for caesarian section. Any Patient noted to have unexplained hypotension (systolic BP below 90 mm Hg) or hypertension (systolic BP above 140 mm Hg) before the block and repeated spinal anesthesia.
Sampling technique
Sample size determination: The sample size was calculated using Pocock’s formula for sample size estimation for two proportion studies-
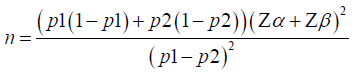
Where: n=desired sample size
Z α=standard normal deviation at 5% significance level (1.96) for a two- sided test
Z β=power of the test (0.84)
P1=Proportion of interest of the preload group with hypotension
P2=Proportion of interest of the co-load group with hypotension
A study in Nigeria showed the incidence of hypotension for preload 48.3% and co-load 20.7% (22).
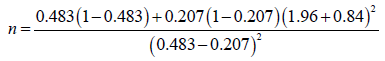
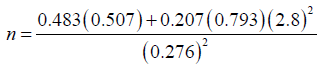
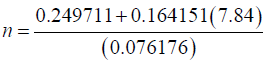
To make up for protocol violation/attrition 10% was added to the calculated sample size i.e., 43+5=48 for each group.
Sampling technique
All consecutive mothers undergoing cesarean section were included until the determined sample is completed in the study period (Dyer RA, et al., 2004; Idehen HF, et al., 2014).
Data processing analysis
The data were coded, entered, and analyzed by using SPSS Version 25 software and presented in form of tables, graphs, charts, and texts. Continuous variables are expressed as mean ± SD or median ± IQR based on the normality assumption. Analysis was done by independent sample t-test, χ2 or Fisher’s exact test as appropriate and P-value <0.05 considered as statistically significant (Olajumoke TO, et al., 2017).
Data quality control and assurance
Data collectors were trained by principal investigators. Pretest done for 1 week in 5% of the sample size at Felege Hiwot referral hospital and during data collection, regular supervision and follow up was made appropriately (Singhal A, et al., 2019). The principal investigator cross-checked for completeness and consistency of data every day.
Operational definition and definition of terms
Spinal-Induced Hypotension (SIH): Reduction in Systolic Blood Pressure (SBP) of 20% or more from baseline values after induction of spinal anesthesia (Ohpasanon P, et al., 2008).
Baseline BP: The BP recorded before administration of spinal anesthesia
Co-loading: Giving fluid while at the same time performing spinal anesthesia (Williamson W, et al., 2009).
Preloading: Administration of fluid 20 minutes before anesthesia initiated (Williamson W, et al., 2009).
Results
Demographic and clinical data of study participants
A total of 96 ASA II mothers with C/S under spinal anesthesia were included in this study. Among these 48 were preloaded and 48 were co-loaded. Age, V/S, BMI, total blood loss during the surgery, and APGAR score were comparable between the two groups (Table 1).
| Variables | Preload group (n=48) | Co-load group (n=48) | P-value |
|---|---|---|---|
| Age (mean ± std deviation) | 32.65 ± 5.27 | 32.06 ± 5.14 | 0.48 |
| BMI (kg/m2) (Median (range)) | 24.5 (21-30) | 26.93 (27-35) | 0.43 |
| Gravida of the mother (mean ± std deviation) | 4.08 ± 0.94 | 4.08 ± 1.12 | 0.86 |
| Sensory level of SA (median(range)) | T10 (T10-T8) | T10 (T10-T8) | 0.1 |
| APGAR score at 1 min (mean ± std deviation) | 8.25 ± 0.75 | 8.27 ± 0.76 | 0.06 |
| APGAR score at 5 min (mean ± std deviation) | 8.47 ± 0.71 | 8.87 ± 0.63 | 0.63 |
| Amount of fluid (ml) (median(range)) | 1500 (1320-1700) | 1500 (1200-1700) | 0.42 |
| Blood loss (mean ± std deviation) | 614.37 ± 74.83 | 611.25 ± 70.37 | 0.96 |
| Experience of anesthetist in year (median(range)) | 6 (4-7) | 6 (5-1) | 0.45 |
| Experience of obstetrician in year (median(range)) | 8 (5-10) | 8 (5-8) | 0.38 |
| Duration of surgery in minute (median(range)) | 40 (35-50) | 45 (30-50) | 0.034 |
Note: where n=desired sample size
Table 1: Demographic and clinical data of women who underwent cesarean delivery under spinal anaesthesia in Debre Tabor Comprehensive Specialized Hospital, North-central Ethiopia, 2021
The blood pressure of women who underwent spinal anesthesia
The systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure were comparable. The minimum median SBP value recorded in group preload was 70 which were recorded at 20th minutes of SAB which was statistically significant.
The pulse rate of women who underwent spinal anesthesia
The baseline and first sixty-minute pulse rates in the two groups were comparable and the difference was not statistically significant.
The incidence of hypotension in women who underwent cesarean delivery
The overall incidence of systolic hypotension after spinal anaesthesia was 77.1% in the preload group and 35.4% in the co-load group, which is statistically significant (p<0.05). There was a statistically significant difference in the incidence of hypotension at 10 and 20 minutes after spinal anaesthesia in between groups (P<0.05) (Figure 1).
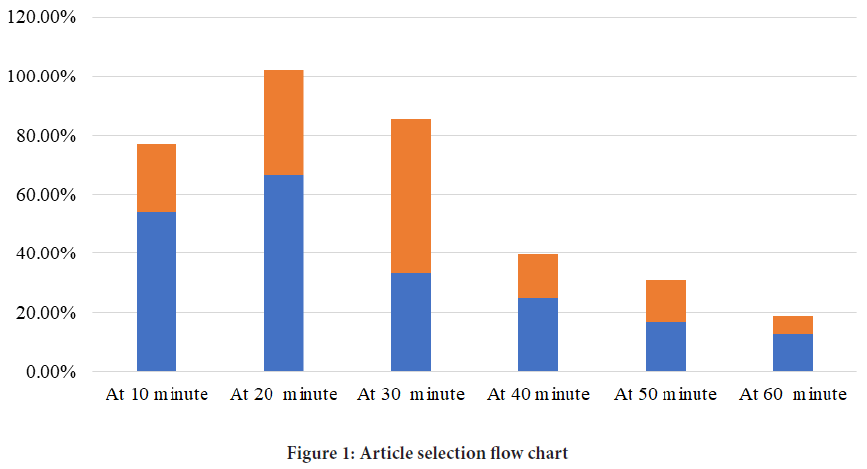
Figure 1: Article selection flow chart
Discussion
Hypotension is a common side effect of spinal anesthesia, occurring in 16%-33% of cases. It is thought to be caused by a decrease in either Systemic Vascular Resistance (SVR) or Cardiac Output (CO), or both. This response is exacerbated in pregnant mothers by aortocaval compression of the gravid uterus when they lie supine (Farid Z, et al., 2016).
Various methods and techniques have been used, such as leg wrapping, elastic stockings, optimizing patient’s position, intravenous fluids, and vasopressors to offset these hypotensive effects of spinal anesthesia with varying degrees of success (Bajwa SJS, et al., 2013).
One of the foremost methods includes prophylactic administration of intravenous fluids before implementation of the subarachnoid block to offset the effects of hypotension (Bajwa SJS, et al., 2013). Fluid preloading for cesarean section under regional anesthesia has been established as routine and well-thought-out to be a safe and effective method of reducing the incidence of hypotension previously (Varshney RK and Kapoor K, 2016).
Despite numerous studies on the effectiveness of preload versus co-load on the effect of spinal-induced hypotension, neither technique is accepted as the most effective or safe, leaving the field open for further investigation.
In this study, there was a statistically significant difference in the incidence of hypotension in preload (77.1%) versus co-load (35.4%) groups. In line with this finding a study by Oh, et al. (Oh AY, et al., 2014) showed that there was a statistically significant difference in the incidence of hypotension between preload (83%) and co-load (53%) groups. Both studies showed that the blood pressure significantly dropped in preload group (Table 2).
| Variables | Preload group (n=48) | Co-load group (n=48) | P-value |
|---|---|---|---|
| Baseline SBP (mean ± std deviation) | 116.93 ± 9.58 | 121.39 ± 9.91 | 0.48 |
| Baseline DBP (Median (range)) | 75.5 (70-85) | 79 (68-90) | 0.09 |
| Baseline MAP (Median (range)) | 81(63-99) | 90(68-102) | 0.12 |
| 10-minute SBP (Median (range)) | 82(60-114) | 100(55-28) | 0.29 |
| 10-minute DBP (Median (range)) | 58.41(9.30) | 62.72(8.71) | 0.07 |
| 10-minute MAP (mean ± std deviation) | 71.52 ± 7.48 | 78.64 ± 8.76 | 0.5 |
| 20-minute SBP (Median (range)) | 70(58-115) | 100(50-123) | <0.0001* |
| 20-minute DBP (Median (range)) | 54(42-75) | 60(45-78) | 0.1 |
| 20-minute MAP (Median (range)) | 66(60-90) | 74(57-92) | 0.09 |
| 30-minute SBP (Median (range)) | 84(60-117) | 100(50-120) | 0.02* |
| 30-minute DBP (Median (range)) | 60(45-75) | 60(53-88) | 0.07 |
| 30-minute MAP (Median (range)) | 66(60-80) | 74(66-92) | <0.0001* |
| 40-minute SBP (Median (range)) | 95(60-113) | 103(60-125) | 0.01* |
| 40-minute DBP (mean ± std deviation) | 63.43 ± 5.49 | 68.50 ± 7.40 | 0.6 |
| 40-minute MAP (Median (range)) | 69(65-84) | 76(65-91) | <0.0001* |
| 50-minute SBP (Median (range)) | 96(60-118) | 105(64-122) | <0.0001* |
| 50-minute DBP (Median (range)) | 67(56-84) | 70(64-88) | 0.01* |
| 50-minute MAP (Median (range)) | 72(66-87) | 78(67-92) | <0.0001* |
| 60-minute SBP (Median (range)) | 99(60-117) | 106(65-125) | 0.6 |
| 60-minute DBP (Median (range)) | 68(60-96) | 73(60-96) | 0.001* |
| 60-minute MAP (Median (range)) | 75(69-89) | 79(68-95) | 0.14 |
Note: where *=significantiy different from all other times (p<0.01) and n=desired sample size
Table 2: The blood pressure of women who underwent cesarean delivery under spinal anaesthesia in Debre Tabor Comprehensive Specialized Hospital, North-central Ethiopia, 2021
The findings of this study, (77.1%) of preload group and (35.4%) of the co- load group is more compared with the study done by Ni HF, et al. (Ni HF, et al., 2017). which revealed that there was a statistically significant difference in the incidence of hypotension (57.8%) in the preload group and (47.1%) in the co-load group.
The result of this study was in line with the study done by Kulkarni, et al. (Kulkarni AG, et al., 2016) showed that there was a statistically significant difference in the incidence of hypotension after spinal anesthesia (72%) for preload groups and (23%) for co-load groups. The study by Khan M, et al. (Khan M, et al., 2013) also showed that (70%) of preload mothers and (44%) of co-load mothers developed hypotension after spinal anesthesia which has a statistically significant difference. The finding of this study is also close to the study of David Bruck, et al. and they got 72% from preload and 39 from co-load groups develop hypotension (Zhao PS, et al., 2014) (Table 3).
| Pulse rate | Preload group (n=48) | Co-load group (n=48) | p-value |
|---|---|---|---|
| Baseline (Median (range)) | 80(70-105) | 82(72-120) | 0.12 |
| 10 minute (Median (range)) | 84(70-98) | 84(74-100) | 0.47 |
| 20 minute (Median (range)) | 82(73-96) | 84(75-110) | 0.56 |
| 30 minute (Median (range)) | 84(70-114) | 80(66-98) | 0.49 |
| 40 minute (Median (range)) | 82(72-104) | 84(65-100) | 0.53 |
| 50 minute (Median (range)) | 84(72-108) | 85(64-102) | 0.1 |
| 60 minute (Median (range)) | 84(72-79) | 85(62-78) | 0.19 |
Note: where n=desired sample size
Table 3: The pulse rate of women who underwent cesarean delivery under spinal anaesthesia in Debre Tabor Comprehensive Specialized Hospital, North-central Ethiopia, 2021
In contrary to this finding, a study by Banerjee, et al. (Banerjee A, et al., 2010) showed that there was no statistically significant difference in the incidence of hypotension between co-loading and preloading groups. This may be due to different study areas.
A study by Farid Z, et al. (Farid Z, et al., 2016) showed that there was no statistically significant difference in the incidence of hypotension after spinal anesthesia in preload and co-load groups which were different from the result of this study. They concluded that neither of the two techniques effectively prevents spinal-induced hypotension. The difference was, they used an extensively vasopressor when systolic BP dropped to 90 mm Hg.
Conclusion
This study indicated that the occurrence of hypotension was (77.1%) in preload group and (35.4%) in the co-load group. Therefore, crystalloid co-loading was better than preloading in the prevention of spinal anesthesia-induced hypotension in cesarean section mothers. Suspending surgery to supply preload of fluid may not be necessary. Secure large gage double IV line and co-load the mother while administering spinal anesthesia.
Acknowledgement
We would like to give credit to study participants, Debre Tabor University, and facilitators for their unreserved cooperation in the process of this study.
Ethical Consideration
The study was approved by The Ethics Committee of Debre Tabor University. Verbal consent was obtained from respondents and the data was collected confidentially. No personal identification was used on the questionnaire and no incentive or coercive measures were used.
Author Contribution
All authors had an equal contribution to this research and agreed for publication.
Data and Materials Availability
The dataset containing all the required data is found at the primary author who can be accessed with a justifiable request.
References
- Casey WF, Ankcorn C. Spinal anaesthesia-A practical guide. Update Anaesth. 2000.
- Olawin AM, Das JM. Spinal anesthesia. StatPearls. 2019.
- Naskar C, Dalai CK, Baidya TK, Sarkar N. Colloid versus crystalloid coload for the prevention of spinal aneasthesia induced hypotension of elective caesarean section. J drug deliv ther. 2013; 3(4): 54-61.
[Google scholar] [Pubmed]
- Farid Z, Mushtaq R, Ashraf S, Zaeem K. Comparative efficacy of crystalloid preloading and co-loading to prevent spinal anesthesia induced hypotension in elective caesarean section. Pak J Med Health Sci. 2016; 10(1): 42-45.
- Varshney RK, Kapoor K. A randomised prospective double blind study to compare the effects of fluid preloading and co-loading during spinal anaesthesia for caesarean delivery. Ann Int Med Dent Res. 2016; 2(1): 410. 4.
- Bajwa SJS, A Kulshrestha, Jindal R. Co-loading or pre-loading for prevention of hypotension after spinal anaesthesia! a therapeutic dilemma. Anesth: Essays res. 2013; 7(2): 155.
[Crossref] [Google scholar] [Pubmed]
- Lotfy ME, Moustafa AM, Feky EME, Mowafy IA. Colloid versus crystalloid co-load with spinal anesthesia during emergent cesarean section and their effect on hemodynamic changes. J Am Sci. 2014; 10(11): 158-163.
- Kilinç N, Deniz MN, Erhan E. Crystalloid preload versus crystalloid coload during spinal anesthesia for ureterorenoscopy: A randomized controlled trial. Ege Tıp Dergisi. 2020; 59(3): 181-187.
- Bhardwaj N, Thakur A, Sharma A, Kaushal S, Kumar V. Comparative study between crystalloid preloading and coloading for prevention of hypotension in elective cesarean section under spinal anesthesia in a secondary care hospital. Int J Res Rev. 2020; 7(7): 500-504.
- Ni HF, Liu HY, Zhang J, Peng K, Ji FH. Crystalloid coload reduced the incidence of hypotension in spinal anesthesia for cesarean delivery, when compared to crystalloid preload: A meta-analysis. BioMed research international. 2017.
[Crossref] [Google scholar] [Pubmed]
- Jackson R, Reid J, Thorburn J. Volume preloading is not essential to prevent spinal-induced hypotension at caesarean section. Br J Anaesth. 1995; 75(3): 262-265.
[Crossref] [Google scholar] [Pubmed]
- Kaufner L, Karekla A, Henkelmann A, Welfle S, Weizsacker KV, Hellmeyer L, et al. Crystalloid coloading vs. colloid coloading in elective Caesarean section: Postspinal hypotension and vasopressor consumption, a prospective, observational clinical trial. J Anesth. 2019; 33(1): 40-49.
[Crossref] [Google scholar] [Pubmed]
- Jain P, Valecha D. Comparative evaluation of preloading and coloading of crystalloids to prevent spinal induced hypotension in caesarean section. Int J Contemp Med. 2017; 4(2): 411-414.
- Teoh WH, Sia RT. Colloid preload versus coload for spinal anesthesia for cesarean delivery: The effects on maternal cardiac output. Anesth Analg. 2009; 108(5): 1592-1598.
- Oh AY, Hwang JW, Song IA, Kim MH, Ryu JH, Park HP, et al. Influence of the timing of administration of crystalloid on maternal hypotension during spinal anesthesia for cesarean delivery: Preload versus coload. BMC Anesthesiol. 2014; 14(1): 1-5.
- Banerjee A, Stocche RM, Angle P, Halpern SH. Preload or coload for spinal anesthesia for elective cesarean delivery: A meta-analysis. Can J Anaesth. 2010; 57(1): 24-31.
[Crossref] [Google scholar] [Pubmed]
- Jacob JJ, Williams A, Verghese M, Afzal L. Crystalloid preload versus crystalloid coload for parturients undergoing cesarean section under spinal anesthesia. J Obstet Anesth Crit Care. 2012; 2(1): 10.
- Parmar SB, Sheikh ANA, Shalu PS. A comparative study of preloading versus coloading of crystalloid to prevent spinal anaesthesia induced hypotension. J Evolution Med Dental Sci. 2012; 5(1): 746-753.
- Kumari S, George JK. Comparative study of hemodynamic effects of crystalloid preloading versus coloading during spinal anaesthesia for caesarean section. Int j res anal rev. 2017; 4(4): 343-348.
- Dyer RA, Farina Z, Joubert IA, Toit PD, Meyer M, Torr G, et al. Crystalloid preload versus rapid crystalloid administration after induction of spinal anaesthesia (coload) for elective caesarean section. Anaesth Intensive Care. 2004; 32(3): 351-357.
[Crossref] [Google scholar] [Pubmed]
- Idehen HF, Amadasun FE, Ekwere IT. Comparison of intravenous colloid and colloid. crystalloid combination in hypotension prophylaxis during spinal anesthesia for cesarean section. Niger J Clin Pract. 2014; 17(3): 309-313.
[Crossref] [Google scholar] [Pubmed]
- Olajumoke TO, Owojuyigbe AF, Afolayan JM. Preloading or coloading of crysralloid for prevention of hypotension during ceaserian section under spinal anaesthesia, a randomisd control trial. IOSR-J Med Dent Sci. 2017; 16(4): 140-142.
- Singhal A, Gupta A, Chittora S. Influence of the timing of administration of crystalloid on maternal hypotension during low dose spinal anesthesia for elective cesarean delivery: Preload versus coload. Int Arch Integr Med. 2019; 6(5): 16-21.
- Ohpasanon P, Chinachoti T, Sriswadi P, Srichu S. Prospective study of hypotension after spinal anesthesia for cesarean section at Siriraj hospital: Incidence and risk factors. J Med Assoc Thai. 2008; 91(5): 675.
[Google scholar] [Pubmed]
- Williamson W, Burks D, Pipkin J, Burkard JF, Osbome LA, Pelligrini JE. Effect of timing of fluid bolus on reduction of spinal-induced hypotension in patients undergoing elective cesarean delivery. AANA J. 2009; 77(2): 130-136.
- Kulkarni AG, O Asai, AS Tarkase. Comparative evaluation of co-loading versus preloading for prevention of post-spinal hypotension in elective caesarean section. Indian J Clin Anaesth. 2016; 3(3): 340-346.
- Khan M, Nisai W, Farooqi A, Ahmad N, Qaz S. Crystalloid coload: A better option than crystalloid pre-load for prevention of postspinal hypotension in elective caesarean section. Internet J Anesthesiol. 2013. 32: 1-8.
- Zhao PS. Supine hypotensive syndrome: A comprehensive review of literature. Transl Perioper and Pain Med. 2014; 1(2): 22-26.
Author Info
Metages Hunie1, Tadesse Wubishet1, Efrem Fenta1, Diriba Teshome1, Simegnew Kibret1, Tiruwork Desse2, Keder Essa1, Kumlachew Geta1*, Abebaw Misganaw1 and Dereje Zewdu32Department of Internal Medicine, Debre Tabor University, Debre Tabor, Ethiopia
3Department of Anesthesia, Wolkite University, Wolkite, Ethiopia
Citation: Geta K: The Effect of Preloading and Co-Loading in the Prevention of Hypotension among Mothers Who Underwent Cesarean Delivery under Spinal Anesthesia: A Prospective Cohort Study
Received: 07-Feb-2022 Accepted: 22-Feb-2022 Published: 01-Mar-2022, DOI: 10.31858/0975-8453.13.3.213-218
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






