Case Series - (2023) Volume 14, Issue 5
Abstract
The primary location of hydatidosis in the soft tissues is a rare situation, and the clinical picture is not very specific and consists of a painless swelling. The diagnosis is based on a combination of clinical, biological, radiological and anatomopathological findings. The biological work-up is essentially based on serological examinations using different immunological techniques; a negative serology does not however allow the diagnosis of hydatidosis to be excluded. Imaging is the most important step in the diagnosis, namely ultrasound and Computed Tomography (CT), but especially Magnetic Resonance Imaging (MRI) which is the most useful imaging tool in hydatid pathology of the soft tissues, through their results allow a better approach of this pathology, thus facilitating its management. Surgery remains the reference treatment, but a medical-surgical approach is now the rule. We have described in our study the cases of isolated hydatid cysts of the soft parts operated, with anatomo-pathological confirmation, by following the evolution of the patients since their consultation until the cure.
Keywords
Primary, Hydatid cyst, Unusual anatomical areas, Soft tissues
Introduction
Hydatidosis, or cystic echinococcosis, a name suggested by the World Health Organization (WHO) (Boussofara M, et al., 2005), is an anthropozoonosis caused by a parasitic taeniid-type tape-worm, Echinococcus granulosus, which is commonly transmitted from infected dogs, throw a hand to-mouth transfer of viable tapeworm eggs released in dog faeces (Tsukada H, et al., 2000). Hydatid cysts can form in any organ or tissue, but it’s most commonly found in the liver (75%) and lungs (15%) (Memis A, et al., 1999). Soft-tissue hydatidosis is a very rare location of the parasite, even in endemic regions, this location doesn’t exceed 3% (Garcia-Diez AI, et al., 2000). Clinical manifestations of soft-tissue hydatidosis are widely variable, depending on cyst location and its size, it rangs from a painless non-inflammatory swelling, to presentations that can mimic soft-tissue abscess or tumors (Cissé AM, et al., 2002; Daali M and Hssaida R, 2000).
Biological assessment using immunological tests is an essential step, however, negative serological tests doesn’t exclude the diagnosis of hydatidosis. Radiological exploration is an important diagnostic tool that allows a better approach in soft-tissue hydatidosis management using ultrasound, CT and especially MRI which is a performing imaging tool in case of soft-tissue involvement (El Haddad S, et al., 2011). Surgery is considered as the standard treatment for hydatid cyst, but a combination of medical and surgical management seems to be more often used (Örmeci N, et al., 2007). Prophylactic approach is an important tool that should be considered at every step of the epidemiological chain, especially in endemic regions (Agoumi A, 2003). We report in this article a case series of 4 patients presenting soft-tissue hydatidosis.
Case Presentation
Our work consisted on a descriptive retrospective study of 4 patients presenting soft-tissue hydatidosis, being followed in Trauma and Orthopedics department, in Mohammed VI University Hospital in Oujda, over a period of 6 years extending from November 2014 to September 2021.
We have included in our study, patients presenting soft-tissue hydatidosis with histological confirmation. Collecting epidemio-logical, clinical, radiological, and histological data was possible by accessing medical records from Trauma and Orthopedics departments (Medical Records Department), and Radiology department (Radiological information system and Carestream/PACS system for image acquisition). Radiological evaluation of soft-tissue hydatidosis in our patients was based on X-ray, ultrasound, CT-scan and MRI findings.
Medical information was collected and analyzed using a data collection sheet including epidemiological, clinical, radiological, pathological, therapeutic and evolutionary data from every patient.
Results
In our series, there is a higher incidence among females (75% of patients were females), and most of them came from rural areas (75% of patients). The main clinical symptom in our series correspond to a slow growing soft-tissue mass. The average delay for seeking a medical advice was about 45 months, with extremes extending from 1 to 10 years.
Clinical examination of our patients revealed a soft-tissue mass as the most predominant symptom, and variably associating other symptoms like pain and movement restriction (Figure 1) (Table 1).
| Clinical symptoms | No. of patients |
|---|---|
| Soft-tissue tumefaction | 4 |
| Pain | 1 |
| Restricted movements | 1 |
| Altered performance status | 0 |
Table 1: Common clinical symptoms seen in our series
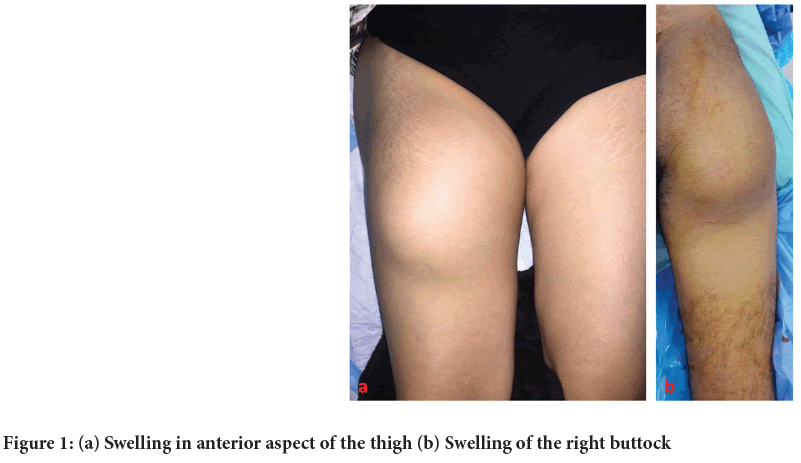
Figure 1: (a) Swelling in anterior aspect of the thigh (b) Swelling of the right buttock
Biological assessment has shown a normal blood count in all our patients, and a normal level of C-Reactive Protein (CRP), except for one patient. Serological tests were positive in only 2 patients.
An X-ray was performed in all patients showing variable results (Figure 2) (Table 2)
| Characteristics of the mass | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
|---|---|---|---|---|
| Location | Gluteal region | Gluteal region | Thigh | Subclavicular |
| Edges | Ill-defined | Well-defined | Well-defined | Well-defined |
| Consistency | Soft | Soft | Soft | Firm |
| Tenderness | Painful | Painless | Painless | Painless |
| Mobility | Mobile | Fixed | Mobile | Mobile |
| Local inflammation | Absent | Absent | Absent | Absent |
Table 2: Characteristics of the soft-tissue mass
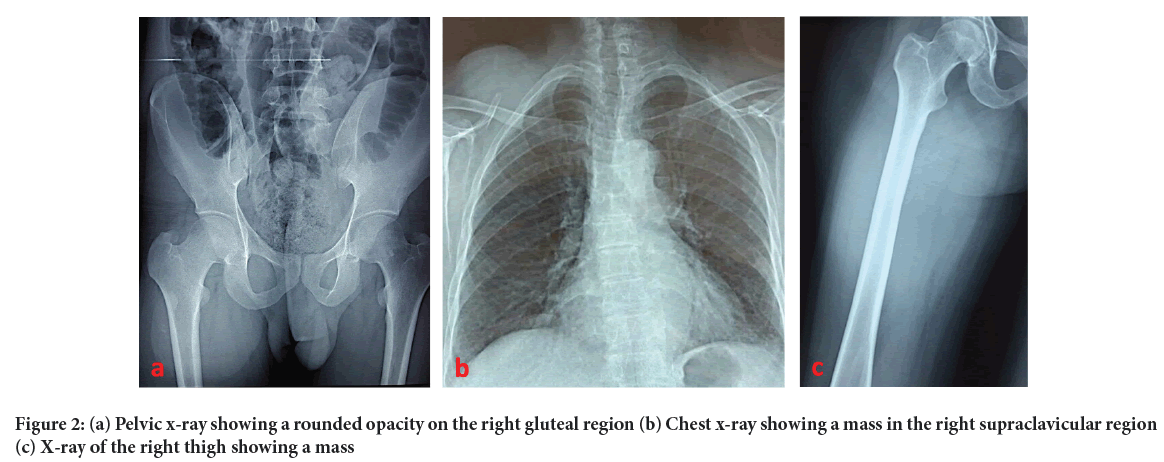
Figure 2: (a) Pelvic x-ray showing a rounded opacity on the right gluteal region (b) Chest x-ray showing a mass in the right supraclavicular region (c) X-ray of the right thigh showing a mass
• Patient 1-No evident lesion.
• Patient 2-No evident lesion.
• Patient 3-Round, well-defined homogenous radio-opacity on the upper 2/3rd of the thigh with no calcifications.
• Patient 4-Round, well-defined homogenous radio-opacity on the right subclavicular region, without any osteolytic lesions.
Two patients underwent a soft-tissue ultrasound, showing stage III hydatid cyst of GHARBI classification. An MRI was performed on all our patients (Figures 3-5), to reveal the exact location of the mass, its size, borders, shape, signal and to evaluate its relationship to adjacent structures. A chest x-ray with abdominal ultrasound were performed in all of our patients showing no secondary location of hydatid cyst.
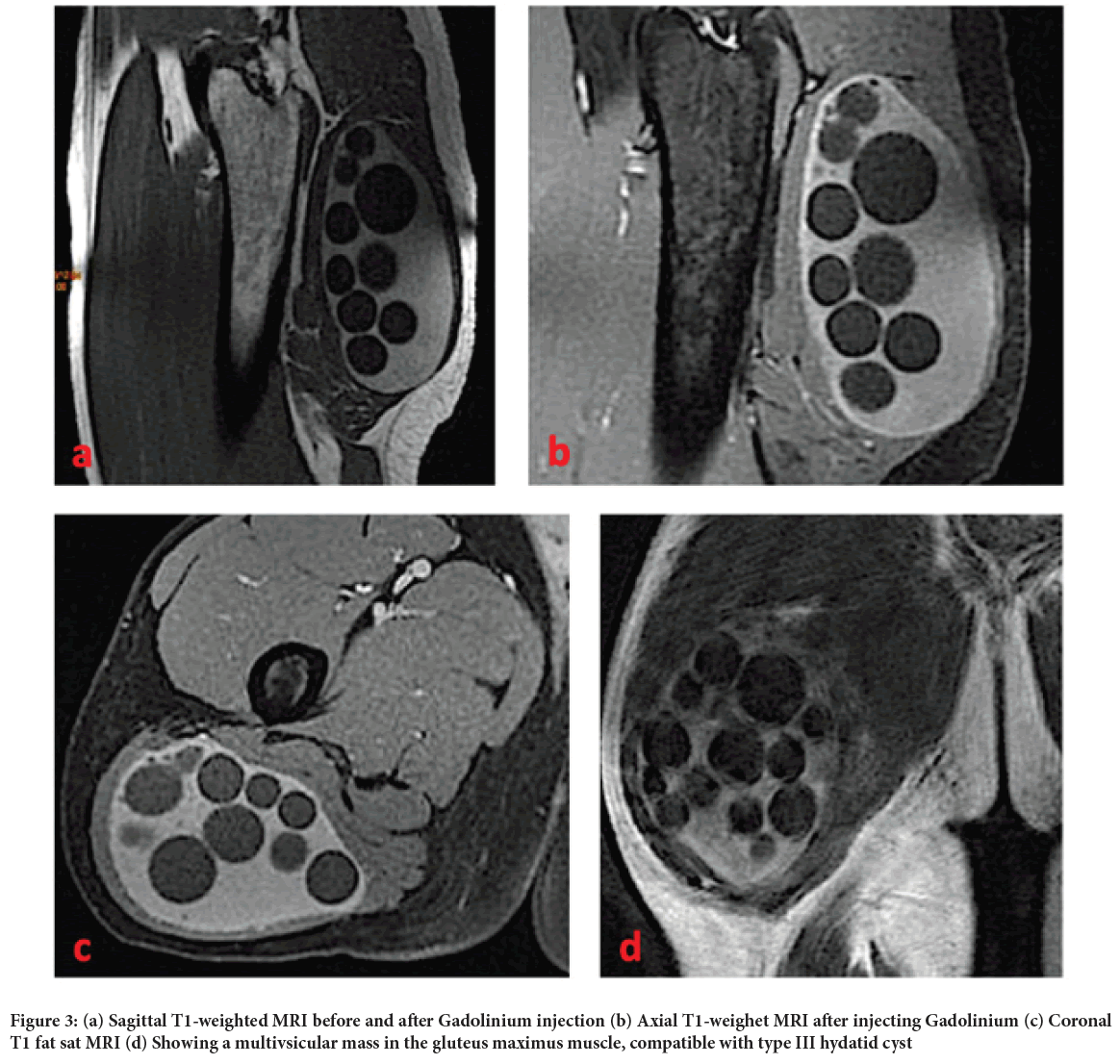
Figure 3: (a) Sagittal T1-weighted MRI before and after Gadolinium injection (b) Axial T1-weighet MRI after injecting Gadolinium (c) Coronal T1 fat sat MRI (d) Showing a multivsicular mass in the gluteus maximus muscle, compatible with type III hydatid cyst
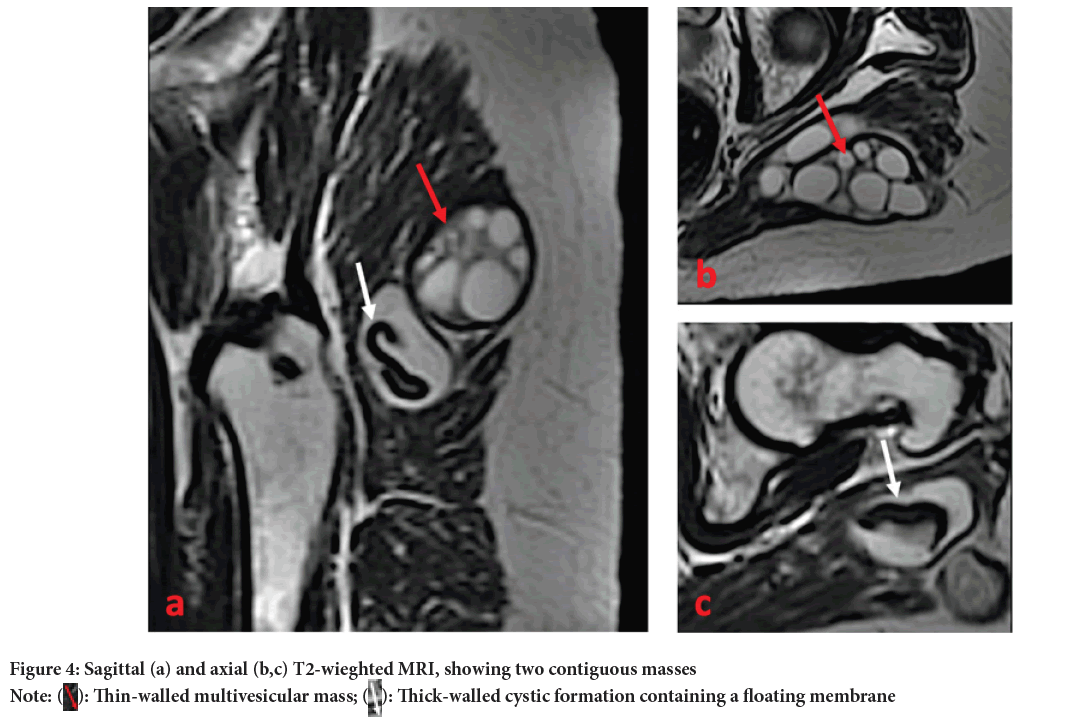
Figure 4: Sagittal (a) and axial (b,c) T2-wieghted MRI, showing two contiguous masses
Note:  Thin-walled multivesicular mass;
Thin-walled multivesicular mass;  Thick-walled cystic formation containing a floating membrane
Thick-walled cystic formation containing a floating membrane
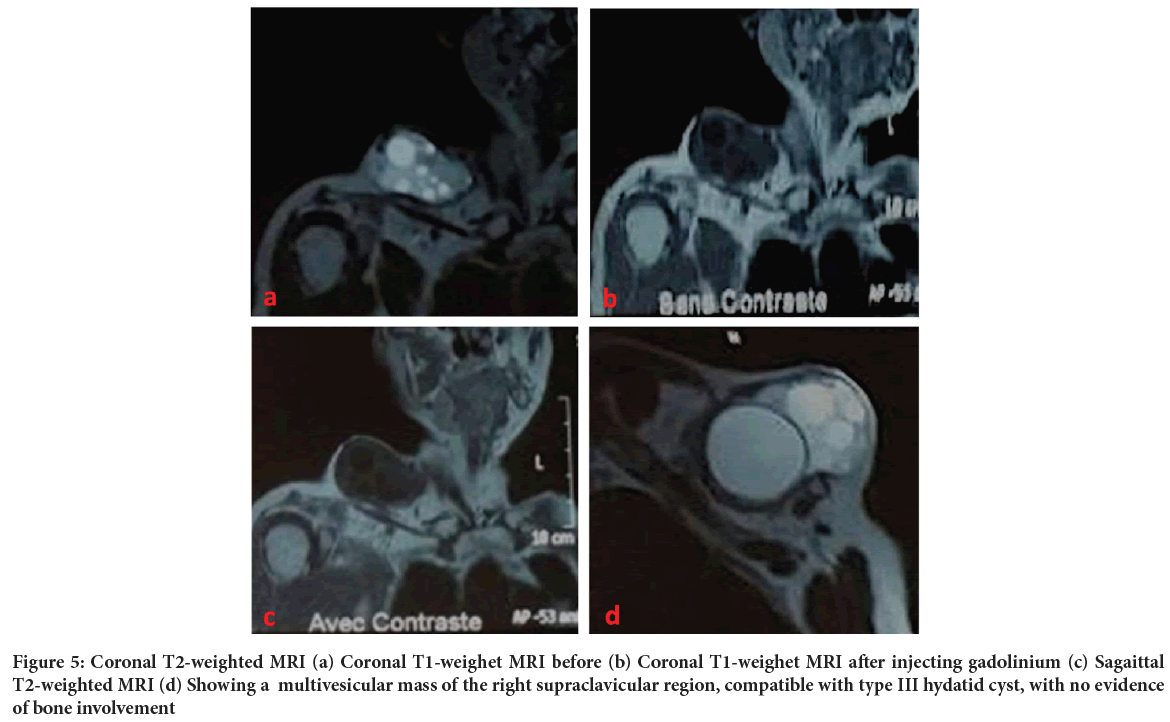
Figure 5: Coronal T2-weighted MRI (a) Coronal T1-weighet MRI before (b) Coronal T1-weighet MRI after injecting gadolinium (c) Sagaittal T2-weighted MRI (d) Showing a multivesicular mass of the right supraclavicular region, compatible with type III hydatid cyst, with no evidence of bone involvement
Gross aspect of hydatid cyst during surgery had a typical appearance, the mass showed numerous vesicles and pseudo-membranes, histological examination of the mass revealed a lamellated layer confirming the diagnosis of hydatid cyst (Table 3) (Figure 6).
| Case | MRI | Surgical exploration | Histology |
|---|---|---|---|
| Patient 1 | Type II and III hydatid cyst | •White mass •Endogenous daughter cyst |
Hydatid cyst |
| Patient 2 | Type III hydatid cyst | •Firm mass •Endogenous daughter cyst |
Hydatid cyst |
| Patient 3 | Type III hydatid cyst | •White mass •Endogenous daughter cyst |
Hydatid cyst |
| Patient 4 | Type III hydatid cyst | Endogenous daughter cyst | Hydatid cyst |
Table 3: Correlation between radiological, surgical and histological findings
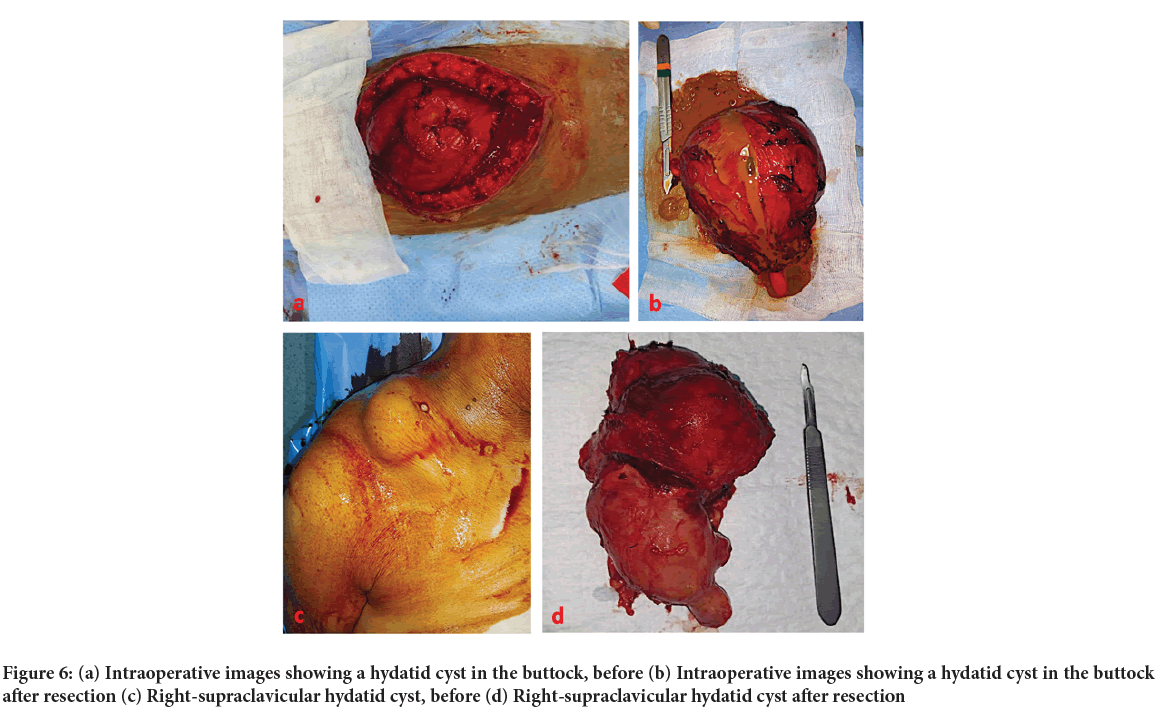
Figure 6: (a) Intraoperative images showing a hydatid cyst in the buttock, before (b) Intraoperative images showing a hydatid cyst in the buttock after resection (c) Right-supraclavicular hydatid cyst, before (d) Right-supraclavicular hydatid cyst after resection
In post-operative phase only one patient has presented vomiting 6 months after surgery, a reason why a thoraco-abdominopelvic CT scan was performed showing no signs of local recurrence, no other complications have been reported in our series and none of our patients had a recurrence so far (Figure 7).
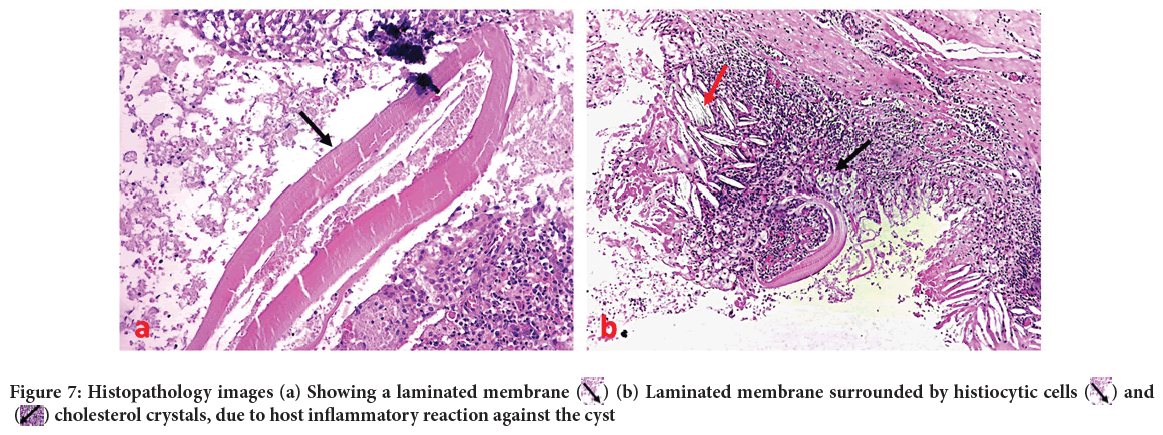
Figure 7: Histopathology images (a) Showing a laminated membrane  (b) Laminated membrane surrounded by histiocytic cells
(b) Laminated membrane surrounded by histiocytic cells  and
and  cholesterol crystals, due to host inflammatory reaction against the cyst
cholesterol crystals, due to host inflammatory reaction against the cyst
In our series, there was a correlation between radiological, histological and surgical findings.
Discussion
Human hydatid cyst is an anthropozoonosis linked to the development in humans of Echinococcus granulosus larvae. The parasitic cycle usually involves two hosts, dogs or wild canids as definitive hosts, and an intermediate host most commonly sheep, goats, cattle, equines, suids or camels (Pedrosa I, et al., 2000). Muscle hydatidosis is rather a rare location, even in endemic regions it accounts for 1% to 5% (Mekki RA, et al., 2005; Bennis A and Maazouzi W, 2001).
Patients included in our study were aged from 29 years to 78 years, with a median age of around 55 years. Several studies have reported high prevalence in young adults, as reported in Oğur HU, et al., 2009 study, where the average age reported was 39.4 years.
Several authors have reported that the majority of cases were females (Bel-lil S, et al., 2009; Habboubi K, et al., 2016), the same observation has been reported in Morocco between 1980 and 1992, where 75.4% of reported cases were females, against 24.6% of males. This is probably linked to agricultural tasks and daily handling of vegetables more often done by women. This predominance of infection in females has also been reported in other countries. In our study we report a higher incidence in women as well, 75% of females against 25% of males.
Most patients reported in literature have rural origins (Hlili F, et al., 2011; Zian D, 1998). In our study 75% of our patients come from rural areas. None of them had a previous history or second location of hydatid cyst, which confirms the primary involvement of soft-tissue. The main risk factor related to hydatidosis is a previous contact with dogs, weather direct or indirect (feces), it is found in 54.8% (DAALI series) and 82.7% (HLILI series) of hydatidosis cases (Hlili F, et al., 2011). In our study 80% of patients have had a previous contact with dogs.
In this study no hyper-eosinophilia has been observed. In Aït-Ammar N, et al., 2016 and Al Alami N, 2020 studies, hyper-eosinophilia was noted in only 10% of patients. CRP was elevated in only one of our patients, which had suggested a cyst infection. All our patients had a serological test using Indirect Hemagglutination Assay (IHA) which confirmed seropositivity in two of them.
Management of muscular hydatidosis is based on a combination of medical and surgical approach, associating cyst excision and drug therapy using Albendazol; antibiotics are usually used in case of cyst superinfection (Zian D, 1998). Some studies report benefits of using formalin, alcohol, silver nitrate (as a scolicidal agent) and a hypertonic saline solution to prevent recurrence and disease spreading (Aït-Ammar N, et al., 2016). In our series, all patients underwent a conservative surgical excision of the cyst, abundant washing with saline solution and hydrogen peroxide with preservation of adjacent healthy soft-tissue, then, they received an antiparasitic treatment based on Albendazol for 28 days (1 cycle), followed by a 14-day drug-free interval, for a total of 3 cycles; liver function and complete blood count were constantly monitored during treatment.
Conclusion
Hydatid disease is a frequent endemic parasitic infection in Morocco as well as in most African countries, primary soft-tissue and specifically muscular location of hydatid cyst is an uncommon situation, occasionally such locations can give rise to many complications due to compression of vascular or nervous structures, which can represent a challenging operative situation, requiring a very careful surgical intervention that aims to remove the mass without bringing any damage to adjacent neurovascular bundles. Interventional radiology could be a useful tool in that situation allowing a percutaneous drainage of the cyst without the need for an invasive procedure.
Authors' Contributions
Adnane Lachkar, Hicham Yacoubi and Najib Abdeljaouad did the surgery. Samir Ben Salah, Ayman Benabdellah drafted the documents for the ethics vote. Samir Ben Salah designed the study, developed the questionnaire, treated the data, did the statistics, and then drafted the manuscript, tables and figures. All authors read and approved the final manuscript.
Ethical Approval and Consent to Participate
Ethical approval was not needed in view of the retrospective and observational type of our study.
Consent for Publication
A written consent signed by all patients was obtained authorizing the use of their medical data in the scientific research and for publication on open access.
Availability of Data and Materials
The collection of data necessary to accomplish this work is facilitated by our computerized system of archiving medical records and the evolution of patients and their final results. Due to the sensitivity of the raw data, all data are available from the first author on request.
References
- Boussofara M, Sallem MR, Raucoules-Aimé M. Anesthésie pour chirurgie du kyste hydatique du foie. EMC-Anesth Reanim. 2005; 2(2): 132-140.
- Tsukada H, Morishima Y, Nonaka N, Oku Y, Kamiya M. Preliminary study of the role of red foxes in Echinococcus multilocularis transmission in the urban area of Sapporo, Japan. Parasitology. 2000; 120(4): 423-428.
[Crossref] [Google Scholar] [PubMed]
- Memis A, Arkun R, Bilgen I, Ustun EE. Primary soft tissue hydatid disease: Report of two cases with MRI characteristics. Eur Radiol. 1999; 9: 1101-1113.
[Crossref] [Google Scholar] [PubMed]
- Garcia-Diez AI, Ros Mendoza LH, Villacampa VM, Cozar M, Fuertes MI. MRI evaluation of soft tissue hydatid disease. Eur Radiol. 2000; 10: 462-466.
[Crossref] [Google Scholar] [PubMed]
- Cissé AM, Nassar I, Hammani L, Dafiri R, Imani F. Hydatidose primitive et étendue de la cuisse: Aspect radiologique inhabituel. Journal de radiologie. 2002; 83(11): 1778-1780.
- Daali M, Hssaida R. L'hydatidose musculaire: 15 cas. La Presse médicale (1983). 2000; 29(21): 1166-1169.
- El Haddad S, Radouane B, Akjouj S, Chaouir S, Semlali S. Liver hydatid cyst rupture in the biliary tract: Diagnosis using CT and MRI. J Africain d'Hépato-Gastroentérol. 2011: 236-241.
- Örmeci N, Idilman R, Akyar S, Palabıyıkoğlu M, Çoban S, Erdem H, et al. Hydatid cysts in muscle: A modified percutaneous treatment approach. Int J Infect Dis. 2007; 11(3): 204-208.
[Crossref] [Google Scholar] [PubMed]
- Agoumi A. Précis de parasitologie médicale. Editions Horizons Internationales. 2003.
- Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: Radiologic and pathologic features and complications. Radiographics. 2000; 20(3): 795-817.
[Crossref] [Google Scholar] [PubMed]
- Mekki RA, Souei MM, Allani M, Bahri M, Arifa N, Gharbi HJ, et al. Kyste hydatique des tissus mous: Apport de l’IRM (À propos de trois observations). Journal de Radiologie. 2005; 86(4): 421-5.
- Bennis A, Maazouzi W. Kyste hydatique du coeur. Rabat: Dar Nachr Al Maarifa. 2001: 15-26.
- Bellil S, Limaiem F, Bellil K, Chelly I, Mekni A, Haouet S, et al. Épidémiologie des kystes hydatiques extrapulmonaires: 265 cas en Tunisie. Med Mal Infect. 2009; 39(5): 341-343.
[Crossref] [Google Scholar] [PubMed]
- Oğur HU, Kapukaya R, Külahçı Ö, Yılmaz C, Yüce K, Tuhanioğlu Ü. Evaluation of radiologic diagnostic criteria and treatment options in skeletal muscle hydatid cysts. J Orthop Surg. 2019; 27(3): 2309499019881219.
[Crossref] [Google Scholar] [PubMed]
- Habboubi K, Kedous MA, Lahmar AA, Miladi M, Annabi H, Mbarek M. Le kyste hydatique des parties molles. Rev du Rhum. 2016; 83: A289-290.
- Hlili F, Benelkhaiat R, Finech B. Les complications du kyste hydatique Les complications du kyste hydatique du foie: À propos de 75 cas. 2011.
- Zian D. Traitement chirurgical des kystes hydatiques du foie à l’hôpital civil de Tétouan (Doctoral dissertation, Thèse de médecine). 1998.
- Aït-Ammar N, Prigent G, Zehou O, Le Mouel S, Chader H, Botterel F. Hydatidose musculaire primitive: À propos de 3 cas. Presse Med. 2016; 45(2): 258-261.
- Al Alami N. Hydatidose musculaire a propos de 20 cas avec revue de la litterature. 2020.
Author Info
Samir Ben Salah1,2*, Ayman Benabdellah1,2, Nadir Miry1,2, Najib Abdeljaouad1,2, Adnane Lachkar1,2 and Hicham Yacoubi1,22Orthopedic Trauma Department, Mohammed Ist University, Oujda, Morocco
Received: 27-Apr-2023 Accepted: 22-May-2023 Published: 29-May-2023, DOI: 10.31858/0975-8453.14.5.336-342
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






