Research Article - (2022) Volume 13, Issue 7
Abstract
Objective: Renal Biopsy is necessary in the assessment of renal diseases as it provides the histopathological diagnosis in the field of nephrology. Pattern varies with demography. Our study is done in one of the tertiary care centers in North India.
Materials and methods: Patients who underwent renal biopsy during the period from September 2019 to December 2020 were retrospectively reviewed. All biopsy specimens were examined by the same pathologist with light and immunofluorescence microscopy. Electron microscopic analysis was performed only in selected cases.
Results: Out of 116 patients, 48 are male and 68 are females. Primary glomerular diseases were the most common diagnosis. The overall most common indication for renal biopsy was Nephrotic Syndrome (45%) followed by Acute Kidney Injury (25%). The most common pathology was Infection Related Glomerulonephritis (18.10%) and least was immune complex mediated Glomerulonephritis (0.86%).
Conclusion: Our study gives an insight into the epidemiology of the renal disease in North India. Our study corresponds to the distribution pattern described in other North Indian states.
Keywords
Renal biopsy, Renal diseases, Tertiary center, Glomerulonephritis
Introduction
Renal Biopsy was first performed more than a century ago. It is still an essential tool in the diagnosis and treatment for several primary and secondary glomerular diseases. There are various presentation of glomerular diseases and renal biopsy is an important tool in its assessment because histopathological diagnosis is an essential part of evidence-based practice in nephrology. It can guide in deciding therapeutic options and can be of prognostic value. Pattern of Biopsy Proven Renal Diseases (BPRD) varies with time and geographical region (Prasad N, et al., 2015). A review of the renal biopsy data can give idea about the spectrum of renal diseases and its epidemiology data in our community. We conducted the present study to report the spectrum of BPRD from a tertiary care center in North India and comparing it with previous other studies to see the changing trend.
Aim
The aim of this work is to study the spectrum of Biopsy Proven Renal Disease (BPRD) in our center and analyze its trend with previous studies. There are only limited studies from Indian centers and there is a great variation when compared globally.
Materials and Methods
The records of the all patients who underwent renal biopsy in our hospital during the period September 2019 to December 2020 were retrospectively reviewed. The patients detail and laboratory investigation reports were obtained. Inadequate biopsy and renal allograft biopsy were excluded. All the biopsies were performed under ultrasound guidance using Bard Max-Core disposable core biopsy instrument. All the biopsies were analyzed by light microscopy using hematoxylin and eosin, periodic acid-Schiff, Jone's silver methenamine and Gomori 's trichrome stains and immunofluorescence studies were performed using antihuman IgG, IgA, IgM, C3, C1q, and kappa and lambda light chains (Werner T, et al., 2009). The diagnosis was made as per standard diagnostic criteria for each disease. The indications for renal biopsy were categorized as: Nephrotic Syndrome (NS) defined as proteinuria >3.5 gram/24 hours and serum albumin <2.5 gram/ dl (Chang JH, et al., 2009) (Figure 1). Acute Kidney Injury (AKI) defined as rapid and usually reversible decline in Glomerular Filtration Rate (GFR) and Kidney Disease Improving Global Outcomes (KDIGO) 2012 criteria is used to define it (Lameire NH, et al., 2013). Rapidly Progressing Renal Failure (RPRF) is defined as the deterioration in GFR with azotemia, over a period of few days, with radiologically normal sized kidneys (Bhowmik D, et al., 2011; Aatif T, et al., 2012). Asymptomatic Urinary Abnormality (AUA) is defined as non-nephrotic range proteinuria <3.5 gram/24 hour and hematuria defined as ≥ 3 red cells per high power field (Chang JH, et al., 2009; Aatif T, et al., 2012). As per NKF (National Kidney Foundation) KDOQI Guidelines, Chronic Kidney Disease (CKD) defined as either a kidney damage (structural or functional abnormalities) or GFR<60 mL/min/1.73 m2 for ≥ 3 months (Levey AS, et al., 2005). Histological categories include Glomerulonephritis (GN), Minimal Change Disease (MCD), Membranous Nephropathy (MN), Membrano-Proliferative Glomerulonephritis (MPGN), Infection Related Glomerulonephritis (IRGN), C3 Glomerulo Nephritis (C3GN), Anti Glomerulo Basement Membrane disease (Anti GBM ds), Pauci Immune Glomerulonephritis (PIG), Focal and Segmental Glomerulonephritis (FSGS), Chronic Glomerulonephritis (CGN), IgA Nephropathy (IgAN), Diabetic Nephropathy (DN), Lupus Nephritis (LN), Thrombotic Microangiopathy (TMA), Amyloidosis and End Stage Renal Disease (ESRD).
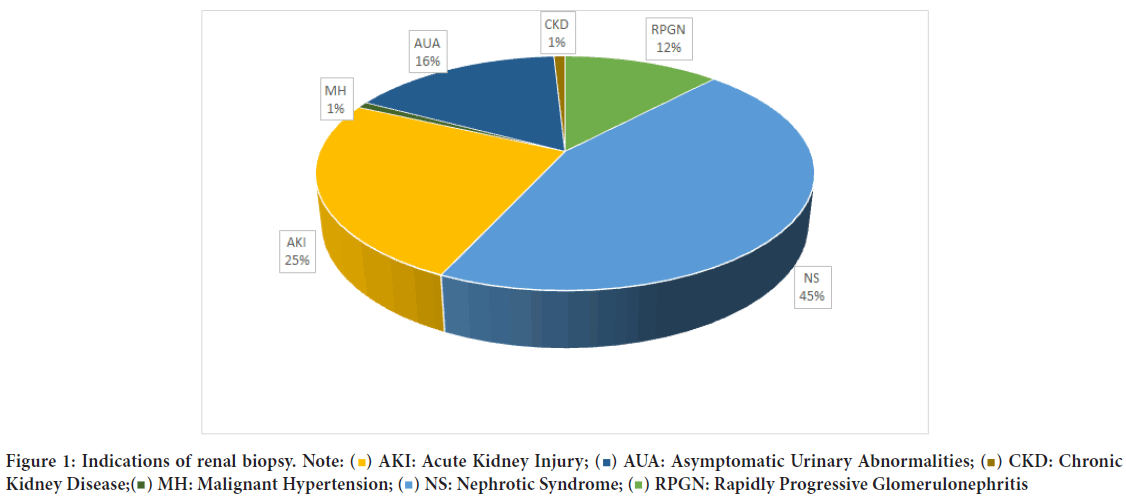
Figure 1: Indications of renal biopsy.

Simple descriptive statistics such as median and mean ± Standard Deviation (SD) were used for variables such as age, clinical and laboratory features. The percentages were used for categorical data.
Results
Out of 118 patients, 48 are male and 68 are females. 4 out of 38 males and 20 out of 68 females had secondary glomerular diseases. Among them 2 had Thrombotic Microangiopathy, 16 had Lupus Nephritis, 3 had Diabetic Nephropathy and 3 had acute pyelonephritis. Among the 118 patients 59 had presented with Nephrotic Syndrome, 29 had presented with AKI, 19 with Asymptomatic Urinary Abnormality, 14 with Rapidly Progressive Renal Failure, 1 with CKD and 1 with Microscopic hematuria. Male preponderance is seen in FSGS, Anti GBM disease, Immune complex mediated GN, IgA Nephropathy, acute tubular necrosis, and Amyloidosis. Female preponderance is seen with rest of the histopathological diagnosis (Table 1).
| Biopsy diagnosis | Gender | Total (n=116) | |
|---|---|---|---|
| Male (n=48) | Female (n=68) | ||
| Acute pyelonephritis | 1 (2.08%) | 2 (2.94%) | 3 (2.59%) |
| Acute tubular necrosis | 7 (14.58%) | 1 (1.47%) | 8 (6.90%) |
| Immune complex mediated Glomerulunephritis (GN) | 1 (2.08%) | - | 1 (0.86%) |
| Anti Glomerulo Basement Membrane (GBM) disease | 1 (2.08%) | 1 (1.47%) | 2 (1.72%) |
| Diabetic Nephropathy (DN) | 1 (2.08%) | 2 (2.94%) | 3 (2.59%) |
| Focal segmental glomerulosclerosis | 7(14.58%) | 8 (11.76%) | 15 (12.93%) |
| IgA Nephropathy (IgAN) | 5 (10.42%) | 5 (7.35%) | 10 (8.62%) |
| Infection Related Glomerulonephritis (IRG) | 9 (18.75%) | 12 (17.65%) | 21 (18.10%) |
| Lupus Nephritis (LN) | 2 (6.25%) | 14 (19.12%) | 16 (13.79%) |
| Minimal Change Disease (MCD) | 4 (8.33%) | 7 (10.29%) | 11 (9.48%) |
| Membranous Nephropathy (MN) | 3 (6.25%) | 10 (14.71%) | 13 (11.21%) |
| Membrano-Proliferative Glomerulonephritis (MPGN) type III | - | 1 (1.47%) | 1 (0.86%) |
| Pauci Immune Glomerulonephritis (PIG) | 1 (2.08%) | 2 (2.94%) | 3 (2.59%) |
| C3 Glomerulonephritis (C3GN) | 3 (6.25%) | 2 (2.94%) | 5 (4.31%) |
| Thrombotic Microangiopathy (TMA) | - | 2 (2.94%) | 2 (1.72%) |
| Amyloidosis | 2 (4.17%) | - | 2 (1.72%) |
Table 1: Gender distribution of various glomerular diseases
Infection Related Glomerulonephritis (18.10%) was the most common diagnosis among all the age groups followed by Lupus Nephritis (13.79%) and FSGS (12.93%). Among the age group <20 years of age MCD (21.88%) was the most common diagnosis followed by Infection Related Glomerulonephritis (18.75%). In the age group >40 years of age, again Infection Related Glomerulonephritis (25%) was the most common diagnosis followed by Membranous Nephropathy (15.63%). In the age group between 20 and 40, Lupus Nephritis (19.23%) is the most common diagnosis followed by FSGS (15.38%). Membranous Nephropathy and Minimal Change Disease commonly presented with serum creatinine <1.5 mg/dl. Serum creatinine value >3 mg/dl were most commonly associated with acute tubular necrosis, Immune complex mediated Glomerulonephritis and Pauci Immune Glomerulonephritis (Tables 2 and 3).
| Biopsy diagnosis | Age group (in years) | Total (n=116) | ||
|---|---|---|---|---|
| <20 (n=32) | 20-40 (n=52) | >40 (n=32) | ||
| Acute pyelonephritis | 1 (3.13%) | - | 2 (6.25%) | 3 (2.59%) |
| Acute tubular necrosis | 1 (3.13%) | 4 (7.69%) | 3 (9.38%) | 8 (6.90%) |
| Immune complex mediated Glomerulonephritis | - | - | 1 (3.13%) | 1 (0.86%) |
| Anti Glomerulo Basement Membrane (GBM) disease | 1 (3.13%) | 1 (1.92%) | - | 2 (1.72%) |
| Diabetic Nephropathy (DN) | 1 (3.13%) | 1 | 1 (3.13%) | 3 (2.59%) |
| Focal segmental glomerulosclerosis | 4 (12.50%) | 8 (15.38%) | 3 (9.38%) | 15 (12.93%) |
| IgA Nephropathy | 4 (12.50%) | 4 (7.69%) | 2 (6.25%) | 10 (8.62%) |
| Infection Related Glomerulonephritis | 6 (18.75%) | 7 (13.46%) | 8 (25%) | 21 (18.10%) |
| Lupus Nephritis | 4 (12.50%) | 10 (19.23%) | 2 (6.25%) | 16 (13.79%) |
| Minimal Change Disease | 7 (21.88%) | 3 (5.77%) | 1 (3.13%) | 11 (9.48%) |
| Membranous Nephropathy | 1 (3.13%) | 7 (13.46%) | 5 (15.63%) | 13 (11.21%) |
| Membrano-Proliferative Glomerulonephritis (MPGN) type III | - | 1 (1.92%) | - | 1 (0.86%) |
| Pauci Immune Glomerulonephritis | 1 (3.13%) | 1 (1.92%) | 1 (3.13%) | 3 (2.59%) |
| C3 Glomerulonephritis | 1 (3.13%) | 3 (5.77%) | 1 (3.13%) | 5 (4.31%) |
| Thrombotic Microangiopathy | - | - | 2 (6.25%) | 2 (1.72%) |
| Amyloidosis | - | 2 (3.85%) | - | 2 (1.72%) |
Table 2: Distribution of glomerular diseases according to age
| Biopsy diagnosis | Creatinine level (mg/dL) | Total (n=116) | ||
|---|---|---|---|---|
| <1.5 (n=60) | 1.5-3.0 (n=25) | >3.0 (n=31) | ||
| Acute pyelonephritis | 1 (1.67%) | 1 (4%) | 1 (3.23%) | 3 (2.59%) |
| Acute tubular necrosis | - | 3 (12%) | 5 (16.13%) | 8 (6.90%) |
| Immune complex mediated Glomerulonephritis | - | - | 1 (3.23%) | 1 (0.86%) |
| Anti Glomerulo Basement Membrane (GBM) disease | - | - | 2 (6.45%) | 2 (1.72%) |
| Diabetic Nephropathy | 1 (1.67%) | 1 (4%) | 1 (3.23%) | 3 (2.59%) |
| Focal segmental glomerulosclerosis | 10 (16.67%) | 2 (8%) | 3 (9.68%) | 15 (12.93%) |
| IgA Nephropathy | 6 (10%) | 0 | 4 (12.90%) | 10 (8.62%) |
| Infection Related Glomerulonephritis | 8 (13.33%) | 10 (40%) | 3 (9.68%) | 21 (18.10%) |
| Lupus Nephritis | 10 (16.67%) | 2 (8%) | 4 (12.90%) | 16 (13.79%) |
| Minimal Change Disease | 10 (16.67%) | 1 (4%) | - | 11 (9.48%) |
| Membranous Nephropathy | 12 (20%) | 1 (4%) | - | 13 (11.21%) |
| Membrano-Proliferative Glomerulonephritis (MPGN) type III | - | - | 1(3.23%) | 1 (0.86%) |
| Pauci Immune Glomerulonephritis | - | - | 3 (9.68%) | 3 (2.59%) |
| C3 Glomerulonephritis | 1 (1.67%) | 2 (8%) | 2 (6.45%) | 5 (4.31%) |
| Thrombotic Microangiopathy | - | 1 (4%) | 1 (3.23%) | 2 (1.72%) |
| Amyloidosis | 1 (1.67%) | 1 (4%) | 0 | 2 (1.72%) |
Table 3: Comparison between creatinine level and biopsy proven renal disease
Discussion
In our study, 118 patients with Biopsy Proven Renal Disease were retrospectively analyzed from our center. Primary glomerular disease constituted to about 70.4% and secondary glomerular diseases constituted to about 20.6%.
Primary glomerular disease is the most common cause of Biopsy Proven Renal Disease in our study correlating with majority of studies worldwide (Haas M, et al., 1997). The most common indication for renal biopsy was Nephrotic Syndrome accounting for 45% which is similar to most of the
studies done worldwide and also in India (Aatif T, et al., 2012; Naumovic R, et al., 2009; Polito MG, et al., 2010; Mubarak M, et al., 2011; Narasimhan B, et al., 2006). The most common causes of Nephrotic Syndrome in adults and children were Membranous Nephropathy and Minimal Change Disease respectively in our study which is similar to majority of the studies worldwide (Ferri FF, 2017). Literature shows that Membranous Nephropathy as the most common causes of Nephrotic Syndrome in adult (Naumovic R, et al., 2009; Aatif T, et al., 2012) and it was the most common cause of Nephrotic Syndrome in patients aged more than 20 years of age in our study.
There is a worldwide increase in the incidence of FSGS in recent times (Lameire NH, et al., 2013; Polito MG, et al., 2010; Mubarak M, et al., 2011; Alwahaibi NY, et al., 2013). This is also reflected in our study as FSGS was the most common cause of Nephrotic Syndrome among all the age groups followed by MN and MCD.
Even though IgA Nephropathy is considered as the most common cause of the glomerular disease worldwide, it came only sixth in the incidence of primary glomerular disease in our study (8.62%). This is also in concurrence with other Indian studies (Mubarak M, et al., 2011; Alwahaibi NY, et al., 2013; Narasimhan B, et al., 2006). Among the secondary glomerular diseases, Lupus Nephritis was the most common cause (13.79%) followed by Diabetic Nephropathy and Thrombotic Microangiopathy. This is similar to many western studies (Chang JH, et al., 2009; Aatif T, et al., 2012; Das U, et al., 2011; Al Arrayed A, et al., 2004; Polito MG, et al., 2010).
Comparing our study with Narasimhan B, et al. done at 2006 (Narasimhan B, et al., 2006), the most common indication for biopsy was Nephrotic Syndrome and most of the lesions were of primary glomerular diseases, which was similar to our study. But the most common diagnosis in their study was mesangioproliferative Glomerulonephritis followed by FSGS, with does not coincide with our study.
In the study done by Das U, et al. done at 2011, which analyzed distribution of biopsy proven disease in a tertiary care center in south India, the most common indication for biopsy was Nephrotic Syndrome followed by Acute kidney disease (Alwahaibi NY, et al., 2013). Primary glomerular diseases were more common indication for biopsy which is similar to our study. The most common cause of primary glomerular disease was MCD in their study but it was IRGN in our study. The most common cause of secondary glomerular disease was Lupus Nephritis which is also similar to our study (Table 4). Kazi JI, et al. studied 316 Biopsy Proven Renal Diseases, in which the most common lesions were FSGS than membraneous Glomerulonephritis. This correlates well with our study (Kazi JI, et al., 2009).
| Biopsy diagnosis | AKI (n=29) | AUA (n=19) | MH (n=1) | CKD (n=1) | NS (n=52) | RPGN (n=14) | Total (n=116) |
|---|---|---|---|---|---|---|---|
| Acute pyelonephritis | 2 (6.90%) | 1 (7.14%) | 3 (2.59%) | ||||
| Acute tubular necrosis | 4 (13.79%) | 1 (1.92%) | 3 (21.43%) | 8 (6.90%) | |||
| Immune complex Glomerulonephritis | 1 (3.45%) | 1 (0.86%) | |||||
| Anti Glomerulo Basement Membrane (GBM) disease | 2 (6.90%) | 2 (1.72%) | |||||
| Diabetic Nephropathy | 1 (3.45%) | 1 (5.26%) | 1 (1.92%) | 3 (2.59%) | |||
| Focal segmental glomerulosclerosis | 1 (3.45%) | 1 (5.26%) | 11 (21.15%) | 2 (14.29%) | 15 (12.93%) | ||
| IgA Nephropathy | 2 (6.90%) | 2 (10.53%) | 4 (7.69%) | 2 (14.29%) | 10 (8.62%) | ||
| Infection Related Glomerulonephritis | 6 (20.69%) | 4 (21.05%) | 1 (100%) | 10 (19.23%) | 21 (18.10%) | ||
| Lupus Nephritis | 6 (20.69%) | 5 (26.32%) | 3 (5.77%) | 2 (14.29%) | 16 (13.79%) | ||
| Minimal Change Disease | 2 (10.53%) | 9 (17.31%) | 11 (9.48%) | ||||
| Membranous Nephropathy | 4 (21.05%) | 8 (15.38%) | 1 (7.14%) | 13 (11.21%) | |||
| Membrano-Proliferative Glomerulonephritis (MPGN) type III | 1 (3.45%) | 1 (0.86%) | |||||
| Pauci Immune Glomerulonephritis | 3 (21.43%) | 3 (2.59%) | |||||
| C3 Glomerulonephritis | 2 (6.90%) | 3 (5.77%) | 5 (4.31%) | ||||
| Thrombotic microangipathy | 1 (3.45%) | 1 (100%) | 2 (1.72%) | ||||
| Amyloidosis | 2 (3.85%) | 2 (1.72%) |
Note: AKI: Acute Kidney Injury; AUA: Asymptomatic Urinary Abnormalities; CKD: Chronic Kidney Disease; MH: Malignant Hypertension; NS: Nephrotic Syndrome; RPGN: Rapidly Progressive Glomerulonephritis
Table 4: Pattern of Biopsy Proven Renal Diseases (BPRD)
Rapidly Progressive Renal Failure (RPRF) was found to be present in 14 patients (12.5%). Among the leading causes of Rapidly Progressive Renal Failure were the acute tubular necrosis (21.43%) and Pauci Immune Glomerulonephritis (21.43%). IgA Nephropathy, Lupus Nephritis and FSGS were the second most common causes of RPRF in our study, all accounting for 14.29% of all the primary glomerular diseases.
Over the past three decades the epidemiology of AKI has shifted and Infection Related Glomerulonephritis is now one of the leading causes of the AKI. This is also reflected in our study. In our study 29 patients (25%) had AKI. Among them, IRGN and LN (20.69%) were the leading causes of primary glomerular diseases causing AKI. Study done by Sujatha S and Ramprasad K in south India showed that acute interstitial nephritis is the most common cause of AKI followed by IRGN and Ischemia (Sujatha S and Ramprasad K, 2015).
Conclusion
Our epidemiological data represents that of a major tertiary care center in South India. And our observations are in concurrence with that of other studies done in South India. Large demographic variations of histopathological patterns of BPRD are seen across the world and within various parts of India. So, in order to have an accurate data, it is imperative to maintain a local renal biopsy registry.
References
- Prasad N, Kumar S, Manjunath R, Bhadauria D, Kaul A, Sharma RK, et al. Real-time ultrasound-guided percutaneous renal biopsy with needle guide by nephrologists decreases post-biopsy complications. Clin Kidney J. 2015; 8(2): 151-156.
[Crossref] [Google Scholar] [Pubmed]
- Werner T, Brodersen HP, Janssen U. Analysis of the spectrum of nephropathies over 24 years in a West German center based on native kidney biopsies. Med Klin. 2009; 104(10): 753-759.
[Crossref] [Google Scholar] [Pubmed]
- Chang JH, Kim DK, Kim HW, Park SY, Yoo TH, Kim BS, et al. Changing prevalence of glomerular diseases in Korean adults: A review of 20 years of experience. Nephrol Dial Transplant. 2009; 24(8): 2406-2410.
[Crossref] [Google Scholar] [Pubmed]
- Lameire NH, Bagga A, Cruz D, de Maeseneer J, Endre Z, Kellum JA, et al. Acute kidney injury: An increasing global concern. Lancet. 2013; 382(9887): 170-179.
[Crossref] [Google Scholar] [Pubmed]
- Bhowmik D, Sinha S, Gupt A, Tiwari SC, Agarwal SK. Clinical approach to rapidly progressive renal failure. J Assoc Physicians India. 2011; 59(2): 38-41. [Crossref]
[Google Scholar] [Pubmed]
- Aatif T, Maoujoud O, Montasser DI, Benyahia M, Oualim Z. Glomerular diseases in the Military Hospital of Morocco: Review of a single centre renal biopsy database on adults. Indian J Nephrol. 2012; 22(4): 257.
[Crossref] [Google Scholar] [Pubmed]
- Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005; 67(6): 2089-2100.
[Crossref] [Google Scholar] [Pubmed]
- Haas M, Meehan SM, Karrison TG, Spargo BH. Changing etiologies of unexplained adult nephrotic syndrome: A comparison of renal biopsy findings from 1976-1979 and 1995-1997. Am J Kidney Dis. 1997; 30(5): 621-631.
[Crossref] [Google Scholar] [Pubmed]
- Naumovic R, Pavlovic S, Stojkovic D, Basta-Jovanovic G, Nesic V. Renal biopsy registry from a single centre in Serbia: 20 years of experience. Nephrol Dial Transplant. 2009; 24(3): 877-885.
[Crossref] [Google Scholar] [Pubmed]
- Polito MG, de Moura LA, Kirsztajn GM. An overview on frequency of renal biopsy diagnosis in Brazil: Clinical and pathological patterns based on 9617 native kidney biopsies. Nephrol Dial Transplant. 2010; 25(2): 490-496.
[Crossref] [Google Scholar] [Pubmed]
- Mubarak M, Kazi JI, Naqvi R, Ahmed E, Akhter F, Naqvi SA, et al. Pattern of renal diseases observed in native renal biopsies in adults in a single centre in Pakistan. Nephrology. 2011; 16(1): 87-92.
[Crossref] [Google Scholar] [Pubmed]
- Narasimhan B, Chacko B, John GT, Korula A, Kirubakaran MG, Jacob CK. Characterization of kidney lesions in Indian adults: Towards a renal biopsy registry. J Nephrol. 2006; 19(2): 205-210.
[Google Scholar] [Pubmed]
- Ferri FF. Ferri's clinical advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. 2017.
- Alwahaibi NY, Alhabsi TA, Alrawahi SA. Pattern of glomerular diseases in Oman: A study based on light microscopy and immunofluorescence. Saudi J Kidney Dis Transpl. 2013; 24(2): 387.
[Crossref] [Google Scholar] [Pubmed]
- Das U, Dakshinamurty KV, Prayaga A. Pattern of biopsy-proven renal disease in a single center of south India: 19 years experience. Indian J Nephrol. 2011; 21(4): 250.
[Crossref] [Google Scholar] [Pubmed]
- Al Arrayed A, George SM, Malik AK, Al Arrayed S, Rajagopalan S, Sharqawi SE, et al. The spectrum of glomerular diseases in the Kingdom of Bahrain: An epidemiological study based on renal biopsy interpretation. Transplant Proc. 2004; 36(6): 1792-1795.
[Crossref] [Google Scholar] [Pubmed]
- Kazi JI, Mubarak M, Ahmed E, Akhter F, Naqvi SA, Rizvi SA. Spectrum of glomerulonephritides in adults with nephrotic syndrome in Pakistan. Clin Exp Nephrol. 2009; 13(1): 38-43.
[Crossref] [Google Scholar] [Pubmed]
- Sujatha S, Ramprasad K. Biopsy series of acute kidney injury from a tertiary care referral center in South India. J Nephropharmacol. 2015; 4(1): 43. [Crossref]
[Google Scholar] [Pubmed]
Author Info
Neha Saxena1, Robert James2, Nagisetti Phanindra Kumar3 and B Rajsekhar4*2Department of Medicine, Varun Arjun Medical College, Uttar Pradesh, India
3Department of Oncology, American oncology Institute, Andhra Pradesh, India
4Department of Pathology, Varun Arjun Medical College, Uttar Pradesh, India
Citation: Saxena N: The Spectrum of Biopsy Proven Renal Disease in a Tertiary Care Centre in North India
Received: 30-Jun-2022 Accepted: 22-Jul-2022 Published: 29-Jul-2022, DOI: 10.31858/0975-8453.13.7.487-491
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






