Case Study - (2023) Volume 14, Issue 6
Abstract
Introduction: The presence of suicidal ideation represents a challenge for clinicians, and it is essential to detect and treat it effectively to prevent the patient from taking his or her own life.
Case presentation: Two clinical cases will be described, a 74-year-old man and a 19-year-old woman suffering from schizophrenic spectrum disorder, manifesting suicidal ideation. The patients were treated effectively and without adverse effects with vortioxetine.
Conclusion: Vortioxetine has proven effective in treating suicidal ideation in patients with schizophrenic spectrum disorders.
Keywords
Schizophrenia, Hallucinations, Delusions, Vortioxetine
Introduction
Suicidal ideation is a multifaceted and complex psychopathological symptom changing in intensity and duration. As per the studies and reports on schizophrenic patients, it is observed that the lifetime prevalence of such thoughts was 34.5%, in comparison, point prevalence was 29.9% (Bai W, et al., 2021). However, a clear thought of self-harm was observed between 6.4% and 13% of patients (Bai W, et al., 2021) and among those only few patients continue to cause self-harm intentionally (Gliatto MF and Rai AK, 1999).
The term suicidal ideation refers to the presence of different selfharm or self-injury ideas due to some mental imbalance. It is unfortunate that no specific signs or symptoms have been identified that would allow the clinician to predict a self-harm event accurately. However, some psychopathological aspects, such as hopelessness, flat affect, insomnia, irritability and nihilistic delusions have been known to be associated with increased risk for negative thoughts (Harmer B, et al., 2023). Studies denote that patients with such negative ideations who are associated with delusions or hallucinations might show a 6-fold increased risk of self-harm respect to patients with negative symptoms such as abulia, alogia and social inhibition, who conversely have a reduced risk (Chapman CL, et al., 2015; Grover LE, et al., 2022). In addition, schizophrenic patients tend to show self-harm thoughts more frequently during periods of remission and in the early stages of psychosis, as they are often more prone to develop depressive episodes (Fawcett J, et al., 1993; Bornheimer LA, et al., 2021). Practically, those patients who do not seem to be straightforward to commit selfharm, are mostly managed as “outpatients”. However, self-harm ideas may persist despite drug treatment with antipsychotics which are used to manage positive or negative psychotic symptoms. In this paper, we will describe two clinical cases in which suicidal ideation were treated with vortioxetine. Vortioxetine is a multimodal antidepressant that, in addition to the classic mechanism of serotonin reuptake inhibition, acts as an antagonist, full and partial agonist of the serotonin receptors. Indirectly by acting on serotonergic receptors, it increases dopamine levels, noradrenaline, histamine and acetylcholine. It also modulates the neurotransmission of glutamatergic circuits.
Case Presentation
Case I
The first case concerns a 74-year-old man with residual schizophrenia. He had previously suffered from a productive form of schizophrenia with delusions of persecution, hallucinations and violent behavior. The patient had been regularly taking olanzapine 10 mg/bid for about ten years with adequate control of psychotic symptoms and he did not present organic medical problems. After a long period of remission, in which he had no longer raised delusions, hallucinations or disorganized behavior, he began to manifest apathy, complaints about his inability to remember and self-destruction thoughts. On the psychiatric examination, he appeared fairly cooperative and the speech was spontaneous but focused on some death issues. Thought content was within normal limits, while thought form seemed poor. The patient was oriented in time, space and person and the affect was flat.
The patient showed prevalent self-destruction ideas without however presenting his clear intension of self-harm. He stated that he would never harm himself, although the self-harm ideation was pervasive and persistent. He was administered the Suicidal Ideation Attribute Scale (SIDAS) (van Spijker BA, et al., 2014) and the score obtained was 42 (the range score is between 0-50, higher scores correspond to more severe symptomatology). He was also well supported by his wife and sons and was rarely left alone or with objects that could be used for self-harm as a precaution. Vortioxetine was used, starting at 5 mg daily and moving to 10 mg/day after a week. One month after the start of treatment, the patient reported a substantial clinical improvement with a reduction in wild thoughts of self-destruction and no longer complained of memory difficulties. Affect was more reactive and did not present psychotic symptoms such as delusions, hallucinations or violent behavior. He had improved and the score obtained at SIDAS had dropped to 24. After 12 months, the patient did not present with worsening self-harm ideation.
Case II
The other case concerns a young 19-year-old girl suffering from a schizoaffective disorder, in which the psychotic component was pretty compensated with the use of long-acting injectable Aripiprazole lauroxil. She was also taking Lithium Carbonate at 300 mg/bid. The last reported value was 0.35 and SIDAS (van Spijker BA, et al., 2014) score was 46.
The psychotic symptoms onset dates back to adolescence, characterized by depressive episodes and predominantly disorganized psychotic symptoms, a tendency to social withdrawal and relational difficulties. She was still in school, failed twice and failed to graduate.
She had many hobbies like music, writing and painting, but she did not care. She had prevailing and persistent ideas of self-harm and was forced to the hospital twice because of these ideas. On the psychiatric examination, she appeared uncooperative, mutated, thought and perception adequate and oriented in space, time and person. She had been treated with 150 mg sertraline a day with little benefit, although she complained of ideas of death. After one month of ineffective treatment with sertraline, she has been treated with Escitalopram 15 mg daily with poor results. Even with venlafaxine 225 mg/day, there was no improvement and the intension to cause self-harm persisted.
Given the various therapeutic failures, it was decided to treat the patient with 10 mg of vortioxetine. Within 8 weeks, self-destructive ideation was less pervasive and persistent and the patient felt relief at having freed herself from this onerous burden. SIDAS (van Spijker BA, et al., 2014) score was 30. She resumed her hobbies and she began singing again. Twelve months later, the improvement related to negative/self-harming thoughts persists.
Discussion
Although these two cases are different regarding sex, age and diagnosis, both share continuous and pervasive self-destruction ideas. The administration of vortioxetine 10 mg was effective in reducing self-destruction ideation without worsening the psychotic symptoms. While the antipsychotic clozapine has a well-documented effect in preventing self-harm in patients with schizophrenia (Meltzer HY, et al., 2003), data are beginning to emerge that have analyzed the effect of vortioxetine on self-harming in schizophrenia. A clinical trial investigating several studies ruled out that vortioxetine increases or induces self-injurious behavior (Mahableshwarkar AR, et al., 2020).
Suicidal ideation is a problem not to be underestimated in the schizophrenic patient and should be evaluated routinely in this category of patients. The risk of self-harm in schizophrenic patients indeed is 4.5 times higher than that for the general US population (Olfson M, et al., 2021). Identifying patients at risk and investigating the presence of self-harm thoughts in patients with schizophrenia should be a part of every psychiatric assessment to intervene early and avoid a negative outcome since the presence of negative thoughts in schizophrenic patients is a indication of future self-harming behavior (Funahashi T, et al., 2000). Treatment with vortioxetine is effective in countering negative thoughts with lasting efficacy and without worsening effects on psychotic symptoms. These clinical cases are limited to extending vortioxetine to all schizophrenic patients with self-harm ideation. Randomized placebo-controlled longitudinal studies would be needed to evaluate the efficacy of vortioxetine, tolerability and the absence of adverse effects on psychotic symptoms (Figure 1).
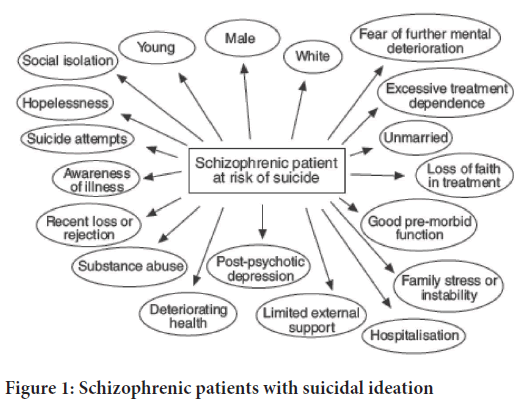
Figure 1: Schizophrenic patients with suicidal ideation
Vortioxetine is a multimodal agent that increases the release of serotonin, norepinephrine and acetylcholine mediated by blockade of the 5HT3 receptor and by agonism on the 5-hydroxytryptamine receptor 1A (5HT1A), 5HT1B, 5HT1D and 5HT7 receptors (Stahl SM, 2015). Some authors also described that vortioxetine acts as an antagonist of the 5HT7 receptor; indeed, sub chronic administration of vortioxetine tends to down-regulated 5HT7 receptor that determines the decrease of thalamocortical glutamate transmission (Okada M, et al., 2021). A hyper-connectivity between the thalamus and frontal regions was observed in schizophrenia and it is associated with the severity and course of schizophrenia (Abram SV, et al., 2022). Moreover, increased neuronal glutamate transporter expression that induces neuronal and glial cell loss in the dorsolateral prefrontal cortex has been associated with a higher risk of committing self-injurious acts (Powers B, et al., 2020).
Some scientific evidence has shown that adding vortioxetine to treatment with antipsychotics such as risperidone (Moazen-Zadeh E, et al., 2020) and clozapine improves both negative and positive symptoms (Bruno A, et al., 2020). However, care should be taken when using antidepressants as they may worsen delusions and hallucinations.
Vortioxetine effectively treated self-harm ideation in the two reported cases, without worsening psychotic symptoms and with no significant side effects.
Self-harm is a process that goes through several stages that begins with the presence of ideas of death, followed by negative thoughts in many cases and can end with the last step, which is the enactment of self-harming behavior (Pompili M, et al., 2007). Therefore, it should be mandatory to assess the presence of such negative thoughts and check for risk factors in patients with schizophrenia to prevent self-injurious conduct.
Conclusion
To date, these are the first cases reported in the literature describing the use of vortioxetine in patients with schizophrenic spectrum disorders who manifest self-harm ideation. The reported clinical cases although effectively and safely treated with vortioxetine, are by no means conclusive and have limited clinical value; nevertheless, given the magnitude of the problem, it would be of hope that randomized clinical trials would be conducted to test the efficacy of vortioxetine in the treatment of self-harm ideation.
References
- Bai W, Liu ZH, Jiang YY, Zhang QE, Rao WW, Cheung T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: A meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. 2021; 11(1): 552.
[Crossref] [Google Scholar] [Pubmed]
- Gliatto MF, Rai AK. Evaluation and treatment of patients with suicidal ideation. Am Fam Physician. 1999; 59(6): 1500.
[Google Scholar] [Pubmed]
- Harmer B, Lee S, Duong TvH, Saadabadi A. Suicidal ideation. Treasure Island (FL): StatPearls Publishing. 2023.
[Google Scholar] [Pubmed]
- Chapman CL, Mullin K, Ryan CJ, Kuffel A, Nielssen O, Large MM. Meta‐analysis of the association between suicidal ideation and later suicide among patients with either a schizophrenia spectrum psychosis or a mood disorder. Acta Psychiatr Scand. 2015; 131(3): 162-173.
[Crossref] [Google Scholar] [Pubmed]
- Grover LE, Jones R, Bass NJ, McQuillin A. The differential associations of positive and negative symptoms with suicidality. Schizophr Res. 2022;248:42-9.
[Crossref] [Google Scholar] [Pubmed]
- Fawcett J, Clark DC, Busch KA. Assessing and treating the patient at risk for suicide. Psychiatr Ann. 1993; 23(5): 244-255.
- Bornheimer LA, Wojtalik JA, Li J, Cobia D, Smith MJ. Suicidal ideation in first-episode psychosis: Considerations for depression, positive symptoms, clinical insight, and cognition. Schizophr Res. 2021; 228: 298-304.
[Crossref] [Google Scholar] [Pubmed]
- van Spijker BA, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, et al. The Suicidal Ideation Attributes Scale (SIDAS): Community‐based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav. 2014; 44(4): 408-419.
[Crossref] [Google Scholar] [Pubmed]
- Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia: International suicide prevention trial (InterSePT). Arch Gen Psychiatry. 2003; 60(1): 82-91.
[Crossref] [Google Scholar] [Pubmed]
- Mahableshwarkar AR, Affinito J, Reines EH, Xu J, Nomikos G, Jacobsen PL. Suicidal ideation and behavior in adults with major depressive disorder treated with vortioxetine: Post hoc pooled analyses of randomized, placebo-controlled, short-term and open-label, long-term extension trials. CNS Spectr. 2020; 25(3): 352-362.
[Crossref] [Google Scholar] [Pubmed]
- Olfson M, Stroup TS, Huang C, Wall MM, Crystal S, Gerhard T. Suicide risk in medicare patients with schizophrenia across the life span. JAMA Psychiatry. 2021; 78(8): 876-885.
[Crossref] [Google Scholar] [Pubmed]
- Funahashi T, Ibuki Y, Domon Y, Nishimura T, Akehashi D, Sugiura H. A clinical study on suicide among schizophrenics. Psychiatry Clin Neurosci. 2000; 54(2): 173-179.
[Crossref] [Google Scholar] [Pubmed]
- Stahl SM. Modes and nodes explain the mechanism of action of vortioxetine, a multimodal agent (MMA): Enhancing serotonin release by combining serotonin (5HT) transporter inhibition with actions at 5HT receptors (5HT1A, 5HT1B, 5HT1D, 5HT7 receptors). CNS Spectr. 2015; 20(2): 93-97.
[Crossref] [Google Scholar] [Pubmed]
- Okada M, Matsumoto R, Yamamoto Y, Fukuyama K. Effects of subchronic administrations of vortioxetine, lurasidone, and escitalopram on thalamocortical glutamatergic transmission associated with serotonin 5-HT7 receptor. Int J Mol Sci. 2021; 22(3): 1351.
[Crossref] [Google Scholar] [Pubmed]
- Abram SV, Roach BJ, Fryer SL, Calhoun VD, Preda A, van Erp TG, et al. Validation of ketamine as a pharmacological model of thalamic dysconnectivity across the illness course of schizophrenia. Mol Psychiatry. 2022; 27(5): 2448-2456.
[Crossref] [Google Scholar] [Pubmed]
- Powers B, Joyce C, Kleinman JE, Hyde TM, Ajilore O, Leow A, et al. Sex differences in the transcription of glutamate transporters in major depression and suicide. J Affect Disord. 2020; 277: 244-252.
[Crossref] [Google Scholar] [Pubmed]
- Moazen-Zadeh E, Bayanati S, Ziafat K, Rezaei F, Mesgarpour B, Akhondzadeh S. Vortioxetine as adjunctive therapy to risperidone for treatment of patients with chronic schizophrenia: A randomised, double-blind, placebo-controlled clinical trial. J Psychopharmacol. 2020; 34(5): 506-513.
[Crossref] [Google Scholar] [Pubmed]
- Bruno A, Zoccali RA, Troili GM, Scala L, Pandolfo G, Cedro C, et al. Vortioxetine on cognition in schizophrenia: A pilot study. J Clin Psychopharmacol. 2020; 40(4): 381-385.
[Crossref] [Google Scholar] [Pubmed]
- Pompili M, Amador XF, Girardi P, Harkavy-Friedman J, Harrow M, Kaplan K, et al. Suicide risk in schizophrenia: Learning from the past to change the future. Ann Gen Psychiatry. 2007; 6(1): 1-22.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Antonino Messina1,2*, Alessandro Rodolico1, Filippo Caraci3 and Maria Salvina Signorelli12Mental Health Department, University of Catania, Catania, Italy
3Department of Drug Sciences, University of Catania, Catania, Italy
Citation: Systematic Review Pharmacy Messina A: Vortioxetine in Patients with Schizophrenia and Suicidal Ideation
Received: 05-May-2023 Accepted: 02-Jun-2023 Published: 09-Jun-2023, DOI: 10.31858/0975-8453.14.6.393-395
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






